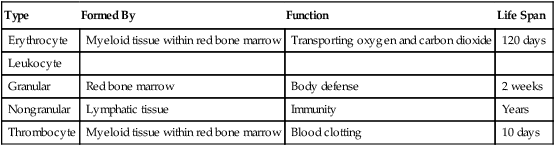
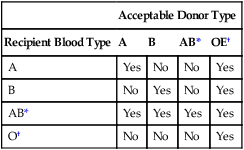
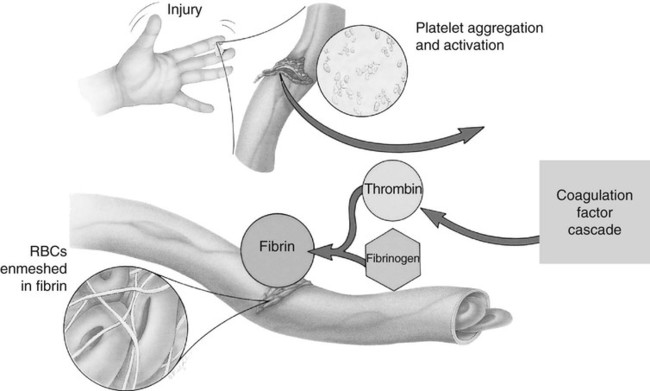
On completion of Chapter 9, the reader should be able to: • Identify the major constituents of blood and describe the function of each constituent. • Specify the various blood types. • Explain the role of the lymphatic system in terms of immunity. • Describe the pathogenesis, prognosis, and signs and symptoms of the disease processes discussed in this chapter. • Identify the various imaging modalities used in diagnosing hemopoietic disorders. Three basic types of blood cells—erythrocytes, leukocytes, and thrombocytes (Table 9-1)—make up the remaining 45% of the total blood volume. TABLE 9-1 The person with type O blood is considered the universal donor because this type does not contain any antigens and can be given to anyone regardless of the recipient’s blood type. The person with type AB blood is considered the universal recipient because this type of blood possesses both antigens, which enables the person to receive any type of blood (Table 9-2). In addition, the Rh blood factor should be considered. The Rh factor is termed such because it was first discovered in the blood of the rhesus monkey. Approximately 85% of the human population has this factor; these people are classified as Rh-positive. Individuals not possessing the Rh factor are Rh-negative. The Rh factor becomes a problem if an Rh-positive father transmits the Rh factor to a fetus carried by an Rh-negative mother. The first pregnancy generally progresses normally, but in subsequent pregnancies, the mother’s anti-Rh antibodies, made during the first pregnancy, attack the Rh-positive fetal blood. This scenario can be avoided by Rh-immunization of the mother before pregnancy. TABLE 9-2 The third major type of blood cells is the thrombocytes, or platelets. These cells are necessary for blood to clot properly and respond within seconds to initiate the coagulation process. Thrombocytes are also formed in the myeloid tissue within the red bone marrow and have a life span of approximately 10 days. The normal platelet count is 140,000 to 340,000 per cubic millimeter (mm3). Platelet activation is increased by an inflammatory response. Vascular damage results in a physiologic response to maintain homeostasis, including vasoconstriction, the development of a platelet plug, the activation of blood coagulation (thrombin), and the formation of a blood clot. This process is critical in preventing hemorrhage and is dependent on the availability of the proper number of platelets (Fig. 9-1).
Hemopoietic System
Anatomy and Physiology
Type
Formed By
Function
Life Span
Erythrocyte
Myeloid tissue within red bone marrow
Transporting oxygen and carbon dioxide
120 days
Leukocyte
Granular
Red bone marrow
Body defense
2 weeks
Nongranular
Lymphatic tissue
Immunity
Years
Thrombocyte
Myeloid tissue within red bone marrow
Blood clotting
10 days
Acceptable Donor Type
Recipient Blood Type
A
B
AB*
OE†
A
Yes
No
No
Yes
B
No
Yes
No
Yes
AB*
Yes
Yes
Yes
Yes
O†
No
No
No
Yes
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine