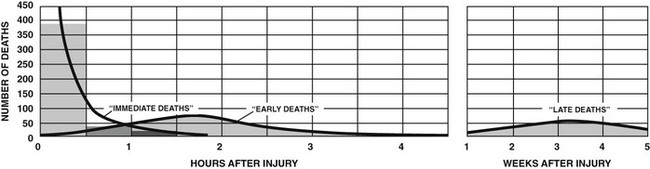
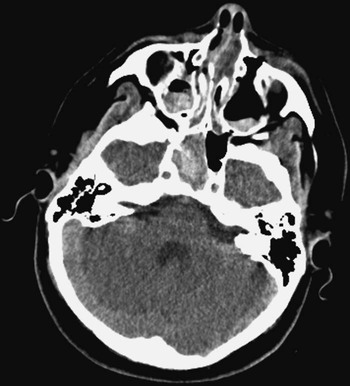
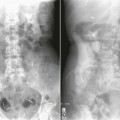
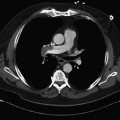
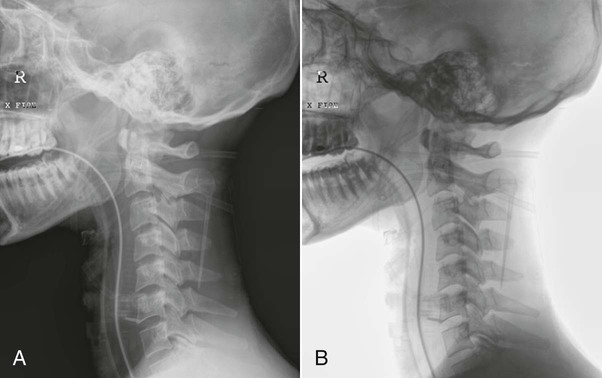
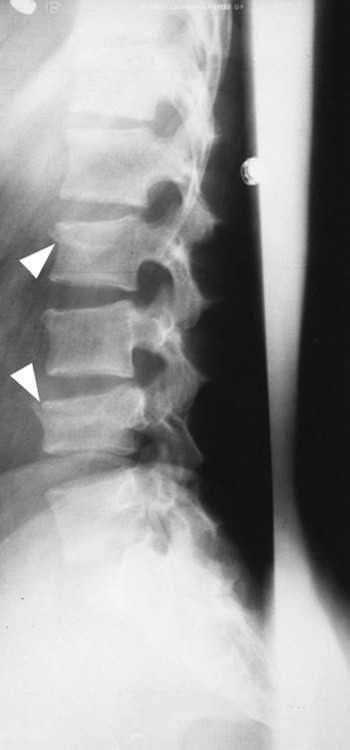
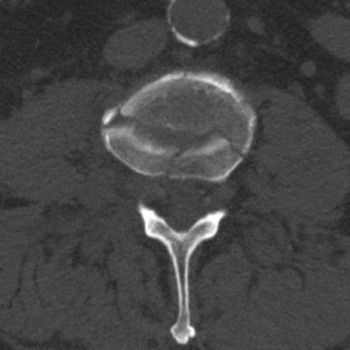
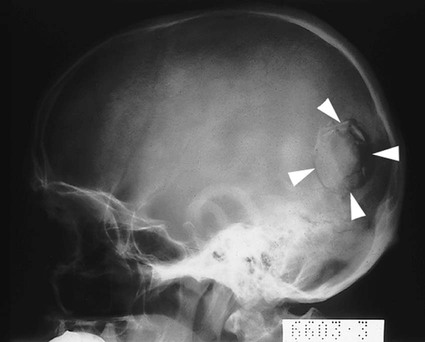
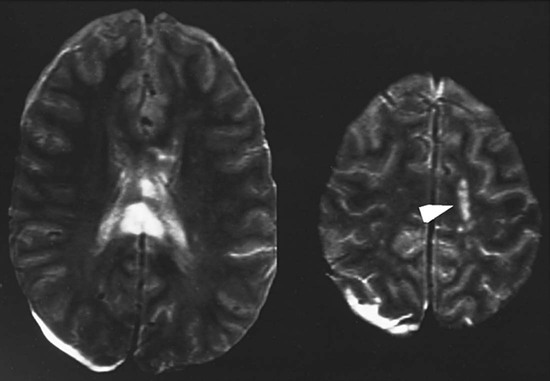
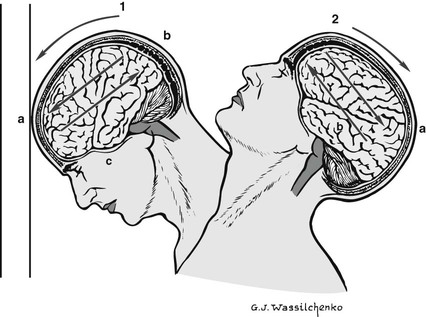
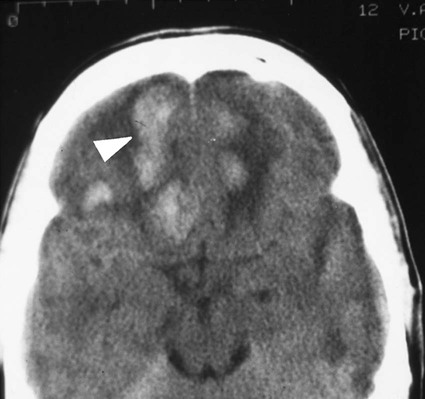
On completion of Chapter 12, the reader should be able to: • Differentiate among level I, II, and III trauma centers and the role each plays in the emergency medical system. • Define common terminology associated with traumatic disease. • Discuss the roles of various imaging modalities in the evaluation and treatment of traumatic injuries. • Describe, in general, the radiographic appearance of each of the given pathologies. • Classify skeletal fractures according to the various classifications discussed in this chapter and describe the healing process associated with skeletal trauma. • Describe the general methods used for the treatment of skeletal fractures. In the United States, injury is one of the leading causes of death and disability, and trauma is the most common cause of death for individuals between the ages of 1 and 44 years, accounting for over 48,000 deaths in 2008. Additional information can be obtained at the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics Web site at www.cdc.gov/nchs/hus.htm. The annual medical cost associated with trauma injury is approximately $200 billion and is classified by several categories. Some examples are as follows: Deaths from traumatic injuries have a trimodal distribution (Fig. 12-1), with the first critical period occurring seconds after the injury. Death during this period results from lacerations of the brain and spinal cord or the heart and great vessels. The second critical period occurs during the first 4 hours after the injury, with death generally resulting from intracranial hemorrhage, lacerations of the liver and spleen, or significant blood loss from multiple injuries. The third critical period occurs weeks after the injury, when death results from infection and multiple organ failure. With the prevalent use of multidetector CT (MDCT), CT evaluation of the cervical spine has become a standard procedure in evaluating trauma patients. The National Emergency X-radiography Utilization Study (NEXUS) and Canadian C-Spine Review (CCR) concluded that CT demonstrates 99.6% sensitivity for the identification of cervical spine fractures. CT has replaced conventional radiography as the first-line approach to imaging the cervical spine, with the meta-analysis of research studies performed in 2005 indicating that CT demonstrates a much higher specificity of 98% compared with a specificity of 52% for conventional radiography of the cervical spine. Axial CT of the cervical spine is performed in conjunction with coronal and sagittal reconstruction to fully assess the areas of interest (Fig. 12-2). With more sensitive imaging techniques now available, CT and MRI have revealed a significant number of fractures and other injuries that are not diagnosed with radiography. CT evaluation can reduce hospital admission rates and results in more efficient surgical intervention by accurately identifying the presence and extent of injury in the trauma patient. Blunt trauma to the abdomen is best evaluated with CT or abdominal sonography. Trauma to the urinary system occurs in about 10% to 15% of patients who experience blunt trauma to the lower abdomen and pelvis. In cases of hematuria, CT is preferred to conventional intravenous pyelography (IVP) or intravenous urography (IVU). Although the use of oral contrast agents for abdominal CT is debatable, intravenous contrast is routinely employed to allow evaluation of vascular injuries and to better visualize the spleen, pancreas, and kidneys. In addition, in cases of blunt abdominal trauma, CT is better able to visualize fractures of the transverse processes of the lumbar spine, often missed on conventional spine radiography. CT, in combination with a conventional anteroposterior (AP) pelvic radiography, is also used to assess pelvic fractures commonly associated with abdominal injury (Fig. 12-3, A). In cases of pelvic fractures, it is also imperative to identify any possible trauma to the urinary bladder and to perform CT (see Fig. 12-3, B) to determine the extent of injury. Occasionally, emergent cystography may be performed to visualize any injury to the urinary bladder. In cases of penetrating trauma to the abdomen, angiography may also be used to identify the extent of injury. Sonography plays little or no role in the evaluation of genitourinary trauma. Several studies have documented the inability of sonography to detect injuries of the kidney or bladder in trauma patients. The causes of vertebral column injuries include direct trauma and hyperextension–flexion injuries (whiplash injuries). Radiographic indications of spinal column injuries include the interruption of smooth, continuous lines formed by the vertebrae stacked on one another (Fig. 12-4). Either a dull or sharp pain in the posterior neck is the primary manifestation of a whiplash injury. The pain may radiate down the arms or back. Muscle spasm as a result of trauma may cause a reversal or straightening of the normal spine curvatures. Imaging of whiplash injuries is limited to soft tissue studies, with the exclusion of fractures and dislocations being the first priority. The loss of lordosis is the most common finding on radiographs of patients with whiplash injuries (Fig. 12-5). Compression fractures are the most frequent type of injury involving a vertebral body. Usually, the damage is limited to the upper portion of the vertebral body, particularly to the anterior margin. Such fractures generally occur in the thoracic and lumbar vertebrae (Fig. 12-6), with the most common site being T11-T12 in the thoracic spine and T12-L1 at the thoracolumbar juncture. Compression fractures are also associated with osteoporosis and range from mild to severe. More severe fractures may cause significant pain, leading to inability to perform activities of daily living to life-threatening decline in the older patient. Cervical spine injuries may involve the odontoid process, usually at the junction of the odontoid and the body of the second cervical vertebra (see Fig. 12-2). A hangman’s fracture (Fig. 12-7) is a fracture of the arch of the second cervical vertebra and is usually accompanied by anterior subluxation of the second cervical vertebra on the third cervical vertebra. A hangman’s fracture, sometimes referred to as traumatic spondylosis, results from acute hyperextension of the head. Fractures or dislocations of the vertebrae may impinge on the spinal cord and cause significant damage. The responsibility of the radiographer in terms of proper patient handling and obtaining diagnostic-quality images cannot be overemphasized. CT plays a vital role in the diagnosis and treatment of vertebral fractures, dislocations, and associated problems (Fig. 12-8). In certain situations, MRI may be used to evaluate the extent of ligamentous and soft tissue injury or injury to the spinal cord. Stable injuries to the spine are treated with complete bed rest and steroids until swelling and pain subside. Unstable injuries are immobilized with traction until bone and soft tissue structures have healed. Cervical radiographs are often obtained to demonstrate proper alignment while the patient is in traction. Surgery may also be necessary for internal fixation of the fractures or to remove displaced fragments and decompress the spinal cord. CT of the spine is used preoperatively to serve as a road map for the surgeon because this imaging modality clearly demonstrates the size, number, and location of various fracture fragments. It may also be used postoperatively to demonstrate the success of the surgical procedure (Fig. 12-9). The term cerebral cranial fractures usually refers to fractures in the calvaria of the skull. Vascular markings in the skull, either venous or arterial, are routinely demonstrated as linear translucencies and may occasionally be mistaken for cerebral cranial fractures (Fig. 12-10). In most cases, a fracture appears more translucent than a vascular marking because a fracture traverses the full thickness of the skull. Although the edges of the fractures may branch abruptly, they may be seen to fit together, whereas venous channels have irregular edges that cannot be fitted together. The sutures between the individual cranial bones remain visible radiographically, even after they become fused. To an untrained eye these sutures may also resemble a fracture. Fractures visible after skull trauma are generally classified as linear, depressed, or basilar skull fractures. Linear fractures appear as straight, sharply defined, nonbranching lines and are intensely radiolucent (Fig. 12-11). Up to 80% of all skull fractures are linear fractures. A depressed fracture appears as a curvilinear density because the fracture edges overlap (Fig. 12-12). These fractures are caused by high-velocity impact by small objects. Injury to the cerebral cortex may result, causing bleeding into the subarachnoid space. A depressed fracture is best demonstrated when the x-ray beam is directed tangentially to the fracture. Basilar skull fractures are very difficult to demonstrate radiographically. The presence of air–fluid levels in the sphenoid sinus or clouding of the mastoid air cells is often the only radiographic finding suggesting a fracture. Therefore, it is important to include cross-table lateral skull radiography with the trauma skull radiographic series. CT and MRI are often used to better identify basilar area fractures and associated soft tissue damage within the skull (Fig. 12-13). In addition to brain injury from a penetration wound (as could happen with a fracture), brain injury may also occur from acceleration and rapid deceleration of the head, which is termed a closed head injury or traumatic brain injury (TBI). With head trauma, the brain is traumatically shaken within the cranium and subjected to forces of compression, acceleration, and deceleration. Brain tissues are injured from compression, tension, and shearing, with the last perhaps most important (Fig. 12-14). The superficial cerebrum in the frontal, temporal, and occipital regions is most often affected. A brain contusion may also result from a direct blow to the head. This bruising of brain parenchyma is more serious than a concussion. A contusion formed on the side of the head where the trauma occurs is called a coup lesion, and one formed on the opposite side of the skull in reference to the site of trauma is a contrecoup lesion (Fig. 12-15). Contusions are characterized by neuron damage, edema, and punctate (pinpoint punctures or depressions) hemorrhaging. On CT, contusions appear as small, ill-defined foci of increased density (Fig. 12-16). Subdural or epidural hematomas may occur in conjunction with a contusion and result in increased intracranial pressure that may be life-threatening. Signs seen in the patient with a contusion include drowsiness, confusion, and agitation. Hemiparesis and unequal pupil size may also be seen. CT plays a major role in the diagnosis of hematomas resulting from contusions, providing ready visualization of hemorrhagic blood, as described in the following section. Treatment is generally conservative, centering on prevention of shock, control of edema, and drainage of any hematoma present. A hematoma is a collection of blood; four primary types of cerebral hematomas have been identified: epidural, subdural (Fig. 12-17), subarachnoid, and intracerebral. The highest mortality rate is associated with an epidural (extradural) hematoma (Fig. 12-18). Even when promptly recognized and treated, it has a mortality rate of up to 30%. An epidural hematoma results from a torn artery, usually the middle meningeal artery, with blood pooling between the bony skull and the dura mater. Most commonly, the artery or its branches are torn by a fracture of the thin, squamous portion of temporal bone. In more than 80% of cases, the skull fracture is visible radiographically. As an arterial bleed, it accumulates rapidly and quickly causes neurologic symptoms, including early coma. It is seen on CT scans as an increased density, generally occupying a small area with a sharply convex appearance. It is often accompanied by a fracture of the skull or facial bones. If not diagnosed and surgically treated quickly, the outcome is fatal as a result of brain displacement and herniation.
Traumatic Disease
Imaging Considerations
Radiography
Computed Tomography
Trauma of the Vertebral Column and Head
Injuries to the Vertebral Column


Injuries to the Skull and Brain
Cerebral Cranial Fractures.


Brain Trauma.
Hematomas of the Brain.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Traumatic Disease