Presentation and Presenting Images
( ▶ Fig. 100.1, ▶ Fig. 100.2, ▶ Fig. 100.3, ▶ Fig. 100.4, ▶ Fig. 100.5)
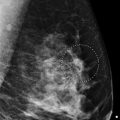
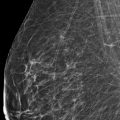
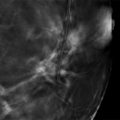
A 47-year-old female with a history of a right breast mastectomy 15 years ago for invasive ductal and lobular carcinoma presents for mammography.
100.2 Key Images
( ▶ Fig. 100.6, ▶ Fig. 100.7, ▶ Fig. 100.8)
100.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
100.2.2 Imaging Findings
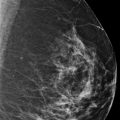
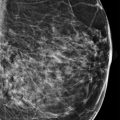
The right breast is surgically absent. The left breast demonstrates a 6-mm group of heterogeneous calcifications in the superior and posterior depth, 7 cm from the nipple (circle in ▶ Fig. 100.6 and ▶ Fig. 100.8). The finding is only seen on lateromedial (LM) conventional mammogaphy and digital breast tomosynthesis (DBT) views. The tomosynthesis slice 19 of 54 ( ▶ Fig. 100.7) localizes the finding to the medial aspect of the breast, which translates to approximately the 11 o’clock location.
100.3 BI-RADS Classification and Action
Category 4B: Moderate suspicion for malignancy
100.4 Biopsy Images
( ▶ Fig. 100.9, ▶ Fig. 100.10, ▶ Fig. 100.11, ▶ Fig. 100.12, ▶ Fig. 100.13, ▶ Fig. 100.14)
100.4.1 Imaging Findings
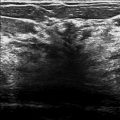
The calcifications are well demonstrated on tomosynthesis and may be biopsied using tomosynthesis-directed stereotactic biopsy. DBT localized the calcifications to the medial aspect, and so biopsy should be performed in the mediolateral (ML) projection. The images presented are the prefire ( ▶ Fig. 100.9 and ▶ Fig. 100.10) and the postfire ( ▶ Fig. 100.11 and ▶ Fig. 100.12) tomosynthesis images and the final mammogram after clip placement ( ▶ Fig. 100.13 and ▶ Fig. 100.14).
100.5 Differential Diagnosis
Fibrocystic changes: Although most commonly presenting as milk-of-calcium calcifications, fibrocystic changes may present as heterogeneous calcifications.
Ductal carcinoma in situ (DCIS): Heterogeneous calcifications are more likely to be associated with DCIS than invasive ductal carcinoma.
Lobular neoplasia: Heterogeneous calcifications have been found to be associated with atypical breast lesions such as lobular neoplasia, which are high-risk breast lesions that have uncertain malignant potential.
100.6 Essential Facts
Fibrocystic change (FCC) of the breast is a benign alteration in the terminal ductal lobular unit of the breast with or without associated fibrosis.
FCC is most commonly diagnosed in women 20 to 40 years of age. This is a very common finding that is observed clinically in up to 50% of women and histologically in 90% of women.
The ACR BI-RADS Atlas, 5th edition, classifies as typically benign calcifications those described as skin, vascular, coarse or popcornlike, large rodlike, round, rim, dystrophic, milk of calcium, and suture. Calcifications that are suspicious are described as amorphous, coarse heterogeneous, fine pleomorphic, and fine linear or fine-linear branching.
Although, the calcifications are not seen on the left CC view, they are well seen on the left LM tomosynthesis movie and the left LM conventional mammographic view. Tomosynthesis places the calcifications in the medial aspect of the breast. The calcifications were heterogeneous (a suspicious morphology) and were therefore biopsied.
100.7 Management and Digital Breast Tomosynthesis Principles
Although DBT cannot magnify calcifications, it can be used to localize and biopsy calcifications.
Findings identified only on DBT may not be reproducible on the prone stereotactic table.
In this case, a left CC tomosynthesis movie was not performed due to the posterior location of the calcifications. The calcifications could be and were localized using the LM view. If surgery had been required, needle localization could have performed using tomosynthesis guidance.
Tomosynthesis-directed biopsies utilize the full detector for imaging and do not require triangulation for biopsies. Biopsies performed with tomosynthesis may be performed more quickly than with the prone stereotactic table.
Some patients are needle averse and are unable to tolerate having the biopsy needle within sight. In these cases, the prone stereotactic table is the preferred option.
100.8 Further Reading
[1] Guray M, Sahin AA. Benign breast diseases: classification, diagnosis, and management. Oncologist. 2006; 11(5): 435‐449 PubMed
[2] Schrading S, Distelmaier M, Dirrichs T, et al. Digital breast tomosynthesis-guided vacuum-assisted breast biopsy: initial experiences and comparison with prone stereotactic vacuum-assisted biopsy. Radiology. 2015; 274(3): 654‐662 PubMed

Fig. 100.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree