Ben Plotkin, MD
MRI OF THE HIP JOINT
The hip joint is a ball and socket type of joint that is also the deepest joint in the body. Since this joint transfers weight from the upper body to the lower limbs, it is subject to a range of problems resulting from faulty weight-bearing positions in normal individuals to problems caused by wear and tear in those who are athletically active. Moreover, the symptoms related to hip pathology can have myriad of manifestations ranging from focal pain to just a vague groin pain. Sometimes an injection of local anesthetics into the hip joint might be required to help diagnose the actual source of the patient’s pain.
IMAGING TECHNIQUES
All imaging studies should begin with radiographs that help differentiate many benign conditions at the outset from what might appear to be very confusing on magnetic resonance imaging (MRI) studies. One should also remember that any unexplained hip pain without any apparent radiographic findings is an indication for MRI if the pain does not resolve within a week. It might be a referred pain, but it alerts the radiologist and the referring physician to the possibility of more ominous conditions like the beginning of an avascular hip necrosis. We routinely perform coronal T1-weighted and short-tau inversion recovery (STIR) sequences of the pelvis that include both hips. This helps in conditions like avascular necrosis (AVN) that might be bilateral. It also helps in comparing common anatomical variants or clarifying imaging artifacts. Then we scan the affected hip in axial T1-weighted or proton density and fluid-sensitive sequences. T2-weighted fat-suppressed sequences are useful in assessing for edema. Sagittal sequences are added to assess the musculature and look for what, if any, part of the weight-bearing surface is affected. In case of hip arthrograms, sequences are tailored to assess for labral pathology. If AVN is a possible diagnosis but the MRI is equivocal, we suggest the referring physician put the patient on restricted weight bearing and repeat the MRI study in a month.
In this chapter, we provide a brief introduction of the hip pathologies one that is most likely to seen and then describe some relatively less common conditions. Interested readers are referred to the references at the end of the chapter for further studies.
AVN is discussed first, followed by less common conditions, and then basic concepts of femoroacetabular impingement syndrome are discussed. This is becoming a more common diagnosis as knowledge of it spreads and the population becomes more physically active at a younger age. In the end, associated conditions like sacral fractures and some basic concepts of pubalgia or “sports hernias” are discussed briefly.
AVASCULAR NECROSIS
AVN is a crippling process that can lead to collapse of the femoral head and the onset of disabling osteoarthritis. There is a long list of conditions that predispose to AVN; some of the more common ones are steroid use, alcoholism, sickle cell disease, lupus, and trauma. As with many other conditions, the true pathogenesis of AVN varies with etiology. In trauma, the culprit can be disruption in the blood supply; in lupus, the etiology may be due to vasculitis; and in steroid use the etiology may be due to hypertrophy of fat cells leading to venous compression and then infarction.1,2 Table 17-1 lists common causes of AVN.
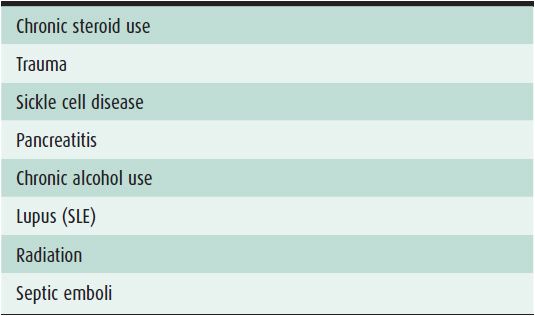
Table 17-1. Common Causes of AVN
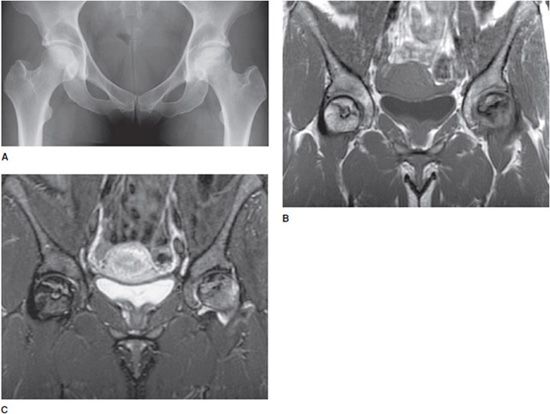
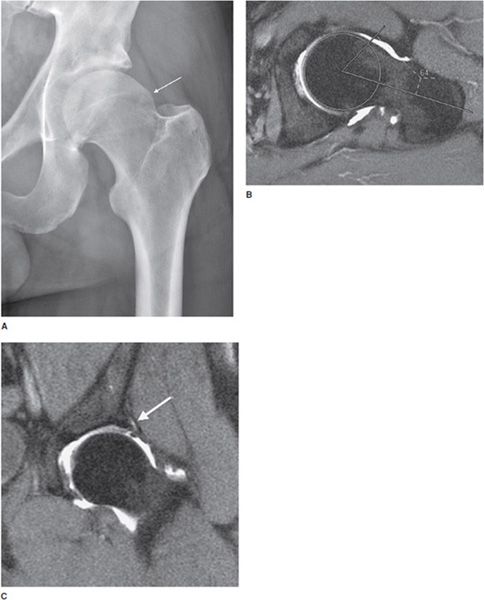
AVN may initially be occult on radiographs, whereas its early stages may be visible on MRI. Early radiographic changes are seen as subtle osteopenia followed by sclerosis of the femoral head and then loss of normal contour (Figure 17-1A–C). Early AVN on MRI may just manifest itself as marrow edema.
Figure 17-1. Early AVN of both hips. (A) Radiograph of woman with SLE shows flattening, collapse, and sclerosis of the left femoral head from AVN. There is faint sclerosis without collapse of the right femoral head. (B) Coronal T1-weighted MRI shows T1 dark serpentine lines in the femoral head, which extend to the subchondral surface. Note that the AVN of the right hip is very subtle on the radiograph, but clearly visible on the MRI. (C). Coronal STIR image shows both T2 dark and T2 bright serpentine lines in the femoral heads. The dark and bright lines parallel each other giving rise to the “double line sign.” There is marrow edema in the femoral heads, more significant on the left side.
The classic findings of AVN on MRI is a subchondral area of low T1 signal intensity, which is outlined by a dark T1 line (Figure 17-1B). On T2-weighted images, there may be a bright signal line that parallels the dark line, which is referred to as the “double line sign,” which has worked its way into the lexicon of classical findings in radiology (Figure 17-1C). Although by the time the double line sign is visible, this is very late in the disease process. The lines that demarcate AVN are traditionally seen and described as serpentine.3,4 As AVN progresses, there will be collapse of the femoral head (Figure 17-1A).
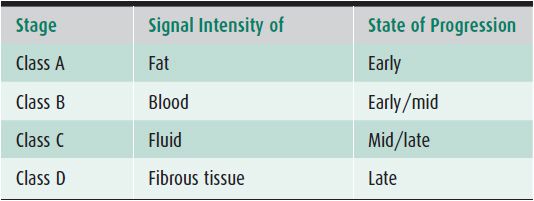
There is an MR staging system, Mitchell Staging, for AVN that takes into account the signal characteristics of the affected area. It breaks the lesion down into class A, B, C, and D (Table 17-2). Class A lesions have signal characteristics that are similar to fat, which will be high on T1, and intermediate on T2-weighted sequences. Class B lesions have signal characteristics that are similar to blood with high T1 and T2 signal. Class C lesions have signal characteristics similar to fluid (low-to-intermediate signal on T1-weighted images and high T2 signal). Class D lesions have signal characteristics close to fibrous tissue being dark on both T1- and T2-weighted sequences. The staging system can be useful as early AVN tends to be a class A or B lesion, while late stage AVN is class C or D.5
Table 17-2. Mitchell Staging System for AVN
PEARLS
BONE MARROW EDEMA SYNDROME (TRANSIENT OSTEOPOROSIS)
There are times when the proximal femur is affected by an unknown process, which is characterized by rapid demineralization of the proximal femur with marked corresponding marrow edema, which is seen when imaged with MR. The older term used to describe this condition was transient osteoporosis of the hip, a newer term that is used in bone marrow edema syndrome. Neither term is very satisfying, which just reflects the depths of our ignorance about what is truly causing this process. As of now we just label it with the generic idiopathic, although there are many theories as to what is the underlying etiology.
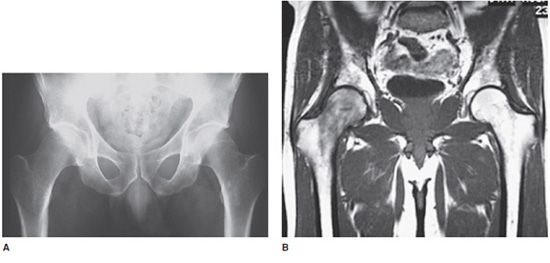
Transient osteoporosis is usually seen in middle-aged men and in pregnant women, and while we may not understand its etiology clearly, for the patient it is quite real. Patients present with acute hip pain, which can be crippling. On imaging, the radiographs and computed tomography (CT) will show an area of focal demineralization of the femoral head (Figure 17-2A), which may be subtle, but once the patient is imaged by MRI, the findings are usually readily apparent.
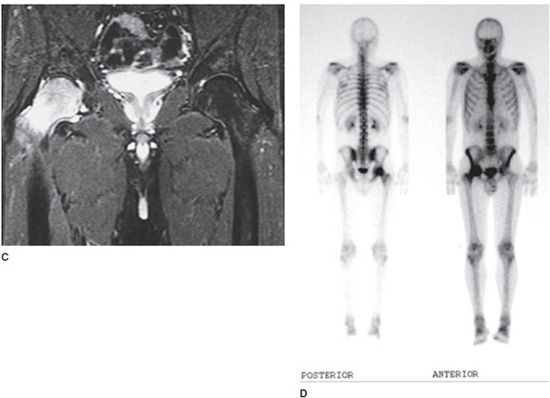
Figure 17-2. Femoral head edema of the right hip (transient osteoporosis). (A) Radiograph shows relative demineralization of the right proximal femur as compared with the left. (B) and (C) Coronal T1-weighted MR image (B) shows focally decreased signal in the right femoral head, which corresponds to the edema in the femoral head on the coronal STIR image (C). Also note the T2 bright fluid in the right femoroacetabular joint from a joint effusion. A key observation is that the marrow signal of the acetabulum is normal. This may mitigate infection. (D) Anterior and posterior whole body views from a technetium 99m-MDP bone scan. Image shows focally increased uptake in the right proximal femur, which corresponds to the edema as seen on MRI.
MRI will show marked edema in the femoral head and neck, which is manifested by dark T1 and bright T2 signal (Figure 17-2B and C). Often there will be an associated joint effusion. Since one of the key differential diagnoses is a septic joint, the effusion may need to be tapped to exclude an infection. However, transient osteoporosis is confined to the femur so the acetabulum will have normal signal, which can be a clue that can help to separate it from infection. Often, though, this is a diagnosis of exclusion. If a bone scan is done, there will be increased uptake in the bone corresponding to the edema (Figure 17-2D).
The process is usually self-limiting with resolution of symptoms in 6–8 months. There is an entity called regional migratory osteoporosis in which after the symptoms resolve in one joint, they reappear later in another joint, often in a nearby joint.
Some theories suggest the edema and pain in the femoral head are related to trauma, and it is important to exclude an underlying fracture or AVN.6–8 So while we can recognize the entity on MRI, we are not sure of its true etiology.
PEARLS
OSTEOID OSTEOMA
Osteoid osteomas are benign tumors. The classic history is of a young patient (10–20 years of age) presenting with pain, which is worse at night and relieved by aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs). Osteoid osteomas are relatively common lesions and the proximal femur is one of the areas they commonly occur. They can occur within the cortex and the medullary portion of the bone, and rarely can occur intra-articularly.
On radiograph or CT, they will show up as a small lucent lesion, which should be less than 2 cm. There is often reactive sclerosis surrounding the lesion and a central lucent or dense (calcified) nidus is visible9 (Figure 17-3A). On MRI, most osteoid osteomas have low T1 signal (Figure 17-3B) and a variable amount of T2 intensity. Because osteoid osteomas are often associated with surrounding edema, this marrow edema will be clearly visible as bright T2 signal on fat-saturated T2-weighted imaging (Figure 17-3C). If the lesion is intra-articular, there may be an associated joint effusion, which will manifest itself as T2 bright fluid within the joint space.10 The central nidus of the osteoid osteoma may be difficult to appreciate on MRI and will be more apparent on CT study (Figure 17-3A).
Figure 17-3. Osteoid osteoma. (A) Sagittal reformatted CT shows a small oval lucent lesion (arrow) with a central calcification in the nidus in the left anterior superior iliac spine. (B) and (C) Coronal T1 (B) and coronal T2 fat-saturated MR images (C) show that the osteoid osteoma is dark on T1 (arrow) with surrounding bright T2 signal from the edema. There is also some edema in the adjacent musculature (arrowheads). Note that the central nidus is visible on CT but not on MR.
The main differential diagnosis to consider is a focal infection or Brodie abscess. It can be difficult to tell them apart as both may have surrounding reactive edema, and a Brodie abscess can have a central sequestrum, which mimics the central calcified nidus of an osteoid osteoma, although other features such as a sinus track or irregularity of an infectious abscess can help to separate the two entities.
Standard treatment of an osteoid osteoma is radio frequency ablation, which is favored over surgical resection. Although in some cases the lesion can be treated symptomatically, it may regress or resolve over time.11
FEMOROACETABULAR IMPINGEMENT
Femoroacetabular impingement (FAI) can be best thought of as several different anatomical variants that predispose to the development of premature osteoarthritis. The diagnosis of FAI is most effective when it is made in younger and often athletic patients; the goal is to make an early diagnosis so that they may potentially be spared the pain and debilitation of early osteoarthritis. FAI morphology can be seen in older patients who have already developed osteoarthritis, but at this point the treatment options available to younger patients usually do not apply.
The normal Femoroacetabular joint is a ball and socket joint, with the rounded femoral head articulating in the cup of the acetabulum. In an idealized body, the femoral head smoothly articulates with the acetabulum. In FAI, there is abnormal morphology to the joint, which causes friction and abnormal contact between the femoral head and the acetabulum and labrum. This repeated wear, over time, leads to tears of the labrum and the development of early osteoarthritis.
FAI has become a recent hot topic in both the radiology and orthopedic communities as radiologists have sought to identify the underlying anatomy that can predispose an individual to developing FAI, and orthopedic surgeons have attempted to correct or alter the morphology of the hip to prevent the development of osteoarthritis. For some radiologists, the issue of FAI remains controversial.
FAI can be a difficult diagnosis to make and is not truly a radiologic diagnosis. The diagnosis of FAI should only be made in combination with an orthopedic surgeon and take into account not only the imaging findings but also the clinical symptoms of the patient. Even when the diagnosis is made, there is controversy within the orthopedic community as to when and how to proceed with treatment.12
The two main types of FAI are the cam type and the pincer type, although there may be overlap between the two. Cam-type FAI can be thought of as a problem with the femoral head, while the pincer-type FAI is more of a problem with the acetabulum.
 Cam-Type FAI
Cam-Type FAI
Cam-type FAI is caused by an abnormal morphology to the femoral head at the head–neck junction. There is an extra bump or mound of bone located along the lateral femoral head–neck junction, which impacts against the labrum and the acetabular cartilage with movement. Over time, this causes continuous wear, which leads to osteoarthritis.13
This bone bump seen in cam-type FAI is located along the lateral proximal femur at the level of physeal scar, which straddles the head–neck junction. This can be seen on radiograph (Figure 17-4A) and has been described as the “pistol grip” deformity. This abnormal morphology is most often seen in young men, and although it is not clear what the cause is, some theories suggest it may be from abnormal bone growth that may have resulted from prior slipped capital femoral epiphysis, Legg–Calvé–Perthes syndrome, or traumatic injury. Alternatively, it may just be a normal developmental variant.14
Figure 17-4. FAI. (A) Radiograph shows a prominent bone bump (arrow) just distal to the lateral femoral physeal scar. (B) Alpha angle in FAI. Axial oblique T1-weighted fat-saturated arthrogram shows measurement of alpha angle. One line is drawn down the midportion of the femoral neck, the other line from center of the femoral head to the junction of the femoral bump. The alpha angle here is abnormal (angle greater than 55°). (C) Hip labral tear. Coronal T1-weighted fat-saturated arthrogram shows a labral tear (arrow) in a patient with impingement morphology. There is also joint space narrowing and articular cartilage damage.
Radiologists are sometimes asked to quantify the degree of a morphologically abnormal appearing proximal femur. One method involves measuring the angle between the femoral head–neck junction. This angle is called the alpha (α) angle and can be measured on a radiograph or an MRI (Figure 17-4B). It is calculated by drawing a line from the center of the femoral head to the beginning point of the bump at the head–neck junction, and a line bisecting the long axis of the femoral head and neck. An angle greater than 55° is considered abnormal.15,16
 Pincer-Type FAI
Pincer-Type FAI
Pincer-type FAI is a problem with the acetabulum, which just as in cam-type FAI, over time leads to early osteoarthritis. This can be an even more difficult diagnosis to recognize than the cam-type morphology. In pincer-type FAI, the acetabulum is too large for the size of the femoral head, which results in overcoverage of the femoral head. Thus, as the femoral head rotates it bangs against the periphery of the acetabulum. This repeated impaction is what leads to the development of osteoarthritis.
Acetabular retroversion is associated with pincer-type FAI. The normal acetabulum is anteverted, which means that the opening of the acetabulum is more anterior. In acetabular retroversion, the opening of the acetabulum is directed more posteriorly. This can be recognized on radiograph or CT if the anterior wall of the acetabulum projects more laterally than the posterior wall. Or to put it another way the anterior rim of the acetabulum should always be more medial than the posterior wall of the acetabulum. This is easier to recognize on CT; looking for this finding on a radiograph can be difficult as precise positioning is needed.17
 Secondary Signs in FAI
Secondary Signs in FAI
Other findings that are often present in FAI are the presence of an associated labral tear and articular cartilage damage. These are stigmata of the constant abnormal motion of the femur against the acetabulum, and treatment is aimed at preventing or delaying the wear and tear of the labrum and articular cartilage (Figure 17-4C).
An os acetabuli, which is a triangular-shaped calcification adjacent to the lateral acetabulum, is associated with FAI. This calcific body is thought to develop from the constant impaction of the acetabulum against the femur causing a portion of the labrum to calcify (Figure 17-5) and sometimes even separate. Not all os acetabuli are pathologic or signify that there is impingement. It can be a normal variant caused by nonunion of the os acetabuli with the os pubis during childhood.18
Figure 17-5. FAI os acetabuli. Radiograph shows a prominent os acetabuli (arrows).
A synovial herniation pit, or Pitt’s pit, appears on radiograph as an oval lucency that occurs at the anterior superior femoral neck junction (Figure 17-6). These appear on MRI as subcortical cysts. They develop at the anatomic site where impingement occurs. Fibrocystic change is another term that is often applied to this finding. Herniation pits are thought to develop from repeated stress, although they are not always associated with FAI.19,20
Figure 17-6. Synovial herniation pit. Radiograph shows a lucency (arrows) with a sclerotic rim in the proximal femoral neck. This is the typical appearance of a herniation pit, which can be a secondary sign of FAI.
Late-stage manifestation of FAI is the same as osteoarthritis with joint space narrowing, articular cartilage damage, osteophytes, and subchondral cysts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree