Fig. 1
Ephraim McDowell (1771–1830): the father of abdominal surgery. Performed the first laparotomy on Christmas Day 1809. Painting by P.W. Davenport in McDowell House. (Photo: Chris Sutton with permission from McDowell House, Danville, Kentucky)
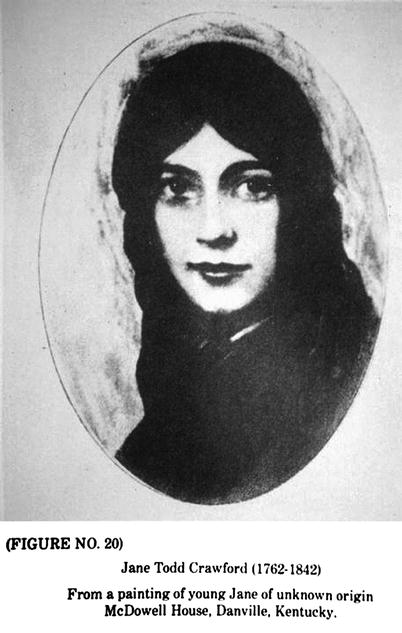
Fig. 2
Jane Todd Crawford (1763–1842). From a painting of young Jane of unknown origin. Reproduced courtesy of McDowell House, Danville, Kentucky
4.2 The Surgeon: Ephraim McDowell
McDowell’s family were of mixed Irish and Scottish extraction and he was born in Rockbridge County, Virginia in 1771, the ninth of 12 children (Othersen 2004). When he was 13 years old the family moved to Danville, a frontier town that was the first capital of the State of Kentucky, where his father was appointed Judge of the small community of some “150 homes and some tolerably good buildings” (Ellis 2009). This was before the era of Medical Schools in the United States of America and the young Ephraim decided on a career in medicine early in his life and served as an apprentice to a family physician, Dr Alexander Humphreys in Staunton, Virginia (Gray 1987). When he was 22 he spent 2 years studying anatomy in Edinburgh under Alexander Munro and surgery under the tutelage of John Bell. For financial reasons he had to return home to Danville without earning a medical degree but even without the letters after his name the prestige of being educated at one of the most famous medical schools in the world ensured that he rapidly built up an extensive surgical practice and he came to be regarded as “the best doctor west of Philadelphia” (Tan and Wong 2005). He was renowned for his swift amputations, hernia repairs and lithotomies and would typically operate in the homes of patients with family members gathered round to hold the unfortunate sufferer down. One of his patients was James Polk who, as a 14-year-old boy had several bladder stones removed, and later became the 11th President of the United States (Graham 1981; Bernhard 1980). McDowell’s fame spread locally among the frontier people because this was an area that was expanding rapidly after Dr Thomas Walker had opened up the Wilderness Trail through the Cumberland Gap from Virginia into Kentucky accompanied by frontiersmen and Indian fighters such as Daniel Boone and Davy Crockett (Gray 1987).
4.3 The Patient: Jane Todd-Crawford
Jane Todd-Crawford lived with her family of five children in a small log cabin in Motley’s Glenn near Greensburg, Kentucky, some 60 miles from Danville and at the age of 44 she was thought to be carrying another child and was causing concern with the local doctors and midwives because she was 2 months beyond her due date. The attending physicians were in despair and had tried various potions and enemas used to induce labour and in desperation had even employed two midwives to jump up and down on her extremely distended abdomen. All this was to no avail and the poor woman had such a swollen abdomen that she could barely breathe and in desperation they decided to summon the “surgeon from Danville”.
Although the journey from Danville to Greensburg can nowadays be easily accomplished in an hour or so using modern highways, in 1809 it required a lengthy and difficult journey on horseback, crossing many mountain ridges and fording deep rivers and when McDowell set out on this arduous journey the snow had already fallen deeply and there were added hazards from bands of skirmishing Indians, to say nothing of predatory wolf packs and bears. When he arrived he quickly appraised the situation and saw that the swollen abdomen did, indeed, have the appearance of a pregnancy, possibly a multiple one, with a size that was indeed making it difficult for the patient to breathe.
Without recourse to sophisticated imaging techniques it is often difficult clinically to distinguish a massive fibroid from a large ovarian tumour or, indeed, from a term pregnancy (Fig. 3). Possibly because of his education in Edinburgh under the tutelage of the anatomist Alexander Monroe (Secundus), he performed a more thorough examination than had been performed by the local physicians and this included a vaginal examination where he found that the mass was inclined to one side and was mobile and his examining finger felt a normal sized uterus and cervix which were pushed to the other side, all of which indicated that the mass was an “enlarged ovarium”.


Fig. 3
Massive ovarian cyst. When removed weighed half of the patient’s weight (Photo: Chris Sutton. St. Luke’s Hospital, Guildford)
Clearly, he was very depressed by his findings and in an account written many years later to a medical student he wrote “I told the lady that I could do her no good and candidly stated to her, her deplorable situation; informed her that John Bell, Hunter, Hay and A Wood, four of the first and most eminent surgeons in England and Scotland, had uniformly declared in their lectures that such was the danger of peritoneal inflammation that opening the abdomen to extract the tumour led to inevitable death.” She was clearly devastated by this pronouncement but told him that it was impossible to continue to live in her present situation since she was almost unable to breathe and felt that she would die anyway. He therefore continued “but, notwithstanding this, if she thought herself prepared to die, I would take the lump from her if she would come to Danville.” He ended this account by stating simply “she appeared willing to undergo an experiment.” (Gray 1987). This must surely be the first documented case of informed consent.
4.4 The Operation
Dr. McDowell returned to Danville expecting to hear no more from her because even the journey with the increasing snowfall that winter was long and difficult and dangerous by horseback, but she was a tough frontier woman and a few days later appeared on his doorstep. Unfortunately the arduous journey had caused considerable bruising over the lower abdomen, where she had rested the enormous tumour on the pommel of her saddle. He therefore determined to wait for a few days before deciding to perform the operation and, being a deeply religious man, he timed the procedure to occur on the morning of Christmas Day when many of the townsfolk were in church so that they could bring the efforts of their combined prayers onto his endeavour. He was joined by his nephew, Dr James McDowell, who had graduated a few months previously from the first medical school in America in Philadelphia to join the practice as a partner and he did his best to dissuade his uncle from “the experiment”. The kitchen table was dragged into the front room and Jane Todd Crawford was placed on her back on the table and tilted slightly to the right side and then “he removed all her dressing which might in any way impede the operation”. Many years later when he wrote about the procedure he described it as follows:
I made an incision about 3 inches from the rectus abdominus muscle on the left side, continuing the same 9 in length, parallel with the fibres of the above-named muscle, extending into the cavity of the abdomen … the tumour then appeared full in view but was so large that we could not take it away entire. We put a strong ligature around the fallopian tube near the uterus and then cut open the tumour, which was the ovarium and fimbrious part of the fallopian tube, very much enlarged. We took out 15 lbs of a dirty gelatinous-looking substance, after which we cut through the fallopian tube and extracted the sac, which weighed 7 lb and one-half… As soon as the external opening was made the intestines rushed out upon the table and so completely was the abdomen filled by the tumour that they could not be replaced during the operation which was terminated in about 25 min. We then turned her upon her left side so as to permit the blood to escape, after which we closed the external opening with the interrupted suture, leaving out at the lower end of the excision the ligature which surrounded the fallopian tube.
During the whole of this ghastly painful procedure Jane Todd-Crawford remained motionless and merely recited the Psalms in order to calm herself during her ordeal.
She stayed in McDowell’s house and the bed in which she lay can still be seen because the entire house and gardens have been turned into a museum to commemorate this amazing feat of pioneering surgery. Ephraim McDowell visited her on a daily basis but on the 5th day he found her making her own bed and reprimanded her severely. She continued to make an excellent recovery and 25 days later she returned home in good health by the same route that she had come, which is now a long distance path named “The Jane Todd Crawford Trail”.
The two of them never met again during their lives. Ephraim McDowell died at the age of 59 years of “an acute attack of inflammation of the stomach” which was probably appendicitis and long before the time when a laparotomy could be performed to remove the infected organ. Jane Todd Crawford outlived him and died at the age of 78 years and a picture of her in her old age (Fig. 4) shows her displaying a locket with the picture of Abraham Lincoln, who was born in a log cabin at Sinking Spring Farm very close to where she grew up in Greensburg County and to whom she was related as a cousin when he married one of her sisters.


Fig. 4
Jane Todd Crawford as an old lady holding a locket with a portrait of Abraham Lincoln, a distant cousin by marriage to one of her older sisters (Photo: Chris Sutton with permission from McDowell House, Danville, Kentucky)
Unlike his modern counterparts, Ephraim McDowell did not immediately rush off to get this operation published and waited until he had performed two more successful ovariotomies in 1813 and 1816 before reporting it in a journal with a limited readership, “The Eclectic Repertory and Analytical Review of Philadelphia”. Two years later he published two further cases in the same journal, one of whom survived, but the other died of peritonitis on the third post-operative day. During his lifetime he performed three further ovariotomies between 1822 and 1826. One involved merely drainage but the patient lived for a long time afterwards, the second underwent complete excision, but the third had to be abandoned because of extensive adhesions.
There were a further three that are mentioned in letters and on reading his descriptions it does seem that, although he styled himself an ovariotomist, at least two of his cases were large pedunculated myomas (Ricci 1945; Graham 1950).
News of great surgical advances took a long time to percolate across the Atlantic and even in America McDowell’s achievement was greeted with a certain amount of scepticism and even outright disbelief (Gray 1987). It was 14 years later that the first ovariotomy was carried out in Europe by John Lizzars, a fellow student from Edinburgh, but the patient died and he then made three more successful attempts in 1825. The initial years of abdominal surgery were associated with an enormous mortality rate, mainly due to uncontrolled haemorrhage or peritonitis and sepsis.
4.5 The First Abdominal Hysterectomy on November 17, 1843
The greatest of the ovariotomists in Europe was Charles Clay of Manchester, in the North of England. He studied at the Manchester Royal Infirmary and, like Ephraim McDowell received part of his medical education in Edinburgh. Like McDowell he also started in surgical practice in a small rural community, Ashton-under-Lyne under the shadow of the Pennines in Cheshire. After 16 years he moved to the industrial city of Manchester where he established his surgical reputation. He was a member of the Reform Club and was a friend of my great grandfather, William Sutton, who was a successful businessman in this thriving Victorian metropolis. He is shown in Fig. 5 at the peak of his surgical career, profoundly confident and appearing dapper with his top hat. He was the first to introduce the word ‘ovariotomy’, a strange choice for the name of this operation in an age when most surgeons were reared in the classics and therefore etymologically correct (Morton 1965).


Fig. 5
Charles Clay (1801–1893) who performed the first successful abdominal hysterectomy in Europe on 2 January 1863. Reproduced with permission of the Royal College of Obstetricians and Gynaecologists of London
The first four of his ovariotomies survived but with the fifth he was not so lucky and this turned out to be the first abdominal hysterectomy recorded and it turned out to be a compete disaster. The operation was performed on 17 November 1843 in the first floor room above his Consulting Rooms in Piccadilly, the large square in the centre of Manchester. As was usual in those days he was accompanied by several friends and medical students as spectators and since it was before the time of Pasteur or Lister no one wore masks or surgical gloves and the patient was given brandy and milk to alleviate the pain of the operation since this was a long time before anaesthesia was introduced by WRT Morton in 1846. He was certain that he was dealing with a massive ovarian cyst so he made a long 60 cm surgical incision from the xiphisternum to the pubis. Unfortunately once the peritoneum was entered the patient coughed and the massive tumour was extruded (Fig. 6) and he realised to his horror that it was a huge fibroid and since the patient was now struggling and had to be forcibly restrained by the medical students and it was impossible to replace the hugely enlarged uterus back in the abdominal cavity he had no option but to proceed and performed a subtotal hysterectomy. By an extraordinary coincidence a few days later on the 21st of November, A M Heath who was also an ovarian surgeon in Manchester, found himself in a similar situation operating on a huge fibroid instead of an ovarian cyst. Unfortunately both patients died of a massive haemorrhage a few hours later (Sutton 1997; Benrubi 1988).
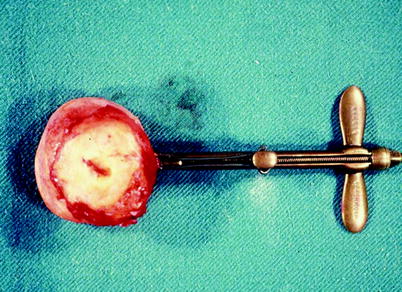
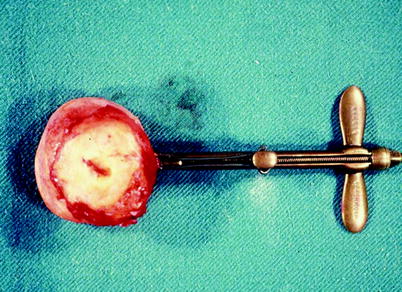
Fig. 6
Massive fibroid exposed at laparotomy (Photo: Chris Sutton from drawing by Medical Illustration Department, St. Luke’s Hospital , Guildford). Reproduced with permission
The next year, he was more successful with a similar case but on this occasion he placed a ligature of Indian hemp around the supra-vaginal cervix to prevent haemorrhage from the uterine arteries. The patient lived for 15 days, when she fell out of bed in a coma and never regained consciousness. Although this was tragic for the patient it was also sad for Clay since she had survived the critical post-operative period and not succumbed to sepsis, the usual cause of death (Benrubi 1988; Bachman 1990).
From reading contemporary accounts of this woman’s post-operative course it is difficult to determine the exact mode of death. She could have had a pulmonary embolus or she could have fallen out of bed in uraemic coma due to occlusion of both ureters by the ligature but popular Mancunian folklore suggests that she was dropped on the floor by a couple of incompetent porters while the nurses changed her bed linen. If this is true then her death was entirely unrelated to the operation and Charles Clay could have claimed to have performed the first successful hysterectomy in the world.
In fact it was not for a further 20 years that he attempted another hysterectomy and this time the patient survived. Interestingly he mentioned this almost as an aside during his important presentation to the Obstetrical Society of London in 1863 when he presented his experience of 395 ovariotomies with only 25 deaths (Clay 1863).
4.6 The First Successful Hysterectomy in the World
The first successful removal of a fibroid uterus was by Walter Burnham in Lowell, Massachusetts in 1853 (Speert 1980). This operation took place in the early days of anaesthesia and the ether caused the patient to vomit so when he made a massive incision from the sternum to the pubis, a large fibroid uterus was extruded through the incision when in fact Burnham was anticipating a massive ovarian cyst. It proved impossible to replace the massive fibroid and he had little choice but to proceed with a subtotal hysterectomy tying off both uterine arteries. The patient recovered and the fact that the original diagnosis was incorrect should not detract from his achievement. He performed a further 15 hysterectomies during the following 13 years but only three survived—the rest succumbing to sepsis, peritonitis, haemorrhage and exhaustion.
Later that year in September, in the same town of Lowell, Gilman Kimball carried out the first deliberate hysterectomy for a fibroid tumour with the patient surviving the operation (Matthieu 1985; Kimball 1855).
It is interesting that these two surgeons came from a small town in rural Massachusetts and considering that hysterectomy is the second most common operation performed on women, second only to caesarean section, that enquiries at the tourist office as to where these operations actually took place lead nowhere and it seems that the burghers of that small town are quite unaware of the fame that should be the just due of these two pioneering surgeons.
4.7 The First Successful Hysterectomy in Europe
Eugene Koeberle from Strasbourg was one of the greatest surgeons in Europe in the latter half of the nineteenth century and the French usually claim that he performed the first successful hysterectomy in Europe. The operation was for fibroids and the diagnosis was correct and in order to obtain haemostasis he used a device of his own invention called a serre-noeud which was a wire loop tightened by a screw device that held the cervix like a clamp and allowed it to be exteriorised through the wound (Fig. 7). Eventually the avascular cervical stump necrosed and fell back into the pelvis. This operation took place on 2 April 1863 and was certainly the first in continental Europe but in his lecture to the Obstetrical Society of London Charles Clay had briefly mentioned a successful case of “the entire removal of the uterus and its appendages” which he had performed in Manchester a couple of months earlier on 3 January 1863 (Clay 1863




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree