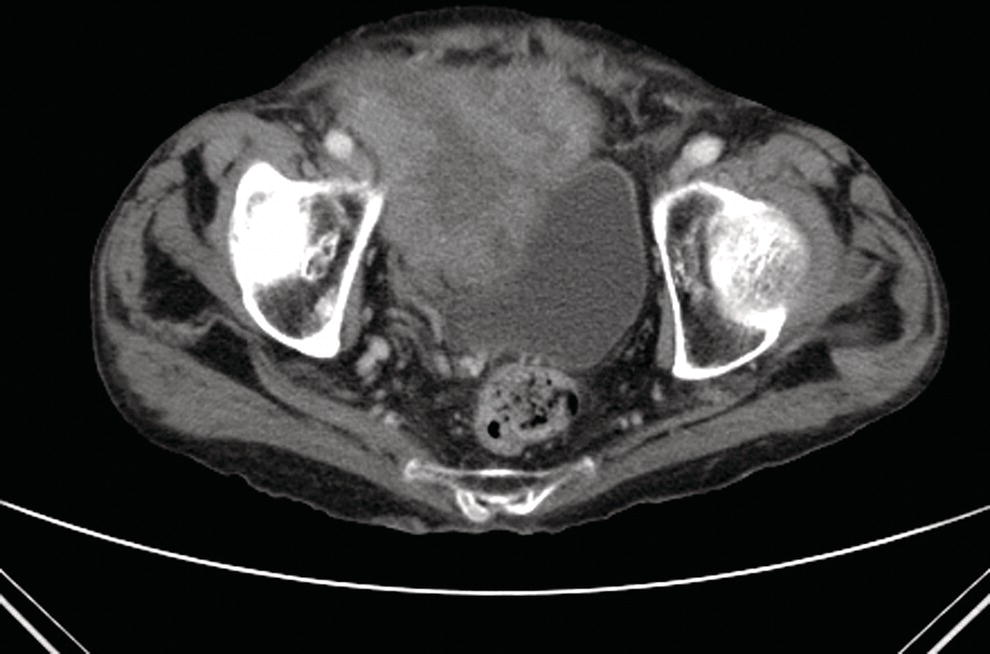
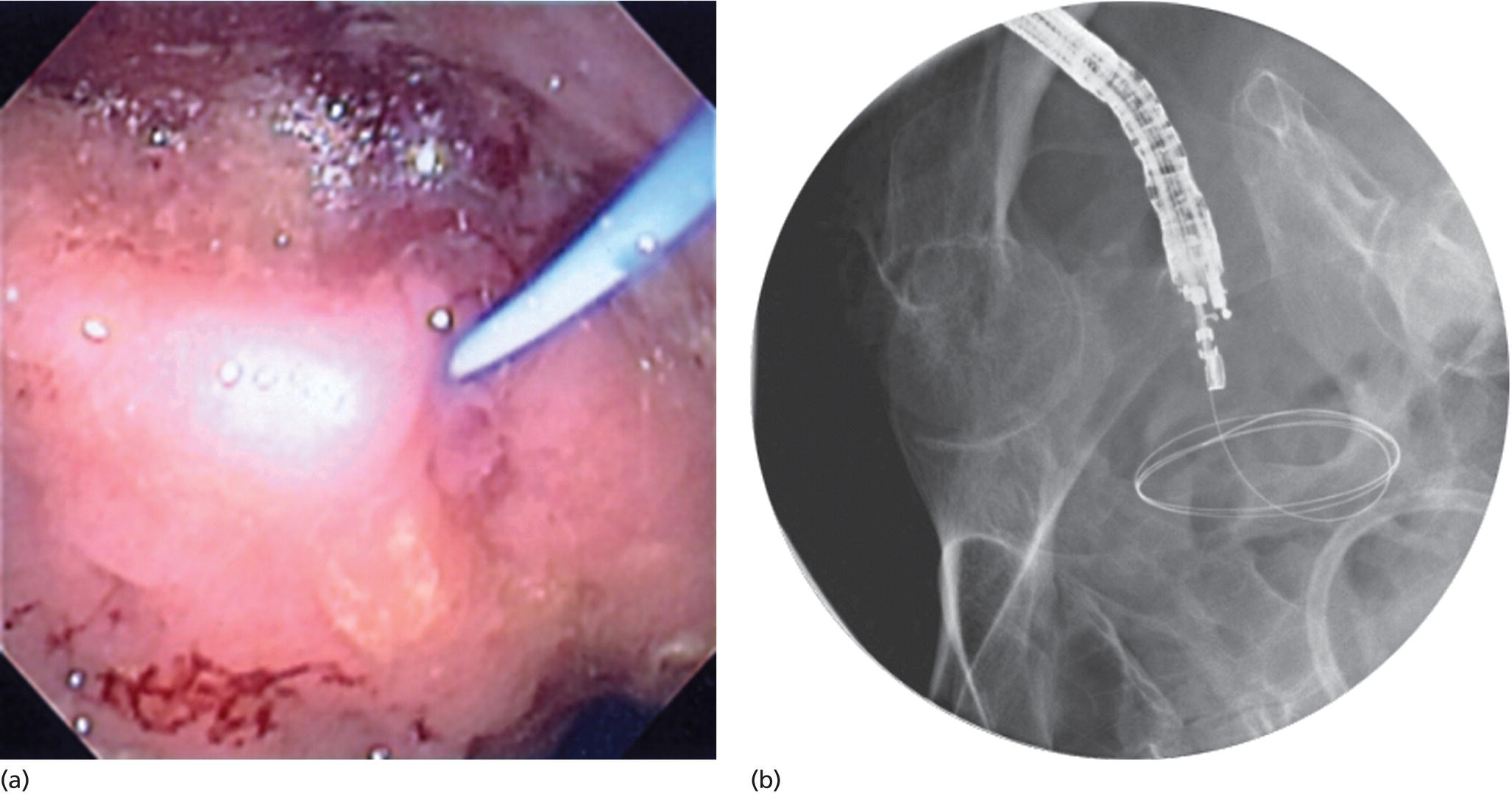
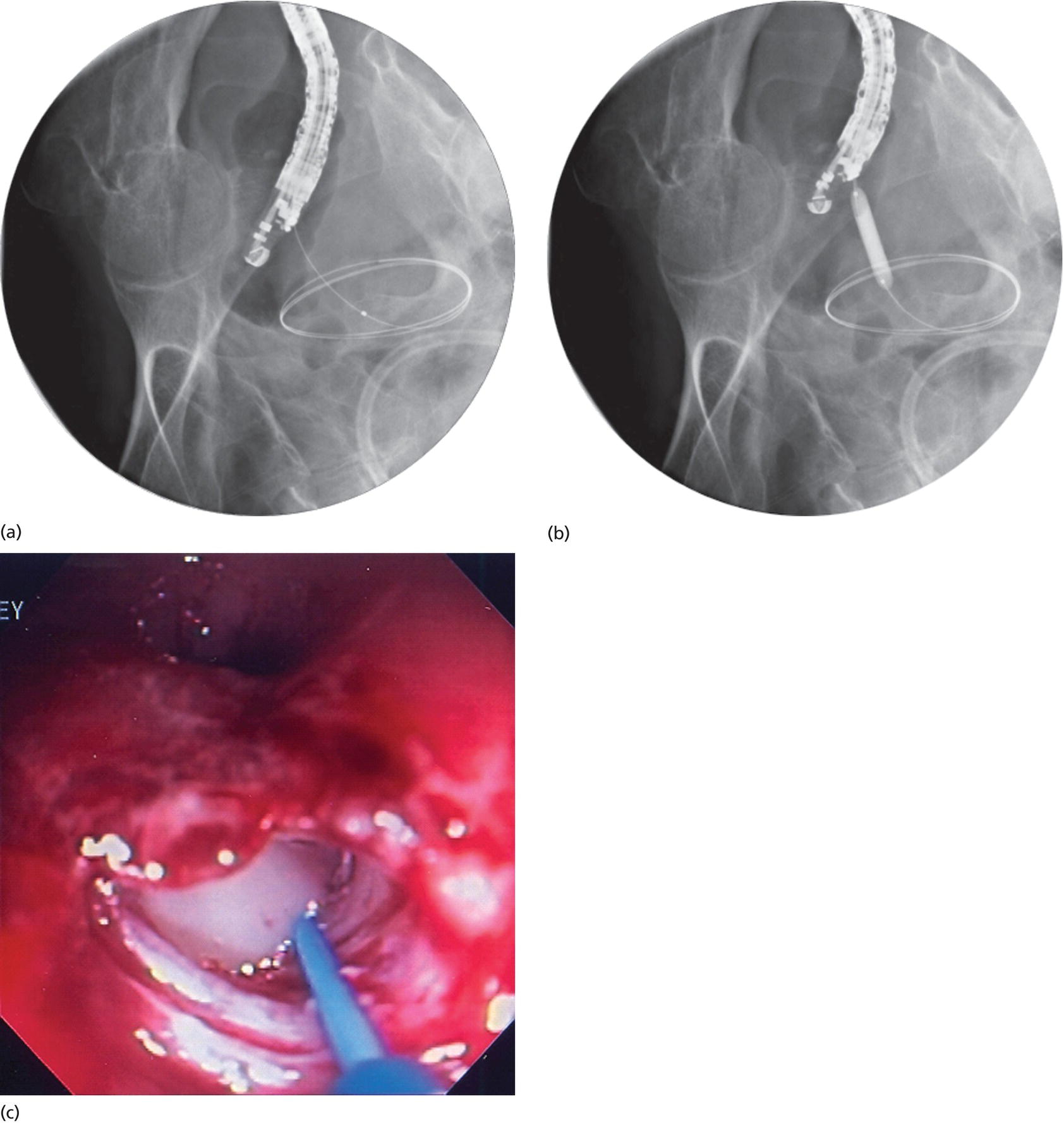
Shyam Varadarajulu1 and Sandeep Lakhtakia2 1 University of Alabama at Birmingham School of Medicine, Birmingham, AL, USA 2 Asian Institute of Gastroenterology, Hyderabad, India Development of pelvic abscess is a well‐recognized complication in patients undergoing low anterior resection for rectal cancer or following medical conditions such as inflammatory bowel disease. Traditionally, these abscesses are drained surgically or image guided (ultrasound or computed tomography [CT]) via the percutaneous, transrectal, or transvaginal routes. Although effective, surgical drainage is associated with a prolonged hospital stay, particularly when performed to manage a postoperative complication. The percutaneous drainage technique is less invasive than surgery but limits patient mobility and predisposes to fistula formation and infection. Also, the complex anatomy of the pelvis with surrounding bones, vascular structures, and other organs makes percutaneous access to the abscess cavity a technical challenge. By virtue of its ability to image and access extraluminal lesions, endoscopic ultrasound (EUS) has emerged as a minimally invasive therapeutic alternative for drainage of pelvic abscesses. A CT of the pelvis must be obtained to get a clear understanding of the abscess location prior to performing pelvic abscess drainage (Figure 38.1). Patients should be administered prophylactic antibiotics prior to the intervention and continued on oral antibiotics for two to three days. Bowel preparation with polyethylene glycol solution or enema is mandatory to minimize the chance of contamination and for adequate visualization. The procedure is best performed under fluoroscopy to visualize guidewire exchange and placement of stent or drain within the abscess. Patients should be instructed to void urine before the procedure as a distended bladder may impair visualization of small abscesses during EUS. A therapeutic linear array echoendoscope with a working channel of 3 mm or more should be used to facilitate deployment of transluminal stents or drainage catheter. A 19‐gauge EUS‐guided fine needle aspiration (FNA) needle is required for transluminal puncture into the abscess cavity, followed by passage of a 0.035‐inch guidewire allowing it to coil inside the abscess cavity. A standard 4.5/5.0 French (Fr) endoscopic retrograde cholangiopancreatography (ERCP) cannula or a needle knife catheter is then railroaded over the guidewire into the abscess cavity. An over‐the‐wire balloon dilator (8–15 mm) is needed for subsequent dilation of the transmural tract. A double pigtail plastic stent (7 or 10 Fr) or drainage catheter is required to facilitate evacuation of the abscess cavity. The following steps are undertaken in sequence (Video 38.1). Figure 38.1 Computed tomography (CT) scan of the pelvis revealing an 8 × 7 cm abscess cavity. Figure 38.2 Passage of a 19‐gauge fine needle aspiration (FNA) needle into the pelvic abscess under EUS guidance. Figure 38.3 A 0.035‐inch guidewire is then coiled within the abscess cavity: (a) endoscopy view; (b) confirmed by fluoroscopy. Figure 38.4 Fluoroscopy view revealing dilation of the tract using an endoscopic retrograde cholangiopancreatography (ERCP) cannula (a) and then an over‐the‐wire balloon dilator (b). Pus is seen to extrude following dilation of the transmural tract (c). In our experience with a carefully selected cohort of 25 consecutive patients, i.e. those with unilocular collections adjacent to the rectum or left colon, EUS‐guided pelvic abscess drainage yielded a successful outcome in 96% of cases. No procedural complications were encountered and, unlike surgical or percutaneous techniques, patients were discharged home within two to three days following their procedures. In contrast to surgery and percutaneous techniques, EUS‐guided drainage of pelvic abscess is less invasive, less costly, and is associated with minimal patient discomfort. We recently compared the outcomes between transcolonic and transrectal drainage of pelvic abscesses in 38 patients and observed no difference in rates of technical success, treatment success, or complications between both approaches. However, when evaluated by etiology, treatment success for diverticular abscess was significantly lower when compared with other causes. Figure 38.5 Fluoroscopic view revealing the presence of a stent within the pelvic abscess cavity. Drainage of pelvic abscess cannot be undertaken when the wall of the abscess cavity is more than 20 mm from the EUS transducer. Also, the presence of multiple cavities in an abscess precludes successful drainage. It is important to carry out a helical CT scan before embarking on this procedure because poorly defined or multilocular fluid collections are not suitable for this non‐surgical method of drainage. Also, stent deployment may not be possible in patients with pelvic abscesses that measure less than 4 cm in size. As the linear array echoendoscope can be advanced only up to 40 cm in the colon, only those fluid collections adjacent to the rectum or left colon can be drained using this technique. Perianal fluid collections are not suitable for EUS‐guided drainage. Endoscopic ultrasound‐guided drainage can be an effective treatment modality for management of patients with abscesses or fluid collections in the pelvis that are within the reach of the echoendoscope. Comparative studies with other treatment modalities that include a larger number of patients will help identify cases that will benefit the most from this technique.
38
How to do EUS‐guided Pelvic Abscess Drainage
Introduction
Patient preparation
Devices and accessories
Procedural technique

Clinical outcomes

Technical limitations
Conclusions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








