Sammy Ho Montefiore Medical Center/AECOM, Bronx, NY, USA The approach to biopsy lesions in the mediastinum has changed over time. Invasive mediastinoscopy and thoracotomy have limited role for tissue acquisition, particularly in the posterior mediastinum, due to the increased use of endoscopic ultrasound‐guided fine needle aspiration (EUS‐FNA). Most recent literature has demonstrated its overall safety, reliability, and accuracy. There is convincing evidence that EUS‐FNA is an accurate method for mediastinal staging in patients with non‐small cell lung cancer (NSCLC), which has become the main indication for transesophageal EUS‐FNA (Table 30.1). Attempts should be made to review cross‐sectional imaging prior to EUS‐FNA, often using a computed tomography (CT) scan of the thorax, to help formulate a plan for targeted tissue acquisition as well as characterizing any anatomic aberrancies. Due to the duration of the time spent with echoendoscope in the esophagus during mediastinal FNA, proper sedation is imperative as is vigilance for periprocedural aspiration. Sudden movements have to be avoided to prevent injuries. Suctioning of the stomach for secretions and minimal use of air and water instillation within the esophagus should reduce the risk of aspiration. The same linear‐array echoendoscope equipment that is used in other parts of the gastrointestinal (GI) tract is utilized for the assessment of mediastinal lesions. The transducer is positioned in the esophagus to examine the posterior mediastinum. Tip of the echoendoscope is adjusted to view the ventral aspect toward 12 o’clock, the dorsal aspect toward 6 o’clock, the cranial toward 9 o’clock, and the caudal toward 3 o’clock position on the screen. Evaluation of the mediastinum using the linear‐array echoendoscope should follow a standardized approach. Beginning with the tip of the echoendoscope in the proximal stomach, the celiac nodes and left adrenal gland can be inspected. The mediastinum is surveyed by first finding the descending aorta. Slow withdrawal of the echoendoscope in 3–4 cm increments and 360‐degree rotations can encompass the entire posterior mediastinum. When the transducer is positioned on the posterior and left side of the esophagus, it is possible to examine the thoracic aorta, the left pleura, and the left lung. When the transducer is positioned on the right side of the esophagus, one can visualize the azygos vein as far as its arch, situated between 24 and 25 cm from the incisors. By having the transducer pointing toward the anterior side of the esophagus in the middle part of the posterior mediastinum, the cardiac region can be examined, including the left atrium, the left ventricle, the pulmonary artery, and the aortic root. Most of the mediastinal lesions are in close proximity to the esophageal wall. Hence, positioning of the echoendoscope to enable visualization and sampling is relatively easier than in other areas of the GI tract. It is important to have an excellent apposition of the tip of the instrument with the wall of the esophagus to avoid “recoil” of the echoendoscope. The actual EUS‐FNA technique is similar to the one used in other areas in the GI tract. Generally, in the medistinum, one to three needle passes are sufficient to obtain adequate material. Presence of vessels in the needle path is a contraindication to EUS‐FNA, and this possibility can be effectively excluded using color or power Doppler. Lymph nodes in the mediastinum are classified according to the American Thoracic Society mediastinal staging map for lymphadenopathy (Figure 30.1). The nodal stations amendable to EUS‐FNA, from inferior to superior, include the pulmonary ligament (stations 9R and 9L), lower paraesophageal (stations 8R and 8L), subcarinal (station 7), AP window (station 5), and para‐aortal (station 6) nodes. When more than one lymph node group is present, the clinically most important location that is also accessible is selected. If two lesions in anatomically different areas are to be sampled, it is advisable to use two different needles, to avoid cross‐contamination and possible misinterpretation of results. Table 30.1 TNM staging system for lung cancer (7th edition). Source: adapted from Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groups in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol 2007;2:706. Figure 30.1 The International Association for the Study of Lung Cancer (IASLC) lymph node map, including the proposed grouping of lymph node stations into “zones” for the purposes of prognostic analyses. Source: Rusch VW, Asamura H, Watanabe H, et al. The IASLC Lung Cancer Staging Project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4(5):568–577. © 2009, Elsevier.
30
How to do Mediastinal FNA
Primary tumor (T)
T1
Tumor ≤3 cm diameter, surrounded by lung or visceral pleura, without invasion more proximal than lobar bronchus
Tumor ≤2 cm in diameter
Tumor >2 cm but ≤3 cm in diameter
T2
Tumor >3 cm but ≤7 cm, or tumor with any of the following features:
Involves main bronchus, ≥2 cm distal to carina
Invades visceral pleura
Associated with atelectasis or obstructive pneumonitis that extends to the hilar region but does not involve the entire lung
Tumor >3 cm but ≤5 cm
Tumor >5 cm but ≤7 cm
T3
Tumor >7 cm or any of the following:
Directly invades any of the following: chest wall, diaphragm, phrenic nerve, mediastinal pleura, parietal pericardium, main bronchus <2 cm from carina (without involvement of carina)
Atelectasis or obstructive pneumonitis of the entire lung
Separate tumor nodules in the same lobe
T4
Tumor of any size that invades the mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, carina, or with separate tumor nodules in a different ipsilateral lobe
Regional lymph nodes (N)
N0
No regional lymph node metastases
N1
Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension
N2
Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s)
N3
Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s)
Distant metastasis (M)
M0
No distant metastasis
M1
Distant metastasis
Separate tumor nodule(s) in a contralateral lobe; tumor with pleural nodules or malignant pleural or pericardial effusion
Distant metastasis
Stage groupings
Stage IA
T1a–T1b
N0
M0
Stage IB
T2a
N0
M0
Stage IIA
T1a, T1b, T2a
N1
M0
T2b
N0
M0
Stage IIB
T2b
N1
M0
T3
N0
M0
Stage IIIA
T1a, T1b, T2a, T2b
N2
M0
T3
N1,N2
M0
T4
N0,N1
M0
Stage IIIB
T4
N2
M0
Any T
N3
M0
Stage IV
Any T
Any N
M1a or M1b 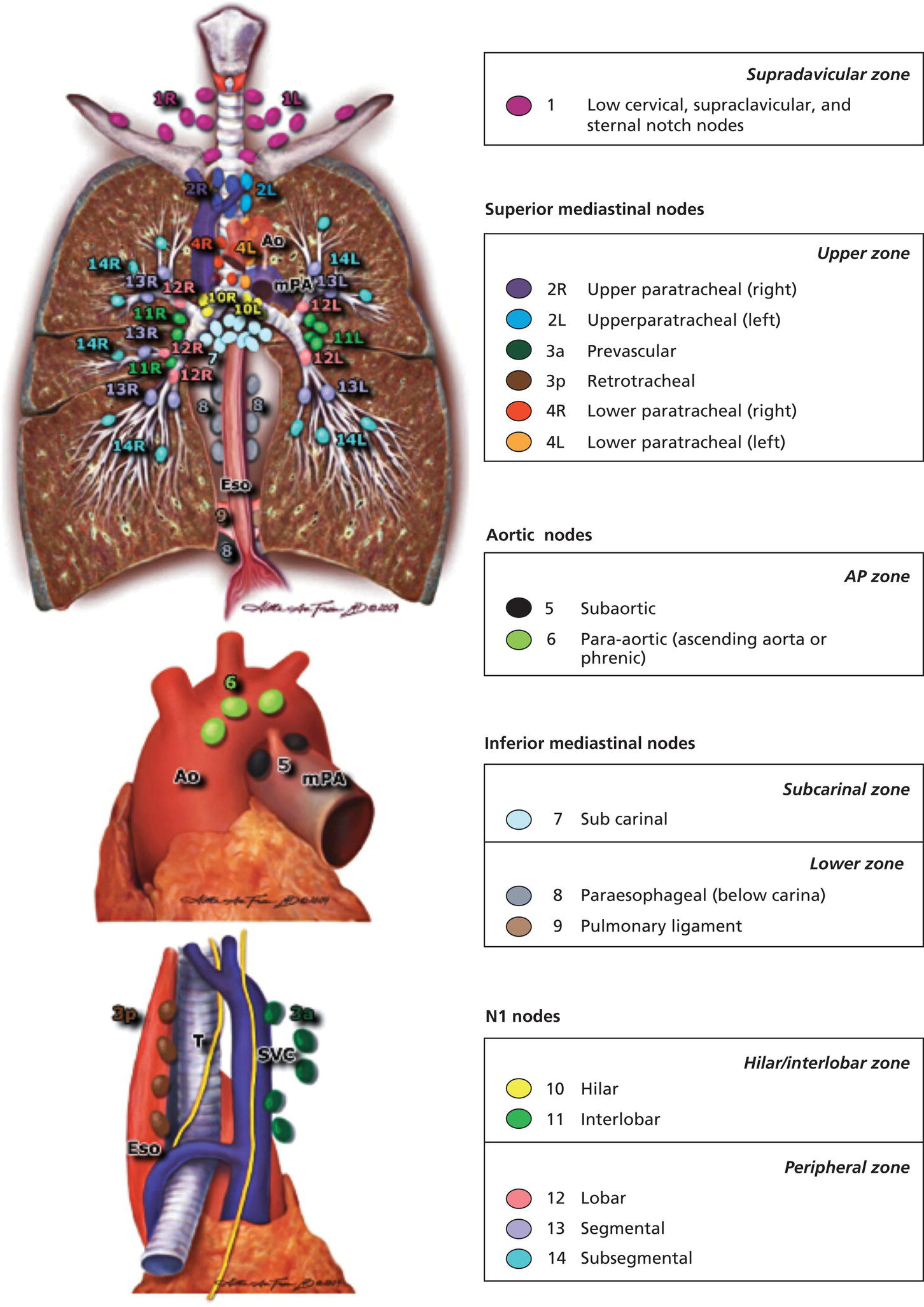
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree