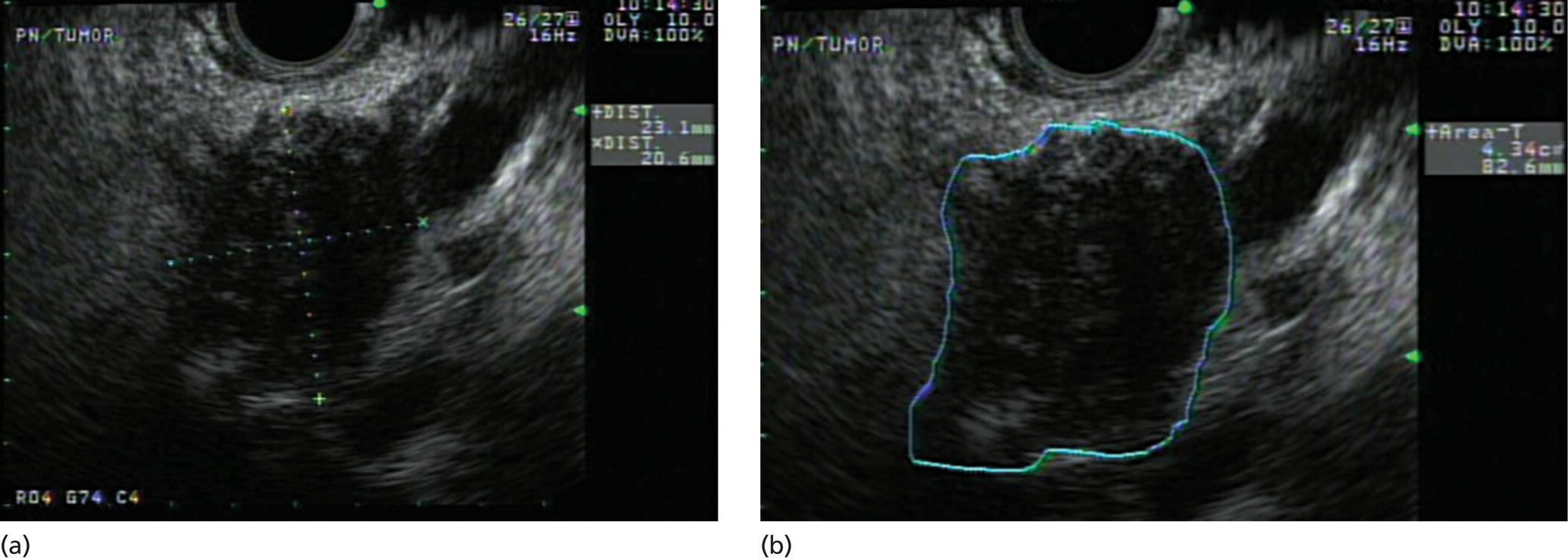
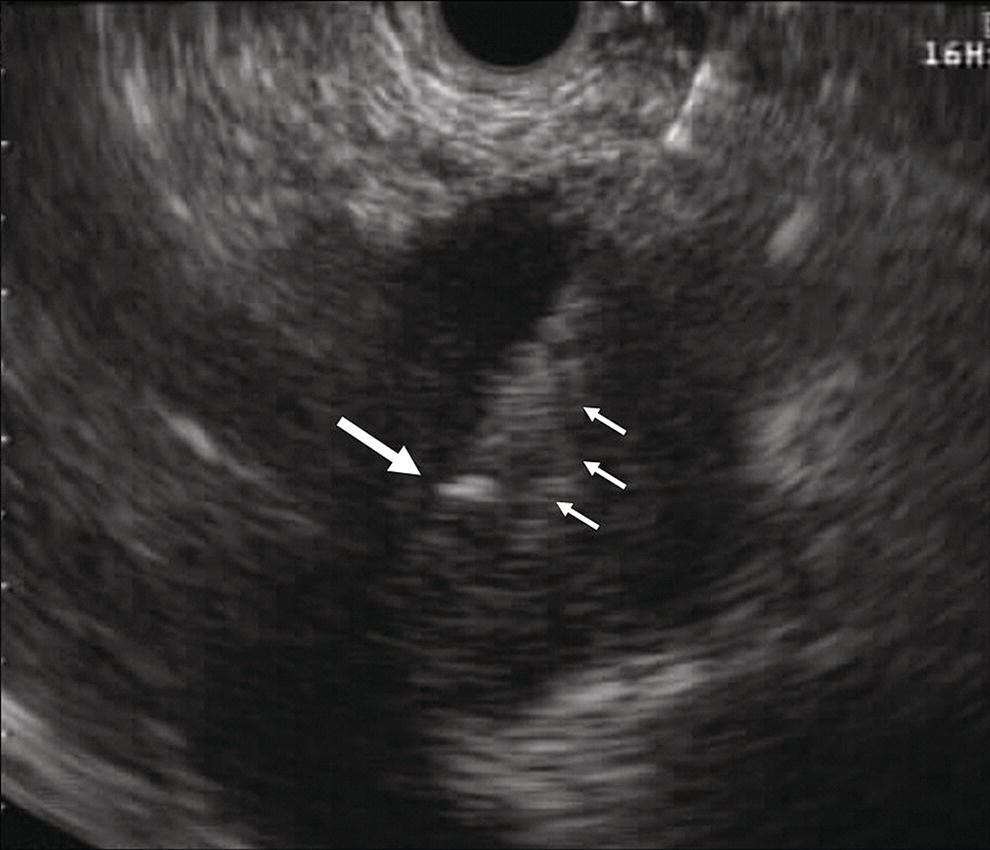
V. Raman Muthusamy and Kenneth J. Chang University of California, Irvine, Orange, CA, USA Endoscopic ultrasound (EUS)‐guided fine needle injection (FNI) has been used to directly administer chemotherapeutic agents within pancreatic and esophageal tumors. Agents used to date include an allogeneic mixed lymphocyte culture and antitumor viral therapy using viral vectors encoding tumor necrosis factor (TNF)‐α or granulocyte‐macrophage colony‐stimulating factor (GM‐CSF). These agents can directly or synergistically assist in achieving tumor lysis. We describe here our specific technique for performing such procedures in pancreatic tumors using TNFerade™ (GenVec Inc., Gaithersburg, MD), a replication‐deficient adenovector encoding human TNF‐α and regulated by a radiation inducible promoter Egr‐1, although the technique is similar for other antitumor agents. Prior to each TNFerade injection, which requires five weekly injections in conjunction with chemoradiation therapy, attire approved by the institutional biosafety committee should be worn by all personnel involved in the procedure, given that a viral vector is being utilized. Typical gear includes material that achieves complete head covering, safety goggles, specially fitted masks to form a complete oral/facial shield, a gown, and gloves. The TNFerade solution is prepared by the pharmacy and is provided to the gastrointestinal laboratory immediately prior to the procedure. We typically use a 22‐gauge fine needle aspiration (FNA) needle (EchoTip™, Cook Medical, Bloomington, IN) to administer the antitumor agent. Prior to inserting the FNA needle into the biopsy channel of the echoendoscope, we remove the stylet within the needle. For TNFerade, in which 2.0 ml is actually injected into the tumor, a total of 2.6 ml is usually provided in a 3.0‐ml syringe by the pharmacy so that the entire needle channel can be primed prior to intratumoral injection. This is accomplished by attaching the 3.0‐ml syringe to the FNA needle via the Luer lock on the handle. The needle is then primed by injecting the therapeutic agent into the needle until the entire dead space of the needle (usually 0.2–0.4 ml) contains fluid and fluid is witnessed exiting the needle tip. Fluid injection is then continued until exactly 2 ml remains in the syringe, at which point the needle is ready for use. Once the needle enters the tumor, the remainder of the fluid in the syringe is injected so that exactly 2 ml is delivered intratumorally. We use a standard linear array echoendoscope (GFUC‐140P, Olympus America, Center Valley, PA), operating at 5 MHz frequency to achieve maximal imaging depth, to perform all EUS‐guided FNI procedures. Prior to FNI of the tumor, we routinely assess the lesion at its maximal cross‐section and measure its size, circumference and area, and estimate tumor volume (Figure 37.1). This is important initially to set a baseline tumor size and during subsequent weekly injections to assess tumor response or progression. We also perform a careful standard EUS exam to assess for the presence or development of metastatic disease. A detailed review of previous images/videos is critical to ensure comparable regions are measured during subsequent exams in order to measure tumor response. We have noted that as therapy progresses, the echotexture within the tumor may become brighter, possibly indicating the development of fibrosis within the treated lesion. We believe this finding corresponds to a region of the tumor that has achieved a good response to therapy. Areas that are anechoic often indicate a region of tumor necrosis. In contrast, we believe that portions of the lesion that are hypoechoic represent residual areas of viable tumor. Our technique of EUS‐guided FNI involves identifying the most hypoechoic area(s) of the lesion to inject. Once the target has been identified, we place the 22‐gauge needle into the biopsy channel of the echoendoscope and Luer‐lock it in place. We then line up the needle‐tip to the targeted (hypoechoic) area of the lesion. Having an assistant hold the echoendoscope to stabilize its position at this juncture is often helpful. We then slowly advance the needle deep into the lesion using standard EUS‐guided FNA technique. Upon reaching the deepest portion of the lesion, we slowly withdraw the needle and slowly inject the therapeutic agent into the well created by the FNA needle. A gradual, methodical withdrawal and injection is recommended to keep the entire injected solution within the tumor. We avoid injecting into anechoic (necrotic) regions and only inject on withdrawal (Figure 37.2). The needle can be realigned and redirected into other hypoechoic areas of the tumor in a fan‐like fashion (Video 37.1). This is done by changing the angle of the elevator when the needle has reached the superficial portion of the tumor (that closest to the gastrointestinal lumen on imaging) and re‐advancing the needle into a new portion of the tumor. Again, withdrawal is done slowly and injection is performed during needle withdrawal only. This process can be repeated until the entire 2 ml in the syringe has been injected, at which time the needle is removed from the lesion and withdrawn from the echoendoscope and the procedure is complete. A typical intratumoral injection lasts only two to three minutes in duration. Figure 37.1 Initial assessment of tumor size by endoscopic ultrasound (EUS) imaging. (a) Measurement of the tumor in maximal cross‐section on EUS imaging prior to injection therapy. (b) This image highlights the ability of EUS to measure tumor area and circumference and, using this data, even estimate volume. Source: Chang KJ, Lee JG, Holcombe RF, et al. Endoscopic ultrasound delivery of an antitumor agent to treat a case of pancreatic cancer. Nature Clin Pract Gastroenterol Hepatol 2008;5:107–111. Figure 37.2 Endoscopic ultrasound (EUS)‐guided fine needle injection (FNI) of a pancreatic lesion using a 22‐gauge needle. The needle tip (large arrow) and the blush resulting from the injection of the chemotherapeutic agent around the needle (small arrows) can be seen. Source: Chang KJ, Lee JG, Holcombe RF, et al. Endoscopic ultrasound delivery of an antitumor agent to treat a case of pancreatic cancer. Nature Clin Pract Gastroenterol Hepatol 2008;5:107–111. Antibiotics are administered orally three hours before the procedure and at 12 and 24 hours after the procedure. We typically administer a 500‐mg dose of oral ciprofloxacin at these time points. The patient is recovered in a standard fashion in the endoscopy unit and then discharged to receive chemoradiation therapy. We believe that careful attention to chemotherapeutic injection technique is essential to achieving maximal results with these agents. An example of a vigorous response to such therapy is illustrated in Figures 37.3–37.5, which show a dramatic weekly reduction in size of a pancreatic tumor (Figure 37.3), with no residual tumor present in the gross resected specimen (Figure 37.4) or on histology (Figure 37.5).
37
How to Inject Chemotherapeutic Agents
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








