Secondary prevention
Primary prevention
Potential arbitrators
Cardiac arrest/sustained VT
Family history of SD
LV apical aneurysms
Syncope
End-stage phase
Massive LVH >30 mm
LGE
NS VT at Holter
LV obstruction
Abnormal exercise BP response
13.2 Left Ventricular Hypertrophy
Being that LV hypertrophy a hallmark of HCM, the degree of LV wall thickness has been tested in several studies as a possible risk factor for adverse outcome. In a large patient population, Spirito et al. [3] demonstrated that the magnitude of hypertrophy is directly related to the risk of SD and is a strong and independent predictor of prognosis. Young patients with extreme hypertrophy (end-diastolic wall thickness ≥30 mm) assessed at M-mode and 2D echocardiography, even those with few or no symptoms, appeared to be at substantially increased long-term risk, deserving consideration for interventions to prevent SD. Elliott et al. [4] found that patients with LV wall thickness ≥30 mm had a higher probability of SD or implanted cardiac defibrillator (ICD) discharge than other HCM patients; however, when considered together, the number of additional risk factors (one to three) was a better predictor of risk than wall thickness alone.
In conclusion, and according to the most recent guidelines [5], severe LV hypertrophy is one of the main factors to be considered for ICD implantation for primary prevention of SD.
13.3 Diastolic Dysfunction
Various degrees of diastolic dysfunction are common in HCM. If severe, it is a marker of adverse outcome. In particular, restrictive filling pattern (RFP) is quite uncommon in HCM, but its evaluation adds prognostic power to the stratification of the patients, as demonstrated by our group [6]. Furthermore, Biagini et al. [7] demonstrated that RFP is a hallmark of severe phenotype, being a strong predictor of SD and progression to end-stage hypokinetic evolution of the disease. In this setting, tissue Doppler imaging (TDI) plays a role—especially in asymptomatic or mildly symptomatic patients—in predicting cardiovascular events. In particular, E wave to E’ ratio (E/E’) was demonstrated as an independent predictor of adverse outcome [8].
The prognostic role of right ventricular (RV) diastolic function was analyzed in patients with HCM by Pagourelias et al. [9]. Patients presenting with increased RV E/E’ ratio (ratio of tricuspid in flow E wave to E’ wave obtained by TDI at the lateral tricuspid annulus) had a 1.6-times greater risk for HF mortality, whereas patients with shortened tricuspid E wave deceleration time had a 1.1 greater risk for SD.
13.4 Left Atrial Size
LA size is associated with an adverse prognosis in various cardiovascular diseases [10]. In HCM, LA enlargement is common, is associated with several adverse pathophysiologic consequences such as LV OT obstruction, and is predictive of atrial fibrillation (AF), which is a major predictor of adverse outcome [11]. Nistri et al., using data from an Italian multicentric registry, demonstrated on a large population of patients with HCM (n = 1,491) that LA dimension is an independent marker of prognosis, particularly relevant in identifying patients at risk for HF-related death [12]. These results were confirmed by studies that considered the independent role of LA diameter in predicting death in the very-long-term follow-up [13].
13.5 Left Ventricular Obstruction
Another feature that frequently affects HCM patients is LV obstruction [14]. As demonstrated by Maron et al. [15] in a population of 1,101 HCM patients, LV OT obstruction is a major risk factor for death related to HCM, stroke, or HF and progression to New York Heart Association (NYHA) class III or IV. The role of LV obstruction in predicting SD is more heatedly debated. Elliott and coworkers [16] reported that it was associated with an increased risk of SD/ICD discharge that was related to obstruction severity and the presence of other recognized risk factors. Conversely, Efthimiadis et al. [17] found that LV OT obstruction did not emerge as an independent predictor of SD. Obstacles to outflow obstruction as a primary risk factor include its dynamic nature, and the high frequency of obstruction encountered in the HCM patient population [15].
13.6 Evolution During Follow-up
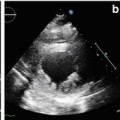
HCM can have a highly variable course. Whereas the majority of patients remain stable during the follow-up, some experience adverse LV remodeling with progressive reduction of systolic function (end-stage disease) [18]. In this setting cardiac imaging is pivotal for monitoring during follow-up. As shown by our group [19], of 101 patients affected by HCM and with long-term follow-up, the number of patients who evolve toward systolic or diastolic dysfunction is not negligible (28 and 16 %, respectively). Taking follow-up evaluation into consideration adds accuracy to the general prognostic assessment of the disease.
The outcome of HCM patients in end-stage disease is particularly severe, not only due to high rates of HF-related complications and mortality but because of a considerable incidence of SD [20]. Consequently, accurate and prompt diagnosis of this condition is important and can affect the general therapeutic management (possible indications to ICD, cardiac resynchronization therapy (CRT), heart transplantation).
13.7 Late Gadolinium Enhancement
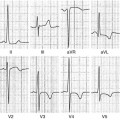
Cardiac magnetic resonance (CMR) may add important information to the prognostic assessment of HCM patients. In particular, fibrosis, as assessed by late gadolinium enhancement (LGE), is hypothesized to be related to SD. Recent cross-sectional studies demonstrated a strong association between LGE and ventricular tachyarrhythmias on ambulatory Holter electrocardiography (ECG) [21–23]. Adabag et al. [24] found that LGE was an independent risk factor for ventricular arrhythmias and conferred a 7.3-fold [95 % confidence interval (CI) 2.6–20.4; p < 0.0001] increased relative risk (RR) of nonsustained ventricular tachycardia (VT), a potential risk factor for SD in HCM. O’Hanlon et al. [21] examined the significance of fibrosis detected by LGE-CMR for predicting major clinical events. Cox proportional hazards modeling revealed the amount of fibrosis to be a significant independent predictor of the primary composite endpoint (cardiovascular death, unplanned cardiovascular hospitalization, sustained VT, ventricular fibrillation, appropriate ICD discharge). Todiere et al. [25] analyzed a cohort of 55 HCM patients with two CMR at an interval of 719 ± 410 days, focusing on LGE progression rate during follow-up. The majority of patients showed a progressive increase in LGE over time, and patients with worsened NYHA functional class presented higher a LGE increase.
Whereas LGE has been identified as a marker of adverse prognosis [22], to date, there is a lack of robust evidence about its role as a predictor of SD in HCM. As a result, recommendations for primary prevention ICDs should not be based solely on the presence of LGE in individual patients. In the most recent HCM guidelines, LGE is classified as an arbitrator, useful in SD prognostic stratification in cases in which the indication for ICD implantation is not clear from conventional risk factors. Another point of discussion regards the extent and site of LGE and the relationship with clinical outcome. In fact, the majority of follow-up studies considered only the presence of LGE rather than its characteristics.
13.8 Microvascular Dysfunction
Microvascular dysfunction is a common feature of HCM, and positron emission tomography (PET) is a reliable method by which to assess it [26]. Cecchi et al. [27], in a PET study of 51 HCM patients, demonstrated that the degree of microvascular dysfunction, assessed using myocardial blood flow values after dipyridamole infusion, is a strong, independent predictor of clinical deterioration and death. Moreover, Olivotto et al. [28] reported severe microvascular dysfunction as being a potent long-term predictor of adverse LV remodeling and systolic dysfunction in HCM, which is thus is a potential target for preventing disease progression and HF in HCM.