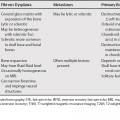
68 The primary etiologies of hypervascular liver lesions are the hypervascular primary liver lesions and hypervascular metastases. Renal cell cancer, breast cancer, thyroid cancer, melanoma, carcinoid, islet cell, and sarcomas are the most common hypervascular liver metastases.1 Small hemangiomas that demonstrate flash filling during early phase imaging can sometimes appear as small hypervascular lesions. The most common etiologies for a solitary large hypervascular mass in the absence of a primary malignancy are focal nodular hyperplasia (FNH), hepatic adenoma and hepatocellular carcinoma (HCC). Many HCCs can be differentiated on the basis of aggressive features and clinical setting. FNH and adenomas both occur in young and middle-aged women and adenomas are seen in the setting of oral contraceptive use. Multiple imaging features are helpful for differentiating the two lesions (Table 68.1). A FNH with a central scar may be difficult to differentiate from a fibrolamellar carcinoma (see Chapter 70) and hepatic adenomas usually cannot be differentiated from low-grade HCCs. Specific magnetic resonance imaging (MRI) contrast agents may be helpful in differential diagnosis. Gadobenate dimeglumine (Multi-hance, Bracco Imaging, Milan, Italy) differs from conventional gadolinium-based agents as 3 to 5% of the dose is eliminated through the hepatobiliary pathway. As hepatic adenomas lack bile ducts they are hypointense on delayed (1 to 3 hours) images after gadobenate dimeglumine images. Focal nodular hyperplasia contains malformed biliary ductules and almost all lesions will be hyperintense or isointense to liver on delayed images.2 Gadobenate dimeglumine is superior to superparamagnetic iron oxide (SPIO) particles for characterizing FNH,3 as FNH and adenomas may have a comparable degree of SPIO uptake.4
Hypervascular Liver Lesions
| FNH | Adenoma | |
|---|---|---|
| Central scar | + | – |
| Heterogeneous enhancement | – | + |
| Heterogeneous intensity | – | + |
| Subcapsular feeding arteries | – | + |
| Degree of arterial phase enhancement* | > | < |
| Hemorrhage | – | +/– |
| T1WI hyperintensity | +/– | +/– |
| Delayed gadobenate dimeglumine uptake | + | – |
Abbreviations: FNH, focal nodular hyperplasia; T1WI, T1-weighted magnetic resonance imaging.
* FNH has a greater degree of enhancement than adenoma in the arterial phase. FNH has an enhancement ratio of >1.6 (arterial phase attenuation compared with noncontrast attenuation) compared <1.6 for adenomas. However, in the portal phase FNH is often isodense; adenomas are often hyperdense.20
Features of Specific Hypervascular Liver Lesions
Regenerative Nodules in Budd-Chiari Syndrome
Benign regenerative hepatic nodules have been described in Budd-Chiari syndrome, which are multiple, small, and hypervascular. These are likely a result of insufficient blood supply to portions of the liver that will atrophy, with compensatory nodular hyperplasia in areas of the liver with adequate blood supply. These nodules have also been reported in other systemic disorders, which impair hepatic blood flow, such as autoimmune disease, lympho- and myeloproliferative disorders, and after treatment with steroids and antineoplastic medications.5 Similar nodules have also been described in autoimmune hepatitis.6 These regenerative nodules are distinct from nodular regenerative hyperplasia (see Chapter 73)7 in which there is no fibrosis between the nodules. These nodules can have central scars, especially if >
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree