2 Ventricles and Cisterns(Table 2.1 – Table 2.4)
Age | Foramen of Monro | Trigone and Atrium | Lateral Ventricle, Body |
Adult | Colloid cyst Cysticercosis Meningioma Choroid plexus cyst Neuroepithelial cyst Central neurocytoma Metastasis Neuroepithelial cyst Cysticercosis | Ependymoma Glioblastoma Metastasis Central neurocytoma Cysticercosis | |
Child (> 5 y) | Giant cell astrocytoma Pilocytic astrocytoma Cysticercosis | Ependymoma Choroid plexus cyst Choroid plexus papilloma Choroid plexus carcinoma Hamartoma/tuberous sclerosis Gray matter heterotopia Cysticercosis | Ependymoma Pilocytic astrocytoma Hamartoma/tuberous sclerosis Gray matter heterotopia Cysticercosis |
Child (< 5 y) | Giant cell astrocytoma Pilocytic astrocytoma Cysticercosis | Choroid plexus papilloma Choroid plexus carcinoma Cysticercosis | Choroid plexus papilloma Choroid plexus carcinoma Primitive neuroectodermal tumor (PNET) Teratoma Cysticercosis |
Age | Foramen of Monro | Anterior Recess | Third Ventricle, Body | Third Ventricle, Posterior |
Adult | Colloid cyst Metastases Cysticercosis | Pituitary adenoma Meningioma Metastasis Aneurysm Craniopharyngioma Lymphoma Cysticercosis | Glioma Cysticercosis | Pineal tumor Glioma Vascular malformation Cysticercosis |
Child | Giant cell astrocytoma Pilocytic astrocytoma Cysticercosis | Germ cell tumor Langerhans cell histiocytosis Glioma Craniopharyngioma Cysticercosis | Choroid plexus papilloma Glioma Cysticercosis | Pineal tumor Glioma Vascular malformation Cysticercosis |
Lesions | CT Findings | Comments |
Child | ||
Astrocytoma | Low-grade astrocytoma: Focal or diffuse mass lesion usually located in the cerebellar white matter or brainstem with low to intermediate attenuation, with or without mild contrast enhancement. Minimal associated mass effect. May extend into ventricles. | Often occurs in children and adults (age 20–40 y). Tumors comprised of well-differentiated astrocytes. Association with neurofibromatosis type 1; 10-y survival common; may become malignant. |
| Juvenile pilocytic astrocytoma subtype: Solid/cystic focal lesion with low to intermediate attenuation, usually with prominent contrast enhancement. Lesions located in the cerebellum and brainstem. May extend into ventricles. | Common in children; usually favorable prognosis if totally resected. |
| Gliomatosis cerebri: Infiltrative lesion with poorly defined margins with mass effect located in the white matter, with low to intermediate attenuation; usually no contrast enhancement until late in disease. Anaplastic astrocytoma: Often irregularly marginated lesion located in white matter with low to intermediate attenuation, with or without contrast enhancement. May extend into ventricles | Diffusely infiltrating astrocytoma with relative preservation of underlying brain architecture. Imaging appearance may be more prognostic than histologic grade; ~2-y survival. Intermediate between low-grade astrocytoma and glioblastoma multiforme; ~2-y survival. |
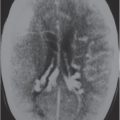
Medulloblastoma (primitive neuroectodermal tumor of the cerebellum) | Circumscribed or invasive lesions; low to intermediate and/or slightly high attenuation; variable contrast enhancement; frequent dissemination into the leptomeninges and/or ventricles. | Highly malignant tumors that frequently disseminate along CSF pathways. |
Ependymoma | Circumscribed spheroid or lobulated infratentorial lesion, usually in the fourth ventricle, with or without cysts and/or calcifications; low to intermediate attenuation; variable contrast enhancement; with or without extension through the foramina of Luschka and Magendie. | Occurs more commonly in children than adults; two thirds infratentorial, one third supratentorial. |
Metastatic tumor | Single or multiple well-circumscribed or poorly defined lesions involving the brain stem and cerebellum, skull, dura, leptomeninges, ventricles, choroid plexus, or pituitary gland; low to intermediate attenuation, usually with contrast enhancement, with or without bone destruction, with or without compression of neural tissue or vessels. Leptomeningeal tumor-drop metastasis often best seen on postcontrast images. | May have variable destructive or infiltrative changes involving single or multiple sites of involvement. |
Hemangioblastoma | Circumscribed tumors usually located in the cerebellum and/or brainstem; small contrast-enhancing nodule with or without cyst, or larger lesion with prominent heterogeneous enhancement with or without vessels within lesion or at the periphery; intermediate attenuation; occasionally lesions have evidence of recent or remote hemorrhage. May extend into ventricles. | Multiple lesions occur in adolescents with von HippelLindau disease. |
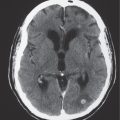
Choroid plexus papilloma or carcinoma | Circumscribed and/or lobulated lesions with papillary projections, intermediate attenuation, usually prominent contrast enhancement, with or without calcifications. Locations: atrium of lateral ventricle (children) > fourth ventricle (adults), rarely other locations such as third ventricle; associated with hydrocephalus. | Rare intracranial neoplasms, Magnetic resonance imaging (MRI) features of choroid plexus carcinoma and papilloma overlap; both histologic types can disseminate along CSF pathways and invade brain tissue. |
Adult | ||
Metastatic tumor | Single or multiple well-circumscribed or poorly defined lesions involving the skull, dura, leptomeninges, brainstem, cerebellum, ventricles, choroid plexus, or pituitary gland; low to intermediate attenuation, usually with contrast enhancement, with or without bone destruction, with or without compression of neural tissue or vessels. Leptomeningeal tumor often best seen on postcontrast images. | May have variable destructive or infiltrative changes involving single or multiple sites of involvement. |
Hemangioblastoma | Circumscribed tumors usually located in the cerebellum and/or brainstem; small contrast- enhancing nodule with or without cyst, or larger lesion with prominent heterogeneous enhancement with or without vessels within lesion or at the periphery; occasionally lesions have evidence of recent or remote hemorrhage; may extend into ventricle. | Occurs in adolescents, young and middle-aged adults. Lesions are typically multiple in patients with von Hippel-Lindau disease. |
Astrocytoma | Low-grade astrocytoma: Focal or diffuse mass lesion usually located in the cerebellum or brainstem with low to intermediate attenuation, with or without mild contrast enhancement. Minimal associated mass effect. May extend into ventricles. | Often occurs in children and adults (age 20–40 y). Tumors comprised of well-differentiated astrocytes. Association with neurofibromatosis type 1; 10-y survival common; may become malignant. |
| Anaplastic astrocytoma: Often irregularly marginated lesion located in the cerebellum or brainstem with low to intermediate attenuation, with or without contrast enhancement. May extend into ventricles. | Intermediate between low grade astrocytoma and glioblastoma multiforme; ~2-y survival. |
Ependymoma | Circumscribed spheroid or lobulated infratentorial lesion, usually in the fourth ventricle, with or without cysts and/or calcifications; low to intermediate attenuation, variable contrast enhancement; with or without extension through the foramina of Luschka and Magendie. | Occurs more commonly in children than adults; two thirds infratentorial, one third supratentorial. |
Choroid plexus papilloma or carcinoma | Circumscribed and/or lobulated lesions with papillary projections, intermediate attenuation, usually prominent contrast enhancement, with or without calcifications. Locations: atrium of lateral ventricle (children) > fourth ventricle (adults), rarely other locations such as third ventricle; associated with hydrocephalus. | Rare intracranial neoplasms; CT and MRI features of choroid plexus carcinoma and papilloma overlap; both histologic types can disseminate along CSF pathways and invade brain tissue. |
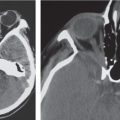
Epidermoid | Well-circumscribed spheroid or multilobulated, extra-axial ectodermal inclusion cystic lesions with low to intermediate attenuation, no contrast enhancement, with or without bone erosion/destruction. Often insinuate along CSF pathways; chronic deformation of adjacent neural tissue (brainstem, brain parenchyma). Commonly located in posterior cranial fossa (cerebellopontine angle cistern, fourth ventricle) > parasellar/middle cranial fossa. | Nonneoplastic congenital or acquired extra-axial off-midline lesions filled with desquamated cells and keratinaceous debris; usually mild mass effect on adjacent brain; infratentorial > supratentorial locations. Adults: men = women; with or without related clinical symptoms. |
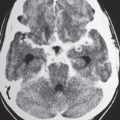
Cysticercosis | Single or multiple cystic lesions in the brain, meninges, or ventricles. Acute/subacute phase: Low to intermediate attenuation, rim with or without nodular pattern of contrast enhancement, with or without peripheral edema. Chronic phase: Calcified granulomas. | Caused by ingestion of ova (Taenia solium) in contaminated food (undercooked pork); involves meninges > brain parenchyma > ventricles. |






Lesions | CT Findings | Comments |
Normal variant | Small ventricles with normal appearance of brain parenchyma and presence of CSF in subarachnoid spaces and cisterns. | Normal variation. |
Postshunt/overshunting | Small, slitlike ventricles (with or without shunt tube present). | Small ventricular size can result from acute or chronic overdrainage of ventricles with shunts. |
Increased intracranial pressure | Small ventricles with effacement of subarachnoid spaces, with or without decreased attenuation in brain parenchyma; cerebral edema. | Ventricular size usually does not correlate well with intracranial pressure. |
Pseudotumor cerebri | Normal shape but small ventricles, with or without mild prominence of intracranial subarachnoid spaces, with or without prominence of fluid in optic nerve sheath complex. | CT with contrast provides a role in excluding intracranial tumors involving the brain or leptomeninges. |
Related posts:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree