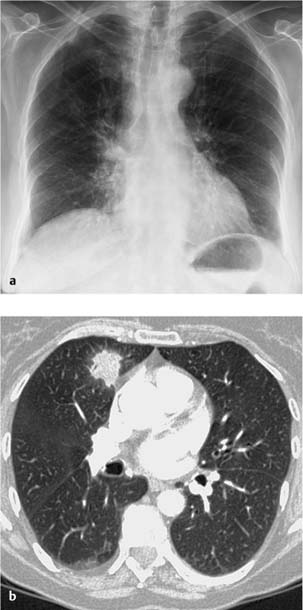
5 Idiopathic Interstitial Pneumonia Idiopathic pulmonary fibrosis is classified by the American Thoracic Society (ATS) and European Respiratory Society (ERS) as an idiopathic interstitial pneumonia (chronic form of idiopathic interstitial pneumonia). Most common form of idiopathic interstitial pneumonia, accounting for about 50% of cases Inflammatory fibrotic disorder of the pulmonary parenchyma of uncertain etiology CT. Reticular shadowing, primarily in the basal segments. Reticular shadowing CT findings in the context of corresponding clinical data are diagnostic (sensitivity is about 50%, specificity > 90%, positive predictive value > 90%); biopsy is not required. Initially insidious but progressive respiratory distress over > 6 months Responds to steroids only in combination with ciclosporin Prognosis is not favorable Confirmation of the diagnosis Fig. 5.1 Idiopathic pulmonary fibrosis. a The plain chest radiograph shows extensive, primarily reticular and honeycomb interstitial changes. b CT shows primarily basal and peripheral subpleural interstitial honeycombing. The trabeculation of the pleural boundaries (arrow), bronchiectasis resembling a string of pearls (open arrow), bronchiectasis resembling a string of pearls (open arrow), ectasia of the trachea and main bronchi (*) are further signs.
Idiopathic Pulmonary Fibrosis
Definition
 Epidemiology
Epidemiology
 Occurs at age 40–50 years
Occurs at age 40–50 years  More common in men than in women.
More common in men than in women.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
 Areas of fibrotic changes in various stages alternating with normal parenchyma
Areas of fibrotic changes in various stages alternating with normal parenchyma  Nodular fibrosis and honeycomb cystic destruction.
Nodular fibrosis and honeycomb cystic destruction.
Imaging Signs
 Modality of choice
Modality of choice
 Radiographic findings
Radiographic findings
 CT findings
CT findings
 Honeycombing
Honeycombing  Traction bronchiectasis
Traction bronchiectasis  Focal ground-glass opacities
Focal ground-glass opacities  Disorganization of pulmonary architecture
Disorganization of pulmonary architecture  Predilection for the peripheral, basal, and subpleural regions
Predilection for the peripheral, basal, and subpleural regions  Apicobasal gradient.
Apicobasal gradient.
 Pathognomonic findings
Pathognomonic findings
Clinical Aspects
 Typical presentation
Typical presentation
 Nonproductive cough
Nonproductive cough  Clubbed fingers (occurs in up to 50% of cases).
Clubbed fingers (occurs in up to 50% of cases).
 Therapeutic options
Therapeutic options
 Lung transplant.
Lung transplant.
 Course and prognosis
Course and prognosis
 Median survival time after diagnosis is 2.5–3.5 years.
Median survival time after diagnosis is 2.5–3.5 years.
 What does the clinician want to know?
What does the clinician want to know?
 Course
Course  Complications (other opportunistic infections, Pneumocystis jirovecii pneumonia).
Complications (other opportunistic infections, Pneumocystis jirovecii pneumonia).
Differential Diagnosis
Other forms of idiopathic interstitial pneumonia | – Micronodules are inconsistent with idiopathic pulmonary fibrosis – Extensive ground-glass opacities – Consolidations – Peribronchovascular distribution |
Secondary interstitial pneumonia | – Pulmonary involvement in collagen diseases, vasculitis, drug reactions, or inhaled noxious agents |
Cryptogenic organizing pneumonia | – Cryptogenic organizing pneumonia with a reticular pattern can be difficult to distinguish from diffuse pulmonary fibrosis |
Extrinsic allergic alveolitis (hypersensitivity pneumonitis) | – Exposure to allergens – Mosaic pattern |
Tips and Pitfalls
Radiographic findings are often suggestive and permit a diagnosis in about 70% of cases.
Selected References
American Thoracic Society/European Respiratory Society. International multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 2002; 165: 277–304
Kim DS, Collard HR, King TE. Classification and natural history of the idiopathic interstitial pneumonias. Proc Am Thor Soc 2006; 3: 285–292
Müller-Lang C et al. [Idiopathische interstitielle Pneumonien.] Radiologe 2007; 47: 384–392 [In German]
Wittram C, Mark EJ, McLoud TC. CT–histologic correlation of the ATS/ERS 2002 classification of idiopathic interstitial pneumonias. Radiographics 2003; 23: 1057–1071
Cryptogenic Organizing Pneumonia
Definition
Cryptogenic organizing pneumonia is classified by the ATS and ERS as an idiopathic interstitial pneumonia (subacute form of idiopathic interstitial pneumonia)  Formerly referred to as bronchiolitis obliterans.
Formerly referred to as bronchiolitis obliterans.
 Epidemiology
Epidemiology
Idiopathic cryptogenic organizing pneumonia is a rare form of idiopathic interstitial pneumonia, accounting for about 10% of cases  Occurs at age 40–50 years
Occurs at age 40–50 years  No sex predilection
No sex predilection  More common in smokers than in nonsmokers.
More common in smokers than in nonsmokers.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Rare in its idiopathic form; more common secondary to collagen diseases and infectious or drug-induced pulmonary disorders  Polypoid granulomatous inflammation of the respiratory bronchioles and alveoli without disorganization of the pulmonary architecture.
Polypoid granulomatous inflammation of the respiratory bronchioles and alveoli without disorganization of the pulmonary architecture.
Imaging Signs
 Modality of choice
Modality of choice
CT.
 Radiographic findings
Radiographic findings
Unilateral or bilateral nodular opacities  Resembles pneumonia.
Resembles pneumonia.
 CT
CT
Bilateral focal non-segmental consolidations in the subpleural or peribronchial regions (> 80% of cases)  Tendency to migrate
Tendency to migrate  An air bronchogram is common
An air bronchogram is common  Perifocal ground-glass opacity (in 60% of cases)
Perifocal ground-glass opacity (in 60% of cases)  Peribronchiolar centrilobular round focal lesions < 10 mm with irregular borders in up to 50% of cases.
Peribronchiolar centrilobular round focal lesions < 10 mm with irregular borders in up to 50% of cases.
 Pathognomonic findings
Pathognomonic findings
Focal areas of consolidation with air bronchogram and associated ground-glass opacification in the subpleural or peribronchial region  Findings are unchanged or progressive for weeks despite antibiotics.
Findings are unchanged or progressive for weeks despite antibiotics.
Clinical Aspects
 Typical presentation
Typical presentation
Subacute onset over a period of up to 3 months  Nonproductive cough
Nonproductive cough  Subfebrile temperatures
Subfebrile temperatures  Often a lower airway infection is initially suspected
Often a lower airway infection is initially suspected  Restrictive pulmonary dysfunction.
Restrictive pulmonary dysfunction.
 Confirmation of the diagnosis
Confirmation of the diagnosis
Biopsy.
 Therapeutic options
Therapeutic options
Inhalational or systemic steroids.
 Course and prognosis
Course and prognosis
Prognosis is good with steroid therapy.
 What does the clinician want to know?
What does the clinician want to know?
Diagnosis  Course under therapy.
Course under therapy.
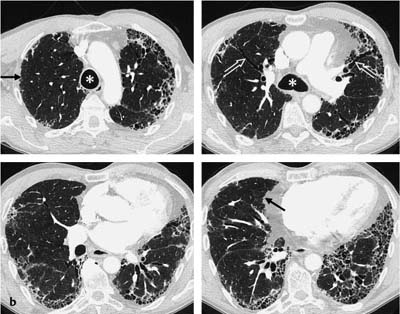
Fig. 5.2 Cryptogenic organizing pneumonia in a 67-year-old woman.
a The plain chest radiograph shows isolated moderately sharply demarcated focal densities bilaterally but primarily on the right side. The right hilar bronchovascular bundles appear slightly thickened.
b CT shows the focal lesions as homogeneous areas of consolidation with isolated excursions but otherwise without any reaction in the adjacent tissue.
Differential Diagnosis
Bronchioalveolar carcinoma | – History – Lung biopsy |
Pneumonia or bronchopneumonia | – Usually unilateral and unilocular – Responds to antibiotics |
Eosinophilic pneumonia | – Predilection for the upper lobes – Blood eosinophilia |
Sarcoidosis | – Predilection for the bronchovascular bundle – Lymphadenopathy |
Lymphoma | – Known underlying disease – Extrathoracic involvement |
Reaction as in bronchiolitis obliterans | – Occurs in collagen diseases – Drug reaction – Toxic damage from inhaled agent – Sequela of aspiration – Postinfectious |
Tips and Pitfalls
Can be misinterpreted as pneumonia.
Selected References
American Thoracic Society/European Respiratory Society. International multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 2002; 165: 277–304
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree