Optimal assessment of the mediastinal masses is performed by a combination of clinical, radiological and often histological assessments. Image-guided transthoracic biopsy of mediastinal lesions is a minimally invasive and reliable procedure to obtain tissue samples, establish a diagnosis and provide a treatment plan. Biopsy can be performed under Computed Tomography, MRI, or ultrasound guidance, using a fine needle aspiration or a core-needle. In this paper, we review the image-guided strategies and techniques for histologic sampling of mediastinal lesions, along with the related clinical scenarios and possible procedural complications. In addition, image-guided mediastinal drainage and mediastinal ablations will be briefly discussed.
Key points
- •
For mediastinal biopsies, image guidance is necessary for targeting the lesion and developing an overall plan. Although computed tomography is the most common imaging modality used for this purpose, ultrasound may be used in some scenarios.
- •
Mediastinal biopsy using a coaxial needle and gun has gained acceptance over fine-needle aspiration due to increased accuracy, particularly for lymphoma.
- •
To avoid complications and ensure patient safety, biopsy needles should not be targeted toward pulsating organs or vascular structures.
- •
Mediastinal ablation procedures for limited metastasis and recurrent tumor after initial surgical resection or radiation therapy are being performed more frequently.
- •
Cryoablation for mediastinal neoplasms is well tolerated by patients, although the heat sink can lead to incomplete ablation and local recurrence.
Introduction
Management of mediastinal masses requires accurate diagnosis to develop appropriate treatment strategies. Image-guided transthoracic biopsy of mediastinal lesions is a minimally invasive and relatively safe procedure that can be used to obtain histologic samples under local anesthesia and conscious sedation, tailor the treatment plans, and potentially obviate more invasive diagnostic procedures. Not all mediastinal masses require biopsy, as certain lesions demonstrate characteristic imaging features that enable diagnosis. Examples of such entities that can be solely diagnosed on clinical and imaging characteristics are retrosternal goiter and asymptomatic visceral compartment cystic lesions such as bronchogenic cyst or esophageal duplication cyst. In addition, in certain clinical conditions, transthoracic needle biopsy of a mediastinal lesion is contraindicated, including uncontrollable cough, bleeding diathesis (international normalized ratio [INR]>1.4; platelet count <50000/mL; increased prothrombin time with INR>1.5 or partial thromboplastin time >1.5 times greater than the normal range), bullous emphysema, and moderate-to-severe pulmonary hypertension. In addition, when there is a characteristic hydatid cyst or a vascular lesion on computed tomography (CT), biopsy should be avoided.
Image-guided transthoracic needle biopsy is regarded as the reliable, cost-effective, and standard method of choice for obtaining specimens from mediastinal lesions. Biopsy planning can be performed via CT, magnetic resonance (MR) imaging or ultrasound. Each of these methods has its inherent advantages and disadvantages. Percutaneous image-guided sampling is performed by fine-needle aspiration or core needle biopsy. The choice of technique depends on the lesion characteristics, location, patient comorbidities, and the experience of the operating physician.
This article reviews the various image-guided strategies for biopsy of mediastinal lesions with focus on the diagnostic yield, clinical relevance, technical aspects of biopsy performance, and possible complications. The role of mediastinal ablation for treating conditions such as limited mediastinal metastasis and recurrent thymoma and malignant pleural mesothelioma will also be described. Finally, the use of image guidance for draining mediastinal collections and benign cystic lesions is briefly discussed.
Imaging modalities and clinical relevance
Image-guided mediastinal biopsy can be performed using different modalities including CT, MR imaging, and ultrasound, with CT remaining, which is used most frequently. The diagnostic yield is defined as the proportion of the diagnostic results achieved by image-guided biopsy, whereas diagnostic accuracy is the proportion of the correct diagnoses relative to the final diagnosis of the lesion. Overall, lymphoma and thymoma are the most common mediastinal mass lesions diagnosed with image-guided biopsy.
Tissue diagnosis is an essential step for management of prevascular mediastinal lesions, except in those with typical imaging features of a cyst. Image-guided biopsy is the least invasive initial method to obtain tissue, as it can obviate more invasive procedures such as mediastinoscopy and anterior mediastinotomy. The sensitivity of needle biopsy in diagnosing prevascular mediastinal lesions depends on tumor type. Most of the nondiagnostic mediastinal biopsies are later diagnosed as lymphoma. The diagnostic yield of percutaneous biopsy for mediastinal lymphoma varies and is based on the pathologic subtype of lymphoma. Fine-needle aspiration has low diagnostic yield for lymphoma, whereas core needle biopsy increases the diagnostic accuracy, in particular, for Hodgkin lymphoma.
Computed Tomography
CT is the most commonly used modality for localization of mediastinal lesions and documentation of biopsy needle track. A meta-analysis of 1345 CT-guided core needle biopsies of mediastinal masses from 18 studies found pooled diagnostic yield of 92% with 94% diagnostic accuracy. They showed that diagnostic yield and accuracy were significantly higher in studies with 3 or higher sampled cores. CT scan allows for accurate targeting and assesses for complications during and immediately after biopsy, for example, pneumothorax or pleural effusion, which can be missed with ultrasound.
MR Imaging
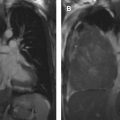
MR imaging may have some advantages over CT, including its superior soft tissue resolution, real-time multiplanar imaging capabilities, excellent delineation of the vascular structures, and lack of ionizing radiation. It is also the preferred modality to assess the paravertebral lesions with possible neural origin. MR imaging, however, is limited by higher costs, longer procedure time, motion artifact, and paramagnetic artifact from usual biopsy needles, which can limit visualization of small lesions or the needle trajectory path in some patients. Garnon and colleagues were the first to describe the use of MR-targeted biopsy of mediastinal lesions in 16 individuals using wide-bore high-filed scanner. They reported a technical success and accuracy of 100% and 87.5%, respectively, with a mean procedure duration of 42 minutes, without any immediate complications.
Ultrasound
Certain mediastinal lesions may be accessible through ultrasound guidance. The technique is practical when the mediastinal lesions are adequately imaged by ultrasound, including those located in the high prevascular mediastinum or those that are adjacent to or protrude through the chest wall. Ultrasound is cost-effective, time saving, and feasible for sampling of mediastinal lesions with diagnostic yield of 80% to 100%. Advantages of ultrasound are continuous real-time needle and target visualization, the ability for oblique needle placement, needle slope manipulation or changing the patient’s position during procedure, and the possibility to perform the targeted biopsy at the bedside of critically ill patients. These features are difficult or impossible to perform under CT guidance. The additional use of color Doppler ultrasound can help avoid the vascular structures during procedure. The main limitation of ultrasound is the limited acoustic window. In the largest series of ultrasound-guided biopsies of mediastinal lesions, Petkov and colleagues evaluated the efficacy of using ultrasound guidance for sampling mediastinal masses larger than 15 mm in 566 patients. The target lesion was visible on ultrasound in 54.4% (91.9% in prevascular, 0.6% in visceral, and 7.5% in paravertebral mediastinum) of the study cohort, in whom ultrasound-guided core needle biopsy was performed. In the individuals with nonvisible lesions on ultrasound, CT-guided transthoracic core needle biopsy was performed. The diagnostic yield of ultrasound-guided biopsy was 96%, comparable with 90% diagnostic accuracy in CT-guided biopsy.
The application of contrast-enhanced ultrasound can increase the diagnostic yield and diagnostic accuracy of biopsy compared with conventional ultrasound guidance. Contrast-enhanced ultrasound allows detection of necrotic and nonviable areas within the mass to be precluded from sampling. ,
Technical considerations
Needle Selection
Several types of needles with different caliber can be used for sampling mediastinal lesions. Needle selection depends on the presumptive diagnosis, size of the lesion, lesion depth from skin, proximity of the vital structures to the biopsy path, and the operating radiologist experience. Cutting-bore or Tru-Cut guns, ranging from 14 to 20 gauge in caliber, can be used to obtain specimen for histologic evaluation and are usually introduced through a coaxial needle. The most common size combination is the 19-gauge coaxial needle and 20-gauge gun. Aspiration needles, ranging from 20 to 23 gauge in caliber are used for cytologic evaluation. Adequate tissue target sampling and diagnostic accuracy are more achievable using core needle biopsy than fine-needle aspiration. Fine-needle aspiration has high sensitivity for obtaining tissue specimens from cystic masses or malignant metastatic lesions; however, it has a relatively low diagnostic yield for the diagnosis of lymphoma. A combination of fine-needle and multiple (ie, 3–5) core needle biopsies has higher diagnostic performance for this purpose. Overall, fine-needle aspiration was the preferred strategy in lesions that are adjacent to vital structures (such as the great vessels), in transpulmonary approach for biopsy, and specifically when a metastatic disease is the first clinical impression. Currently, the most common biopsy technique uses the coaxial system, which is preferred by most radiologists. The guide coaxial needle is placed in a position near or in the target lesion and then a biopsy gun is advanced through the coaxial system to obtain the specimen. Coaxial systems help reduce the number of passes and the possibility of iatrogenic injury to the vital structures. Larger caliber guns can provide much better tissue samples for genetic analysis and hence improve genomic sequencing in particular for lymphoma. In circumstances where tissue is accessible and size of tumor is larger than 1.5 cm, 17-/18-gauge coaxial/gun systems are preferred.
Biopsy Procedure
Image-guided mediastinal biopsy is routinely performed under conscious sedation by using midazolam and/or fentanyl citrate. In noncooperative patients and in pediatric patients, deep sedation or general anesthesia is usually necessary. Local anesthetics (eg, 5–10 mL 1% solution of Lidocaine) are administered before the procedure. Patients may be placed in the supine, prone, or lateral decubitus position based on the selected biopsy approach and the anatomic location of the target lesion. Simple positioning of the patient in the oblique decubitus can allow for mediastinal shift and the mass to move into an accessible needle trajectory approach in order to avoid traversing lung. Before beginning the procedure, the lesion is reassessed on previously acquired cross-sectional images or ultrasound. When prior fluorodeoxyglucose (FDG) PET/CT is available, the most FDG-avid portions of the mediastinal mass lesion are targeted. Repeat imaging examination may be necessary based on the individual case. When planning the path for the needle, it is important to choose a course that allows for the needle to be tangential to the mediastinal vessels in order to avoid targeting the needle toward pulsating organs or vascular structures.
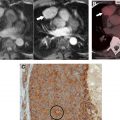
For CT-guided biopsy, unenhanced CT with 3 mm slices is generally adequate to plan the procedure. In select high-risk cases, however, the use of intravenous contrast material could help delineate vascular structures, especially those that may be engulfed by tumor, in the needle trajectory. The optimal CT section is then marked on the skin with the axial laser localizer of the scanner. Radiopaque markers are positioned along the laser light beam, and the scan is repeated to localize the exact point of entry ( Fig. 1 A). A radiopaque marker is then replaced with a skin mark using an indelible pen. A repeat localizer CT is required in each step of needle advancement to ensure the safety of needle trajectory and readjust the biopsy needle when necessary ( Fig. 1 B). When the mediastinal fat contact with the biopsy needle is not satisfactory to ensure a safe needle trajectory, injection of physiologic saline or dilute contrast medium into the mediastinum can create a safe extrapleural path for performing the biopsy ( Fig. 1 ).

For ultrasound-guided mediastinal biopsy procedures, a sector (2.0–2.5 MHz), convex (3.5–5–7.5 MHz), or linear (5–7.5–12.0 MHz) array transducer may be used by the operating radiologist based on the depth of the target lesion from skin and the available acoustic window. The gray scale B-mode imaging is used to direct the needle toward the target lesion, frequently accompanied by color doppler imaging to avoid the mediastinal vessels. In addition, a twinkling sign on color doppler ultrasound allows visualization of the biopsy needle. Needles may be introduced using a free-hand technique or a stretcher guide attached to the transducer. The free-hand technique allows manual movement of the needle into the target lesion under direct visualization.
When the radiologist will be acquiring specimens, it is important to be familiar with the biopsy system, particularly the loading of the gun and the extent of the “throw” beyond the coaxial needle. Injury by extension of the gun into vital structures is unacceptable. The number of samples obtained depends on the suspected disease and the radiologist’s confidence. Typically, 2 to 5 cores are obtained per target lesion.
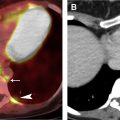
Iatrogenic pneumothorax can be used for mediastinal access without traversing a diseased lung. This approach adds extra time to the procedure but provides a much quicker recovery ( Fig. 2 ).

Following the biopsy, patients may be observed on the scanner for 5 to 10 minutes to confirm the absence of bleeding before moving the patient to an observation unit. Patients are generally observed for at least 2 hours after the procedure to ensure hemodynamic stability and to monitor respiratory status. Imaging with chest radiographs or CT fluoroscopy is performed immediately after the procedure and 2 hours after the biopsy in patients in whom the pleura was punctured or when there has been respiratory distress.
Interventional Approaches
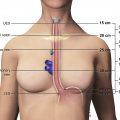
Mediastinal lesions can be accessed through parasternal, transsternal, suprasternal, paravertebral, subxiphoid, transpleural, and transpulmonary approaches. A transthyroid approach can also be attempted to access a retrotracheal target lesion. Transgression of the brachiocephalic vein using a small-caliber fine-needle aspiration needle is a safe and applicable method to obtain samples from target lesions through suprasternal, substernal, and parasternal approaches.
Parasternal
The parasternal route is the most common approach for sampling prevascular and visceral mediastinal lesions, specifically those that are located in the prevascular, pretracheal, paratracheal, and aorticopulmonary window stations. The technique is feasible under CT or ultrasound guidance. The biopsy needle is inserted lateral to the sternum, and the lesion is reached through the parasternal muscles and mediastinal fat. It is important to identify the internal thoracic arteries and veins to prevent vascular injury during the procedure. The internal thoracic vessels can be identified within 2.5 cm of the either side of the sternum. The needle is placed either medial or lateral to the internal thoracic vessels that can be displaced by injecting saline with or without lidocaine (see Fig. 1 B). In an ultrasound-guided parasternal approach, a small footprint probe is required considering the limited acoustic window resulting from anterior curvature of the ribs and costal cartilages ( Fig. 3 ).