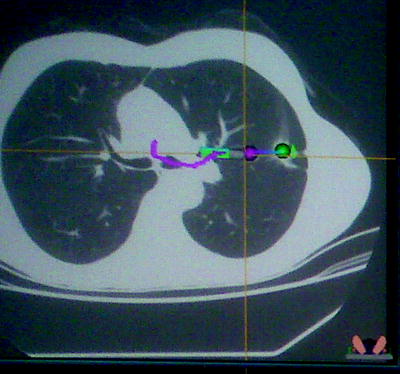
Fig. 24.1
Virtual bronchoscopy showing and endobronchial lesion (arrow)
Virtual Bronchoscopy Navigation and Systems
Virtual bronchoscopy navigation is a VB method clinically applicable to arrive at the peripheral lesions. Virtual images of the bronchial path to the lesion are produced and used for navigation and guidance during real-time bronchoscopy. Unlike the virtual bronchoscope, the tip of the real bronchoscope can only be moved up or down so that appropriate rotation is always necessary for adequate navigation and airway visualization. But when the bronchoscope is rotated, the real image shifts from the virtual image. Therefore, synchronization of the virtual and real images is necessary especially at each branching; otherwise, the risk of disorientation becomes significant. To overcome these issues, systems for clinical use have been developed recently, and data collection is in progress.
Systems in this category include, but are not limited to, the VBN system (Bf-NAVI; KGT, Olympus Medical Systems, Tokyo, Japan) and the LungPoint System by Broncus Technologies. The former system is characterized by the automatic production of VB images along the bronchial path and the display of VB synchronized with real images for bronchoscopic navigation. Bronchoscopists initially input the digital imaging and communication in medicine (DICOM) data of CT images into the system. A CT slice thickness of less than or equal to 1 mm is desirable. Then, the starting point in the trachea is chosen. An appropriate threshold is automatically adjusted, and bronchi to peripheral areas are extracted. Finally, the target is set as well as the terminal point. While observing short-axis, sagittal, and coronal images, the operator selects the lesion and the bronchus closest to it as the target and terminal point, respectively (Fig. 24.2).
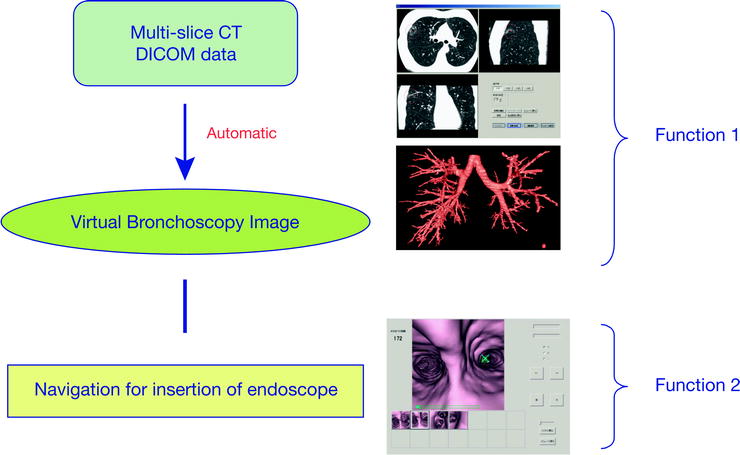
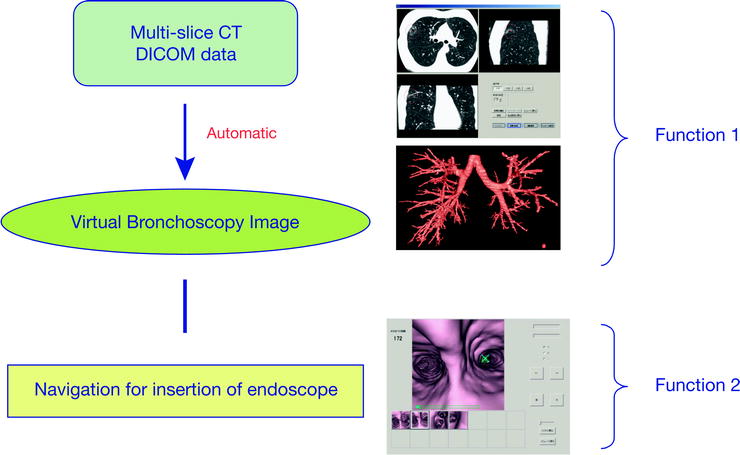
Fig. 24.2
Steps in the setting of the BF-NAVI system
Because the extracted bronchi are indicated in blue, the bronchi involved with the lesion are clearly observed all the way up to the proximal area on the monitor confirming that each branching is extracted. Importantly, alternative manual path extraction can be added. When the target and terminal point are determined, the path to the terminal point is automatically searched and displayed. When the point in the path is moved from the starting to the terminal point, each corresponding cross-sectional image is displayed and the branching and extraction status in the path are reconfirmed. The path is also displayed in the bronchial tree. When the path is determined, VB images along the path are automatically produced. While VB images are moved from the starting to terminal point, the bronchus for the insertion of the bronchoscope at each bronchial branching is marked and registered as a thumbnail (Fig. 24.3).
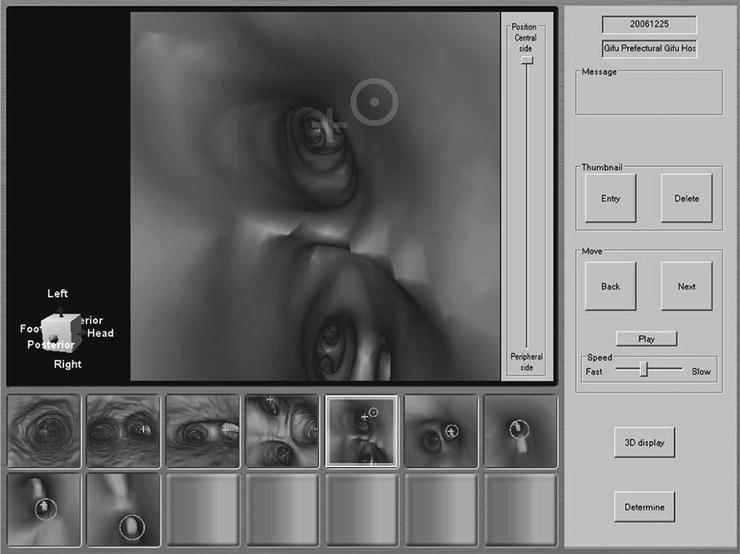
Fig. 24.3
Display of the VB-NAVI system
The time required from the insertion of DICOM data of CT into the system to the completion of thumbnail registration is approximately 15 min, of which half used for manual setting and confirmation. The median range of the production of VB images using this system is the sixth-generation bronchi. VBN is performed while displayed VB images of the target bronchus are synchronized with real-time endoscopic images by image rotation, advancement, and retreat. Concretely, the VB image that diverges from the real image because of the rotation at the time of bronchoscope insertion is made consistent with the real image using the rotation function. Subsequently, the VB image is advanced to the next bronchial branching, and the bronchoscope is similarly advanced. This procedure is repeated. Because the bronchus to which the bronchoscope is advanced is displayed on the VB image at each branching, the bronchoscope is advanced to the target based on this display. When branching is lost during bronchoscopic advancement, VB images are redisplayed, and a thumbnail at each branching is provided as a reference. The direction of the lesion is displayed on the image and can also be referred to.
Most of the data about the safety, efficacy, and yield of this system comes from the Far East. Together, there are eight studies with a total of 428 lesions (317 lesions less than 2 cm); the diagnostic yield was 73% (67% for lesions less than 2 cm).
The LungPoint Virtual Bronchoscopic Navigation System (Broncus Technologies, Inc., Mountain View, CA) is computer-assisted image-based navigation software that enables the bronchoscopist to navigate and localize a targeted area of interest in the lung. The system requires thin-section CT scans in the order of 1.25-mm slice thickness with an interval spacing of 0.0625 mm or less. Scans at total lung capacity (inspiratory breath-hold) are preferred so that the smaller airways are expanded. The system has the capacity to import scans in standard Digital Imaging and Communications in Medicine format either from a compact disk or across the network. Once imported, the images are automatically analyzed by the LungPoint software. This involves segmenting airways 3 mm and greater in diameter and major vessels by calculating a centerline (central axis) for each airway. Along with airway segmentation, endoluminal renderings of the airway structure are modeled to produce a virtual bronchoscopic view. Once the target object is placed, the software calculates up to three pathways through the airways to reach it. These pathways are calculated to reach the points closest to the target. Three-dimensional images of the airway tree and target as well as the virtual bronchoscopic animation enable assessment of the calculated pathways. The CT projections are also available and update as the animation progresses through the airway toward the target. The navigation system displays two main images: the live bronchoscopic video and the VB animation (Fig. 24.4).
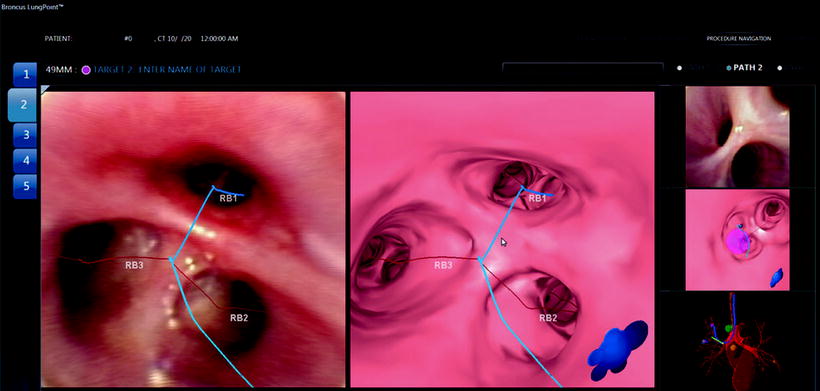
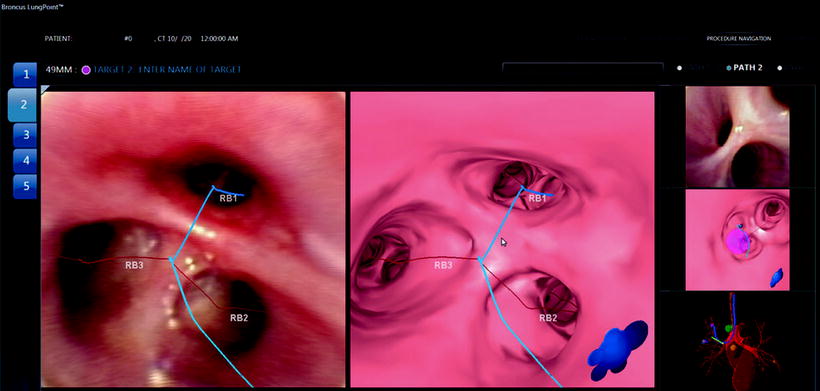
Fig. 24.4
Pathway projected on the virtual (right) and real image (left) on the LungPoint system
The animation represents the pathway that was selected during the planning process. An image-based synchronization technique aligns the virtual images with the anatomy seen in the live bronchoscopic video. An assistant can facilitate this process by advancing and adjusting the virtual bronchoscopic rendering. When the two images are synchronized, the software calculates the position of the bronchoscope in the airway and overlays the pathway to the target on the actual bronchoscopic video image. Adjacent major vessels as well as the target are overlaid on the airway wall. Data on the safety and diagnostic yield of this system is being collected. One series from Germany included 25 subjects (9 women and 16 men, mean age 67 years) with 25 lesions (mean size 28 mm). Using this navigation system, the bronchoscope could be advanced along the planned route in all cases. In 14 of the cases (56%), the bronchoscope could be advanced all the way to the lesion bronchus. The planning time was a median of 5 min, and the median examination time was 15 min. A definitive diagnosis was possible in 20 cases (80%). One patient experienced a small pneumothorax because of the biopsy that resolved without drainage. No other complications occurred.
It is important to remember that VBN-supported bronchoscopy is not providing real-time guidance, as the instrument is not registering as it moves along. Additionally, instrumentation cannot be guided with this approach.
Electromagnetic Navigation
EMN-guided bronchoscopy solves some of the problems of VBN-based guidance. The instrument position is registered in real time within an electromagnetic field, and instruments can equally be tracked. EMN-based navigation has been in clinical use in neurosurgery and vascular medicine, and several such systems are commercially available now for respiratory applications. Examples include the Superdimension and the Veran guidance systems.
When using the Superdimension process, the heart of the electromagnetic system is the locator guide and the magnetic locator board (Fig. 24.5). Performing the navigation procedure is a three-step process. The initial stage (the planning phase) is done prior to the procedure. The patient must have a high-quality CT scan of the chest (there is no need for contrast material) with cuts of 1.5 mm or less and a 1.0-mm overlap. The later criteria provide adequate resolution for the system to create a 3D map of the airways. It also provides cuts of the lung in coronal, sagittal, and longitudinal planes. The physician then marks the affected area to which navigation is desired (Fig. 24.6).


Fig. 24.5
Steerable guide (left) and magnetic locator board (right)