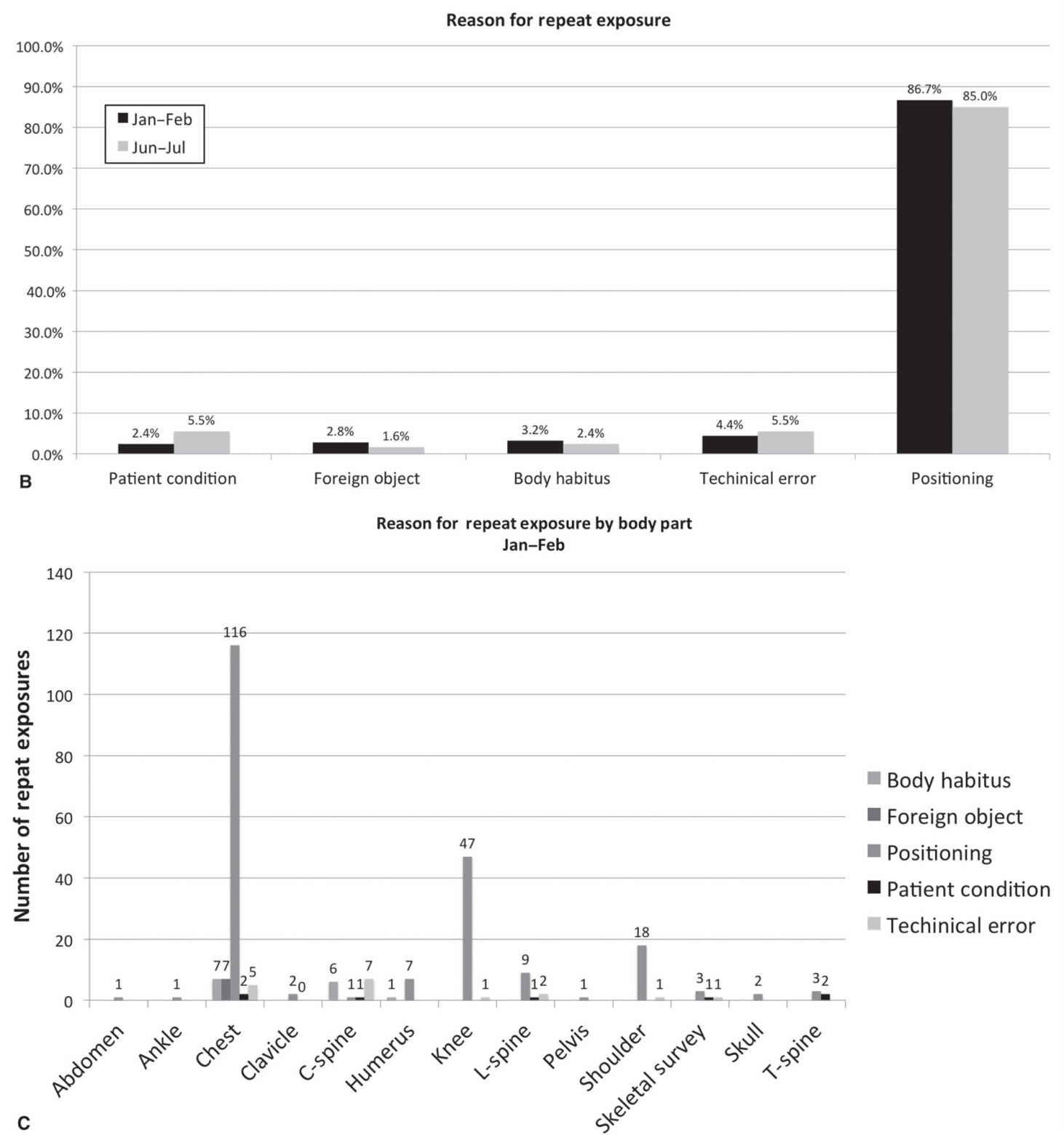
FIG. 5.1 ● Sample data from a quality improvement project assessing digital radiography (DR) repeat rates in a single X-ray room. Education on patient positioning for knee radiographs was provided to technologists between the two time periods. A: Graph showing DR repeat rates over the two examined time periods. Note the marked drop in repeat rates from 21% to 7.3% after the action plan was initiated. B: Graph detailing reason for DR repeat rates over two examined periods. Note that patient positioning is the dominant cause for DR repeat in both time periods. C: Graph from initial time period showing repeat rates by examination, highlighting that positioning for chest and knee radiographs are the major contributors to DR repeats.
The American Association of Physicists in Medicine (AAPM) first published QA guidelines for radiography in 1977,9 followed by updated guidelines in 2002.10 The guidelines advocate for instituting a QC program designed to ensure that radiography studies were obtained with acceptable image quality. The QC program should focus on equipment, processing, and technologist performance. Specifically, the AAPM states in the 2002 report that the repeat rate analysis should be performed at least quarterly, preferably by the same individual to ensure consistency in analysis. To understand repeat rate data, the AAPM suggests that the report contain the following data points: patient positioning, patient motion, artifacts, film fog (for film screen), equipment malfunctions, over- or underexposed films, examination room, technologist, and the anatomical view.
Image quality management extends beyond radiography into other imaging modalities such as computed tomography (CT), ultrasound (US), magnetic resonance imaging (MRI), fluoroscopy, mammography, and nuclear medicine. Radiologists may be more directly involved in image QA and QC for these modalities because of the lower volumes as compared with radiography, close proximity to technologists such as with US and mammography (especially diagnostic mammography), and extensive involvement in protocol development such as in CT and MRI.
Computed Tomography
Image quality management in CT not only ensures that image quality is adequate but also can help protect patients from unnecessarily high exposures to ionizing radiation. CT operators typically work with medical physicists and vendors to ensure that equipment is functioning properly and scheduled maintenance is performed. Specific features of image quality that require assessment, typically by a trained medical physicist, include CT number, image noise, contrast-to-noise ratio, and spatial resolution.11
The radiologist also plays an important role in CT image quality management. CT protocols are typically developed or modified by radiologists to reflect practice preferences and specific clinical indications. A radiologist or group of radiologists should review CT protocols regularly to confirm that the protocols are still appropriate for the designated clinical indication(s) and that they meet the needs of interpreting radiologists while minimizing patient exposure to ionizing radiation. Additionally, radiologists should regularly monitor scans for higher-than-expected radiation exposure, artifacts, appropriate patient positioning and scan range, and adherence to prescribed protocols.
Ultrasound
Quality management in the United States can be challenging because the US units are becoming increasingly common in hospitals, medical centers, and private offices, and not all US equipment falls under the purview of radiology. The first step in developing an US quality management program is to inventory all ultrasound equipment, including transducers and handheld units. Second, equipment needs to be evaluated by a medical physicist for performance. Specific tests include system sensitivity, uniformity, spatial accuracy, and contrast and spatial resolution. Additionally, the medical physicist should work closely with users of the equipment to ensure that settings are optimized for image quality. Aside from image quality management, US equipment should be evaluated by an appropriate individual such as a clinical engineer for mechanical and electrical safety.12
Magnetic Resonance Imaging
Because of the complexities of MRI, image QC requires substantial technical expertise. The American Association of Physicists in Medicine has published AAPM Report No. 28 “Quality Assurance Methods and Phantoms for Magnetic Resonance Imaging” to “describe a standard set of test procedures, which can be used to evaluate the performance of clinical magnetic resonance imaging systems.”13 Not only must MR units themselves be evaluated, but coils used in clinical scans must also be evaluated. As with CT, a specialized medical physicist is typically delegated the responsibility for managing MRI image quality management.
Radiologist involvement in MRI image quality management focuses on developing acquisition protocols and regularly evaluating the performance of these protocols as well as providing ongoing feedback to MRI technologists regarding the quality of clinical MRI examinations. Consultation with a medical physicist may be warranted when artifacts persist across multiple patients or when images continue to be suboptimal.
MEDICAL IMAGING CHAIN
While image quality may be thought of as the result of the single action of image acquisition, it is actually part of a sequence of events (Table 5.1) that begins with exam ordering and ends with communication of results.14 Each step involves multiple technologies and individuals beyond the imaging modality and the technologist. Other technologies include computerized physician order entry (CPOE), radiology information systems, postprocessing software, PACS, and radiology reporting systems.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree