Multimodality images for planning
CT imaging plays a crucial role in radiotherapy planning as it provides the electron density information that is required to correct the absorbed dose for the different tissues through which the beams will pass.
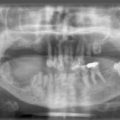
CT imaging also provides excellent definition between tissues having marked differences in x-ray attenuation values (e.g. air/bone/soft tissue), however, the contrast of these images is poor for structures with similar electron densities (e.g. tumour/soft tissue).
Magnetic resonance imaging (MRI) is based on the measurement of radiofrequency radiation resulting from transitions induced between nuclear spin states of hydrogen atoms (protons) in the presence of strong external magnetic fields. Unlike CT, where the signal intensity is dependent on x-ray attenuation and its contrast on the electron density of tissues, MRI depends on the intrinsic tissue properties associated with proton densities and spin relaxation times. Therefore, MRI has the ability to differentiate between tissue of similar density thus providing better delineation, not only of tumour extent, but also of the adjacent critical soft tissue organs.
MRI also provides unrestricted multiplanar, volumetric, vascular and functional information.
Some of the problems associated with using MRI for treatment planning are:
1. inherent image distortion, particularly at the periphery of the image (typically 3 mm for heads and up to 15 mm for pelvic images)
2. pixel intensities are not related to electron density values and therefore cannot be used for heterogeneity correction (i.e. density/dose) when calculating treatment plan dose distributions
3. the physical restrictions of the MRI scanner mean that a patient cannot be easily positioned in the treatment position. A quantitative method called image registration is used that provides fusion of CT and MRI image studies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree