Abdominal trauma presents challenges in diagnostic imaging. Patients with abdominal trauma may have multiple, concomitant life-threatening injuries to the head, spine, chest, and extremities. For the unstable patient, the greatest challenge may be prioritizing injuries for diagnostic and therapeutic interventions. Often, emergency department imaging of these patients must be kept to a minimum before operative intervention. For the stable patient, the challenge is often to avoid unnecessary imaging, which may lead to undesirable radiation exposure and costs of care.
In this chapter, we discuss imaging modalities useful in blunt and penetrating abdominal trauma and imaging of the unstable and the stable patient. For computed tomography (CT) in trauma, we discuss the evidence and indications for contrast agents. We review the interpretation of ultrasound, plain radiographs, and CT images, with a focus on common and serious injury patterns. We also discuss clinical decision rules for blunt abdominal trauma, which may identify patients at low risk for injury who may safely forgo imaging. We consider the safety of discharge from the emergency department following a negative imaging evaluation in blunt and penetrating trauma. Finally, we review trauma imaging in the pregnant patient and radiation exposure in trauma imaging.
Imaging Modalities in Trauma
Plain Radiographs
Plain x-ray plays a limited role in the evaluation of blunt abdominal trauma. X-rays of the chest and pelvis are often obtained to evaluate for concurrent thoracic or pelvic injuries (discussed in dedicated chapters), but normal x-rays do not rule out injuries to solid or hollow abdominal organs. Abnormal chest x-ray findings of pneumothorax and rib fractures are associated with intraabdominal injuries and are indications for abdominal imaging if a mechanism for multisystem trauma is present. Chest x-ray may reveal free air, suggesting hollow organ injury, although this finding is both rare and nonspecific in blunt trauma. Pneumoperitoneum can also result from thoracic injuries, with air tracking into the abdomen, and is thus not an absolute indication for laparotomy. Diaphragmatic rupture may also be seen, although Smithers et al. reported a sensitivity of chest x-ray of around 60% for diaphragm rupture within 48 hours after injury. X-rays of the abdomen are not useful in blunt trauma because they do not assess for solid organ injuries, which are the most commonly injured organs with blunt mechanisms.
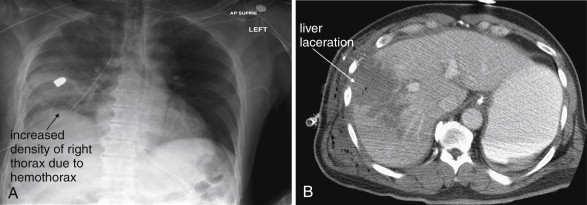
In high-velocity, penetrating abdominal trauma such as gunshot wounds, plain radiographs are commonly obtained, including anterior–posterior (AP) and lateral x-rays of the abdomen, upright AP chest radiograph, and pelvis x-ray. In the case of gunshot wounds, x-rays identify the location and number of retained projectiles. Chest and pelvis x-rays are obtained because of the erratic path of tumbling missiles, which can lead to extra-abdominal injuries. Common findings include free abdominal air (pneumoperitoneum), pneumothorax, and hemothorax. The upright chest radiograph is most sensitive for free air. In penetrating trauma, pneumoperitoneum is generally considered an indication for laparotomy, because of the likelihood of bowel perforation as the source. Plain radiographs may also reveal important bony injuries. Plain radiographic findings of hemoperitoneum and solid organ injury are unreliable, and other imaging modalities are usually relied upon to assess for these.
In abdominal stab wounds, plain radiographs of the chest and abdomen are usually obtained, again to assess for pneumoperitoneum, pneumothorax, or hemothorax, any of which can occur from high abdominal or flank stab wounds.
Ultrasound
Ultrasound has become a common part of the initial assessment of blunt abdominal trauma. Ultrasound serves a screening function because it assesses for the presence of free fluid in the abdomen or pericardium but does not explicitly identify the source. The focused assessment with sonography in trauma (FAST) (also sometimes called focused abdominal sonography in trauma or focused abdominal sonography for trauma) examination has been a standard part of the diagnostic algorithm since the 1990s in most U.S. trauma centers. In the FAST exam, the right upper quadrant (Morison’s pouch, or hepatorenal recess), the left upper quadrant (splenorenal recess), the suprapubic space (pelvis), and the pericardium (usually via a subxiphoid approach) are inspected for anechoic material representing fluid—which in the setting of trauma is assumed to be blood. Advantages of ultrasound include portability (allowing it to be used in the trauma bay during resuscitation), lack of ionizing radiation exposure, repeatability (allowing evaluation of changes in patient condition), and rapidity of the exam. Disadvantages include significant operator dependence, meaning that equal results are not achieved with ultrasonographers of varying experience and ability. Ultrasound is considered most useful in detection of solid organ injuries with associated hemoperitoneum. It is considered insensitive for the detection of bowel or retroperitoneal injuries. More recent studies have focused on the ability of ultrasound to detect pneumoperitoneum and hemopneumothorax (discussed in Chapter 6 on chest trauma). Moriwaki et al. found ultrasound was 85% sensitive and 100% specific for detection of free air in a prospective study of 484 patients. Some small studies have also investigated the utility of ultrasound contrast agents to detect active bleeding.
Ultrasound is relatively sensitive for free abdominal fluid. In one study, in which fluid was instilled into the abdomen in 100-mL aliquots during diagnostic peritoneal lavage (DPL), the median amount of fluid required for identification of an anechoic stripe in Morison’s pouch was 700 mL with the patient in a supine position. Positioning the patient in Tredelenburg (head down) position reduced the detection limit to 400 mL. In a second study, continuous scanning of Morison’s pouch during infusion of DPL fluid revealed a mean detection limit of 619 mL. Only 10% of ultrasonographers (attending physicians and residents in emergency medicine, radiology, and surgery) detected volumes less than 400 mL. The sensitivity at 1 L was 97%.
Ultrasound has been extensively studied in the hands of both emergency physicians and surgeons. In one prospective study of 55 patients, the sensitivity and specificity of ultrasound were 91.7% and 94.7%, respectively, for detection of intraabdominal injury. Another prospective study of 200 blunt trauma patients found ultrasound to be 83% sensitive and 100% specific—although the authors concluded that only a single missed injury was significant. Ma et al. reported sensitivity of 90% and specificity of 99%. A review in 1996 found a paucity of prospective trials of ultrasound and numerous methodologic flaws in those studies. A systematic review and meta-analysis found 123 trials, of which 30 trials met methodologic criteria for inclusion. These trials included 9047 patients and gave a composite negative likelihood ratio of 0.23. Recall that a negative likelihood ratio of 0.1 is generally considered to provide strong evidence of the absence of pathology. In a patient with a pretest probability of abdominal injury of 50%, a negative ultrasound reduces the probability of injury only to around 25%. Ultrasound is not sufficiently sensitive to exclude intraabdominal injury, limiting its utility as a definitive test for abdominal trauma.
What is the role of ultrasound in blunt trauma evaluation? When first introduced, ultrasound was viewed as a potential replacement for DPL. DPL was extremely sensitive for abdominal injuries (100% in many series), but its lack of specificity led to many nontherapeutic laparotomies. Because ultrasound requires the accumulation of greater amounts of peritoneal fluid for detection, it may fail to detect subtle injuries—leading to fewer laparotomies for minor solid organ injuries but also risking missed bowel injuries. With the growth of CT use in evaluation of blunt abdominal injury from the mid-1980s, nonoperative management of most blunt solid organ injuries became the norm, and the information provided by ultrasound became less useful in this setting. Given that a negative ultrasound does not exclude abdominal injury, CT is usually performed in stable patients with possible injury, even following negative ultrasound. CT is also usually performed in stable patients with positive ultrasound findings because further characterization of the source and degree of bleeding can allow nonoperative management, sometimes with angiographic embolization (see Chapter 16 ).
Ultrasound remains useful in the unstable patient. Following blunt trauma, hemodynamic instability is most often because of hemorrhage, with six potential sources: chest, abdomen, pelvis, retroperitoneum, large extremity compartments, and external bleeding sources ( Table 10-1 ). Ultrasound can be used to exclude or confirm substantial abdominal and pelvic free fluid. A negative FAST suggests other sources of hemorrhage. A positive FAST suggests that abdominal bleeding is a significant contributor, potentially leading to immediate laparotomy. In a retrospective study, Farahmand et al. evaluated the performance of ultrasound in hypotensive blunt abdominal trauma patients. Whereas ultrasound was only 85% sensitive for detection of any injury, it was 97% sensitive for surgical injuries with 82% specificity in these patients, suggesting utility in patients too unstable for CT. The treatment priorities for the patient depend on the overall scenario, including the results of chest and pelvis radiographs and the presence of head injury. Patients with significant pelvic bleeding may require angiographic embolization, either before or after laparotomy. Patients with concurrent chest injuries may require thoracotomy or endovascular repair.
| Bleeding Source | Diagnostic Modality | Comments |
|---|---|---|
| Chest | Chest x-ray | A negative chest x-ray (normal mediastinum and no hemo- or pneumothorax) substantially reduces the risk of thoracic hemorrhage as the cause for hemorrhagic shock. |
| Abdomen | Ultrasound (FAST examination) | A negative FAST (ultrasound) examination excludes abdominal bleeding as a likely source of shock, though it does not rule out abdominal injuries. A positive FAST examination identifies significant abdominal bleeding sources. |
| Pelvis | Pelvis x-ray | A normal pelvis x-ray excludes significant pelvic bleeding in most patients. Fractures that destabilize the pelvic ring may be associated with substantial pelvic bleeding (see Chapter 13 ). |
| Retroperitoneum | CT | Retroperitoneal injury is not readily evident from examination, though ecchymosis of the flanks or abdominal wall may be present. X-ray and ultrasound do not screen for this injury well, although by excluding hemorrhage sources in the chest, abdomen, and pelvis, they may identify retroperitoneal injury as a likely source of hemorrhage by process of elimination. CT scan is usually necessary to confirm or exclude retroperitoneal injury. |
| Extremities | Physical examination, x-ray | Examination may reveal significant limb swelling and possible unstable fractures. X-rays confirm fracture. |
| External sources | Physical examination | External bleeding is usually readily visible on examination. |
The role of ultrasound in patients with penetrating abdominal trauma is limited. As described later, CT is increasingly used to evaluate stable patients with penetrating abdominal injury, avoiding laparotomy in some. Because ultrasound does not distinguish between free fluid from penetrating solid organ injury (often managed nonoperatively) and that from hollow viscus injury (managed operatively), it is of little use in stable patients. Unstable patients with penetrating abdominal injury typically are taken rapidly to the operating suite, regardless of ultrasound findings.
Ultrasound can be useful in penetrating abdominal trauma in assessing for hemopericardium. Penetrating abdominal wounds can enter the chest, causing this injury pattern.
Does ultrasound improve clinical outcomes in patients with blunt abdominal trauma? Melniker et al. conducted a prospective randomized controlled trial of ultrasound in the initial evaluation of blunt abdominal trauma. The measured outcomes were time from emergency department arrival to transfer for operative care, CT use, hospital length of stay, complications, and charges. They enrolled 262 patients, and all measured outcomes favored patients undergoing ultrasound and reached statistical significance. Time to operative care was 64% less for ultrasound patients compared to control patients, and ultrasound patients underwent fewer CTs (odds ratio = 0.16), spent 27% fewer days in the hospital, and had fewer complications (odds ratio = 0.16). Charges were 35% less compared to control patients. Although this study appears at first glance to demonstrate a resounding advantage, the study was conducted in centers in which operative management of blunt solid organ injuries was common—not the case in most U.S. medical centers today. As a consequence, the reductions in time to operating room entry, CT use, and cost are unlikely to be reproduced. The study included penetrating and blunt trauma patients, two populations treated with different diagnostic and treatment algorithms in most centers. Other methodologic flaws limit the study, including lack of blinding, failure to enroll consecutive patients, and significant dropout rate (17%) after enrollment. The study did not control for the availability of operative care, which may have been the largest factor in the measured difference in time to operating room entry.
Computed Tomography
CT is discussed in detail later, including sensitivity for solid and hollow organ injuries in the setting of both blunt and penetrating trauma. For most stable trauma patients, CT has become the definitive imaging modality of choice when intraabdominal injury is suspected. CT is rapid and highly sensitive and specific for many important injury types. The information provided by CT allows prognosis of injury and selective nonoperative management in both blunt and penetrating trauma. CT is less sensitive for some important injuries, including bowel and diaphragmatic trauma, a limitation that must be recognized to prevent clinical errors following a negative CT.
Imaging Algorithms in the Unstable and Stable Abdominal Trauma Patient
Patients with hemodynamic instability should be assumed to have hemorrhagic shock as the most likely source, with obstructive shock (tension pneumothorax or pericardial tamponade) or distributive shock (spinal cord injuries) being exceedingly rare by comparison. Imaging in the emergency department should be performed quickly, with the goal of triage to the operating room or angiography suite if necessary. Sources of hemorrhage fall into six categories (see Table 10-1 ), which can be evaluated in the trauma bay using ultrasound and portable plain radiographs. Pericardial tamponade can be evaluated with bedside ultrasound as described in Chapter 6 . Although tension pneumothorax is often described as a clinical diagnosis never to be made radiographically, rapid chest x-ray or bedside ultrasound can be used to evaluate for this condition (see Chapter 6 ).
No further emergency department imaging may be needed in a hemodynamically unstable patient with a single identified source of hemorrhagic shock. Patients with shock and abdominal or chest injuries typically are taken to the operating suite for surgical intervention. Patients with pelvic injuries resulting in shock usually receive external pelvic fixation and pelvic angiographic embolization of actively bleeding vessels. Preperitoneal packing is also sometimes used to tamponade bleeding. Patients with extremity hemorrhage or active external bleeding are usually treated with limb splinting and local compression to limit bleeding. If these interventions plus fluid resuscitation succeed in stabilizing the patient, then additional imaging with CT can be performed to evaluate more comprehensively for injuries.
Hemodynamically stable patients can be evaluated with plain radiographs followed by CT in patients with suspicion of injury, based on clinical judgment or published clinical decision rules (described later). Some patients with minimal trauma mechanism and no signs or symptoms of injury require no imaging. Stable blunt trauma patients with suspected abdominal injury usually undergo CT. In some centers, stable penetrating trauma patients without pneumoperitoneum on x-ray also are evaluated with CT, allowing nonoperative management for those without CT evidence of peritoneal violation and in those with isolated solid organ injury. In other centers, laparotomy or laparoscopy is performed rather than diagnostic imaging with CT.
Computed Tomography in Trauma: Indications for Contrast Agents
Blunt Trauma: Indications for CT Contrast Agents
For the evaluation of blunt abdominal or flank trauma, intravenous (IV) contrast should be routinely used, but oral contrast should not. The American College of Radiology recommends the use of 150 mL of intravenous contrast, infused at 2-4 mL per second, with CT being performed after a 60 second delay. Without any contrast agents, CT can reveal several important imaging findings. Free air, while rare following blunt trauma, is readily seen without any contrast agents. Air appears black on all window settings and is even more readily visible on lung or bone windows than on soft-tissue (abdominal) window settings (see Chapter 9 ). Free abdominal fluid representing hemoperitoneum is also readily seen on noncontrast CT. Simple fluid such as simple ascites or urine has a Hounsfield density on CT of 0 Hounsfield units (HU), whereas blood has a density of around 45 HU (though the exact value likely varies with time since hemorrhage and hematocrit). Using a digital radiology display called a picture archiving and communication system (PACS), the density of organs and fluid collections can be measured. On a noncontrast CT, blood appears slightly darker gray on soft-tissue windows than do solid organs such as the liver and spleen because these organs are slightly denser (around 100 HU).
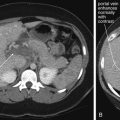
The liver, spleen, kidneys, vascular structures, bones, bladder, and peritoneal fat are also visible on noncontrast CT. Use of bone windows and reconstructions to evaluate the spine and bony pelvis is discussed in Chapter 3 , Chapter 13 . With the addition of IV contrast, several additional important features can be seen. First, solid organs such as the liver, spleen, and kidneys are highly vascular and intensely enhance with injected contrast on arterial phase imaging (CT images acquired at a moment coinciding with the injected contrast bolus reaching arterial beds). Enhancement is visible as a brightening or whitening of the organ because of the distribution of high-density injected contrast throughout the organ parenchyma. A normal solid organ enhances relatively uniformly. Injured areas of these solid organs fail to enhance with IV contrast because they no longer receive a normal blood supply. These regions appear darker than (“hypodense” relative to) the surrounding normally perfused organ. Areas of injury are variously described as contusions, lacerations, and contained hematomas —but these terms are essentially synonyms for regions of solid organs that do not enhance with IV contrast, indicating poor perfusion of that organ segment. Without the addition of IV contrast, these regions may be less conspicuous because the density of normal solid organs is similar to that of an injured region without IV contrast. A large area of injury may be visible on noncontrast CT if the density is sufficiently decreased by accumulated blood.
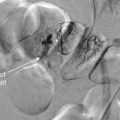
IV contrast serves a second important function: revealing active hemorrhage from injuries. With the injection of contrast, a blush of contrast on arterial phase imaging within a hypodense injured solid organ indicates active bleeding. This must be distinguished from normal enhancement of vessels within solid organs, such as portal and hepatic vessels within the liver. These normal vessels are surrounded by enhanced normal tissue on CT images. On the other hand, active bleeding within an area of injured organ appears as a bright white spot of contrast, surrounded by the hypoattenuated (darker gray) region of injury. Active bleeding into the peritoneal cavity can also be seen with injection of IV contrast. In this case, blood that had escaped into the peritoneal cavity before the moment of contrast injection and CT acquisition appears dark (around 45 HU) on soft-tissue windows. Active bleeding at the moment of CT acquisition appears as a bright white spot or amorphous patch within this hypoattenuated region of injury.
If noncontrast CT can reveal hemoperitoneum and even large areas of solid organ injury, why is IV contrast of value? In a stable patient, hemoperitoneum and even large regions of solid organ injury are often managed nonoperatively. On the other hand, active bleeding revealed by injected IV contrast predicts the need for either operative management or, more commonly today, angiographic embolization to stop hemorrhage. Angiographic embolization is discussed in more detail in Chapter 16 .
IV contrast can also reveal hypoperfused organs resulting from vascular pedicle injuries. In this case, the organ appears hypodense (dark gray), failing to enhance normally following IV contrast administration. This is an indication for laparotomy, either for vascular repair to salvage the organ or for organ removal to prevent hemorrhage. Active bleeding from an injured vessel may be visible but may be limited acutely by vasospasm. Bowel injuries are sometimes recognized with the addition of IV contrast. A regional bowel injury may result in hypoattenuation of the bowel wall because IV contrast does not perfuse the injured segment.
Other injuries can be revealed by injected IV contrast. Although contrast is injected intravenously, not intra-arterially, for CT, the CT image acquisition is usually timed to coincide with arterial perfusion, so arterial bleeding may be seen directly. The timing of the CT may be intentionally selected to represent an intermediate phase of perfusion, when both arterial and venous structures are filled with contrast. Sometimes, additional “delayed” CT images are acquired following the initial CT. These additional images are obtained seconds to minutes after the injected contrast bolus to allow visualization of venous structures, venous phases of solid organ perfusion, and even renal perfusion and excretion of contrast. The use of delayed images to evaluate renal and ureteral injuries is discussed in detail in Chapter 12 .
Oral contrast is not indicated for the evaluation of blunt trauma patients. Intuitively, it seems logical that addition of oral contrast might assist in recognition of bowel injuries. A bowel injury might result in bowel perforation, characterized by leak of contrast from the bowel lumen into the peritoneal cavity. Alternative, a contused and thickened bowel wall might be more visible if the bowel lumen were opacified with contrast. These theoretical benefits have not been demonstrated in clinical trials. In multiple large studies, CT without oral contrast performed comparably to CT with oral contrast. In its appropriateness criteria for blunt abdominal trauma, the American College of Radiology states “CT evaluation of the abdomen and pelvis for blunt trauma does not require the use of oral contrast.”
Clancy et al. reviewed 492 abdominal CTs for blunt trauma and compared CT interpretation with operative findings and clinical follow-up. Oral contrast was used in only 8 patients. Only 1 of 372 patients with a negative non–oral contrast CT required surgery. Five bowel injuries were found in 42 patients who underwent operation, and the authors claimed that oral contrast would not have ensured preoperative diagnosis, although their retrospective methods cannot prove this assertion.
Stafford et al. randomized 594 adult blunt trauma patients to receive oral contrast or no oral contrast before CT with IV contrast. Six bowel injuries were identified at laparotomy in the oral contrast group, and three were identified in the non–oral contrast group. One small-bowel injury was missed by CT in the 199 patients receiving oral contrast. No small-bowel injuries were missed by CT in the 195 patients receiving no oral contrast.
Allen et al. prospectively enrolled 500 consecutive adult blunt trauma patients and performed CT with IV contrast only to determine the sensitivity for blunt bowel and mesenteric injury. They compared the initial clinical CT interpretation to a composite criterion standard of laparotomy results, autopsy results, a research study–only CT reading, and clinical follow-up to determine the presence or absence of injury. CT without oral contrast was 95% sensitive and 99.6% specific, comparing favorably with the reported sensitivity of oral contrast–enhanced CT. In a separate report from the same study, the authors reported the sensitivity and specificity of CT without oral contrast for blunt diaphragmatic injury (66.7% and 100%, respectively).
Stuhlfaut et al. retrospectively reviewed records of 1082 patients undergoing multidetector CT without oral contrast to determine the sensitivity of CT for bowel and mesenteric injury requiring surgical repair. The criterion standard was a composite of laparotomy report and hospital course. CT was considered positive for bowel or mesenteric injury if findings included pneumoperitoneum with other secondary findings ( n = 4), mesenteric hematoma and bowel wall abnormality ( n = 2), mesenteric hematoma only ( n = 4), or bowel wall thickening only ( n = 4). CT was considered negative for bowel or mesenteric injury if findings included no intraabdominal injury, solid organ injury only, or free fluid only. Sensitivity was 82%, with a 95% confidence interval (CI) of 52% to 95%, and specificity was 99% (95% CI = 98%-99%), similar to prior studies of CT with oral contrast.
Holmes et al. retrospectively reviewed records of 6052 consecutive blunt trauma patients undergoing CT with IV but without oral contrast to determine the sensitivity of CT for gastrointestinal injury. Injuries were confirmed by laparotomy, autopsy, or additional (non-CT) imaging studies. Out of 106 patients with confirmed gastrointestinal injuries, CT was abnormal in 91 patients (86%, 95% CI = 78%-92%). CT specifically suggested gastrointestinal injury in 81 patients (76%, 95% CI = 67%-84%). CT specifically suggested gastrointestinal injury in 58 of 64 patients (91%, 95% CI = 81%-96%) with major gastrointestinal injuries, defined as gastrointestinal perforation, active mesenteric hemorrhage, or mesenteric devascularization.
Why did these trials fail to demonstrate an anticipated benefit of oral contrast? Several factors may contribute. First, some bowel injuries are seen on CT without oral contrast. Bowel injuries may be suggested from free air, hypoperfusion of a segment of bowel following IV contrast administration, thickening of the bowel wall, infiltration of the mesenteric fat surrounding the bowel, or free peritoneal fluid without an evident solid organ injury. None of these findings requires oral contrast for detection. Although these findings are nonspecific, they may be sufficient to prompt appropriate management (observation or surgical exploration). Second, many bowel injuries do not result in frank perforation, at least initially. Instead, the bowel wall may be contused but not violated. As a result, oral contrast may not leak into the peritoneal cavity. Other injuries may be microperforations that seal spontaneously or do not lie in dependent loops of bowel where contrast could escape. Third, if CT is performed rapidly following oral contrast administration, or if injuries or drugs slow gastrointestinal transit of contrast, orally administered contrast may not reach an injured segment of bowel to aid in diagnosis.
Finally, bowel injuries are quite rare, occurring in only about 1% of blunt abdominal trauma. Consequently, even large studies may fail to demonstrate a moderate benefit of oral contrast. For example, in a population of 1000 blunt trauma patients, only about 10 bowel injuries would be expected. If oral contrast enabled detection of 8 of 10 injuries, whereas 5 of 10 were detected without oral contrast, a real difference might exist, but the difference would be too small to be statistically significant. A very large study of thousands of patients would be required to confirm a difference of this magnitude. From a practical standpoint, however, the number needed to treat (by administering oral contrast) to detect a single additional bowel injury would be several hundred. While bowel injuries are important and might seem to justify the treatment of many patients to prevent a single missed injury, oral contrast has potential harms. Oral contrast takes time to ingest and transit through bowel before CT, potentially wasting precious time in a patient with other life-threatening injuries. In addition, many blunt abdominal trauma patients are intoxicated, have head injuries, or are immobilized supine because of suspected spine trauma—making ingestion of oral contrast a potential aspiration hazard, though likely a rare event. In one retrospective review of 506 consecutive trauma patients undergoing CT with oral and IV contrast, one patient was noted to have instillation of enteral contrast through a nasogastric tube inadvertently placed into the right main bronchus rather than the stomach.
Penetrating Trauma: Can “Triple-Contrast CT” Guide Nonoperative Management?
Historically, penetrating trauma of the abdomen or flank was evaluated with surgical exploration (laparotomy), laparoscopy to inspect for peritoneal violation, or local wound exploration. More recently, selected stable patients have been evaluated with so-called triple-contrast CT (CT with oral, IV, and rectal contrast). IV contrast in this setting serves the same functions as in blunt trauma, discussed in detail earlier. Oral and rectal contrast agents are used for the theoretical benefit of demonstrating leak of contrast from the bowel lumen into the peritoneum or retroperitoneum.
As we discussed earlier, oral contrast has not been shown to be diagnostically beneficial in blunt abdominal trauma. Theoretically, oral and rectal contrast might be more useful in penetrating injuries, in which bowel penetration is a more common injury, and in which larger defects in the bowel wall might be expected. However, multiple studies have failed to show contrast leak from the bowel lumen to be a sensitive indicator of hollow viscus injury. In one prospective study of 200 patients, only 19% of patients with proven bowel injury had contrast leak from bowel observed on CT. In comparison, a wound track near the bowel was 77% sensitive. Given this, are oral and rectal contrast agents truly essential in the setting of penetrating trauma? A single study has evaluated the sensitivity and specificity of “single-contrast CT” (CT with IV contrast and no oral or rectal contrast) for penetrating abdominal or flank injuries. Ramirez et al. retrospectively reviewed 10 years experience with IV contrast–only CT for evaluation of penetrating torso trauma in 306 hemodynamically stable patients. CT predicted “need for laparotomy” with 98% sensitivity and 90% specificity, a positive predictive value of 84%, and a negative predictive value of 99%. In 222 patients with gunshot wounds, the authors reported 100% sensitivity and a 100% negative predictive value, whereas they found 92% sensitivity and a 97% negative predictive value in patients with stab wounds. Although the authors did not compare the sensitivity and specificity of CT with IV contrast to triple-contrast CT, their results are comparable to those reported in studies of triple-contrast CT, described later. Like many retrospective studies, this study suffers from a mixed criterion standard that includes laparotomy and clinical course. The authors did not report the duration of clinical follow-up and losses to follow-up, raising the possibility that some injuries might have been missed by CT. Unlike some other studies, this study focused on prediction of “need for laparotomy” rather than sensitivity for peritoneal violation. Unfortunately, the authors did not categorize the laparotomy results (therapeutic, nontherapeutic, and negative). Because the surgeons in this study were not blinded to the CT results, they assuredly were influenced by the CT findings in their decision to operate. As a consequence, the reported performance of the CT is affected by incorporation bias. Nevertheless, the authors pointed to significant time savings by avoiding oral and rectal contrast agents.
Demetriades et al. prospectively studied alert hemodynamically stable patients without findings of peritonitis on examination following penetrating abdominal injury. Unstable patients, patients with peritonitis, and those who could not be evaluated clinically underwent immediate laparotomy. Of 152 patients, 61 (40.1%) met criteria for CT evaluation with IV but without oral or rectal contrast. Patients without CT findings of hollow viscus injury were observed with serial exams and laboratory evaluation for falling hematocrit or developing leukocytosis. The authors found that 43 patients with 47 solid organ injuries (liver, spleen, and kidney) had no CT evidence of hollow viscus injury by CT. Because of CT evidence of active bleeding, 4 patients underwent angiographic embolization of the liver. Whereas 41 patients (27% of total) were managed nonoperatively, 3 patients failed nonoperative management but recovered without complications after laparotomy, and 2 patients underwent laparoscopy to evaluate for possible diaphragm injury, given the relatively low reported sensitivity of CT for this injury pattern.
Inaba and Demetriades reviewed the indications for laparotomy in penetrating abdominal injury. Hemodynamically stable patients without examination findings of peritonitis can be managed nonoperatively with careful observation. Gunshot wounds to the abdomen can be imaged with CT to determine projectile trajectory and likely injuries. Peritoneal violation on CT without evidence of organ injury can be managed nonoperatively with careful serial examinations. Solid organ injuries can be managed with endovascular therapies, primarily embolization for control of hemorrhage. Evidence of hollow viscus injury on CT warrants surgical exploration.
Mitra et al. retrospectively reviewed all patients with penetrating abdominal injury over a 5-year period and found 36 hemodynamically stable patients undergoing CT for evaluation. The authors did not identify the CT protocol used, although they specified that triple contrast was not used. They reported a 77.8% combined sensitivity of CT and ultrasound in these patients.
Beekley et al. retrospectively reported on 145 stable patients in a military combat support hospital without peritonitis following penetrating abdominal shrapnel wounds. Patients were routinely evaluated with CT with IV contrast; oral contrast was used “rarely” and rectal contrast was used in 2 cases. Patients with no CT findings of intraperitoneal or retroperitoneal penetration were managed nonoperatively. Based on CT, 85 (59%) of patients were managed nonoperatively, and 60 (41%) underwent laparotomy. The authors reported that 75% of laparotomies were therapeutic. Negative CT missed 1 patient with an intraabdominal injury requiring laparotomy (sensitivity = 97.8%, specificity = 84.8%, negative predictive value = 99%).
A number of studies have evaluated the safety and sensitivity of the triple-contrast CT approach. Multiple large series and a metaanalysis report good outcomes with conservative nonoperative management following a CT showing no evidence of bowel injury. We discuss these shortly, but first consider some limitations. First, publication bias may skew the reported literature on this topic, with authors not reporting failures of this technique. Second, many of the published studies suffer from limited clinical follow-up, raising the possibility of missed injuries not recognized by the researchers. Third, the indications for conservative management with CT include a reassuring physical exam. Because different physicians may interpret the physical examination differently, it is unclear how safe the practice would be outside of the major trauma centers that are the source of much of the data.
Hauser et al. retrospectively reviewed 40 cases of posterior abdominal penetrating injuries evaluated with CT using IV, oral, and rectal contrast. They found 6 of the 40 cases to have abdominal injury by CT, confirmed by laparotomy. Although 34 patients without CT evidence of peritoneal or retroperitoneal organ injury were observed for 72 hours and discharged without laparotomy, lack of long-term follow-up prevents certainty that no injuries were missed.
Himmelman et al. prospectively enrolled 88 hemodynamically stable patients with penetrating back or flank wounds. In 9 patients, CT suggested surgical injuries; 5 of these underwent laparotomy, with 2 having significant injuries. The other 79 patients had no CT findings suggesting need for surgery, and 77 of them were observed for 48 hours without complications. Because of positive DPL, the remaining 2 patients underwent laparotomy, negative in both cases. The authors concluded that a reassuring CT had a 100% negative predictive value for injuries requiring surgical repair.
McAllister et al. reported on 53 hemodynamically stable patients with stab wounds to the back, evaluated with triple-contrast CT if local wound exploration showed muscle fascia penetration. Of the 53 patients, 51 had negative CT or injuries not requiring surgery and did well with nonoperative management. Two CTs demonstrated injuries requiring therapeutic celiotomy. The authors concluded that CT was accurate in detection of occult injury but was costly and did not contribute to clinical management decisions—a peculiar conclusion given that the authors did not assess the planned management from clinicians blinded to the CT results.
Soto et al. reported on 32 stable patients examined with triple-contrast CT and serial ultrasound following penetrating abdominal stab wounds. One patient had CT findings of extensive hepatic laceration and massive hemoperitoneum and was managed operatively. The other 31 patients were managed nonoperatively based on CT and ultrasound findings and were asymptomatic at 28-day follow-up. Of these patients, 21 had some form of intraperitoneal injury but without evidence of bowel injury. The small number of patients in this series, and the limited number of significant injuries, limit the external validity of this study.
Chiu et al. retrospectively reviewed 75 hemodynamically stable patients undergoing triple-contrast CT following penetrating torso trauma. Patients with negative CT or isolated solid organ injury were observed, whereas those with any other evidence of peritoneal violation (free air or fluid, contrast leak, or nonsolid visceral injury) underwent laparotomy. In patients with negative CT, 47 of 49 (96%) had successful nonoperative management, 1 had negative laparotomy, and 1 had a left diaphragmatic injury. In patients with positive CT, 15 of 18 had therapeutic laparotomy. Whereas 5 patients had isolated hepatic injuries, 2 had hepatic and diaphragmatic injuries, managed with angiographic embolization and thorascopic diaphragmatic repair. The authors concluded that CT is useful in selecting patients for nonoperative management, although solid organ injuries and diaphragmatic injuries may require invasive therapies.
Shanmuganathan et al. prospectively studied triple-contrast helical CT in predicting peritoneal violation and need for laparotomy following penetrating torso trauma in 104 hemodynamically stable patients (54 gunshot wounds and 50 stab wounds). A positive CT was defined as evidence of peritoneal violation or injury to the retroperitoneal colon, a major vessel, or the urinary tract. Laparotomy was performed in patients with a positive CT except in those patients with isolated liver injury or free fluid. Patients with negative CT were initially observed. Among those with positive CT, 19 (86%) had therapeutic laparotomy. Whereas 9 patients with isolated hepatic injury on CT were successfully managed nonoperatively, 67 of 69 patients (97%) with negative CT had successful nonoperative management. The authors reported 100% sensitivity and 96% specificity of CT, although they failed to account for the operative management in 2 patients with negative CT.
In a separate report, Shanmuganathan et al. reported on 200 hemodynamically stable penetrating trauma patients without peritoneal signs or radiographic (x-ray) findings of pneumoperitoneum. The group included 86 patients with gunshot wounds, 111 with stab wounds, and 3 sharp impalements. Triple-contrast CT was prospectively evaluated by three radiologists for peritoneal violation and injury to intra or retroperitoneal solid organs, bowel, mesentery, vascular structures, diaphragm, and urinary tract. CT was 97% sensitive for peritoneal violation requiring laparotomy and diagnosed 28 hepatic, 34 bowel or mesenteric, 7 splenic, and 6 renal injuries. Laparotomy based on CT findings was therapeutic in 87% of patients. Two patients with negative CT required therapeutic laparotomy.
Conrad et al. retrospectively reviewed the charts of 81 patients who had emergency department workup for penetrating truncal trauma using triple-contrast CT. Following negative CT, 62 patients were discharged from the emergency department. Two missed injuries were identified but had no complications according to the authors. The authors concluded that emergency department discharge is a safe disposition; unfortunately, nearly one third of those discharged had no follow-up, rendering uncertain the outcomes of this strategy. If a significant percentage of the patients lost to follow-up had missed injuries, emergency department discharge following a negative CT would be unacceptable.
Loberant and Goldfeld provided a case report of a patient undergoing a negative laparotomy because of a bony fragment mistakenly identified as contrast extravasation on triple-contrast CT.
Dissanaike et al. reported a series of 9 patients evaluated with triple-contrast CT, with no missed injuries following nonoperative management of patients with negative CT. Clearly, the small numbers of patients in this series limit the value of the study.
Goodman et al. performed a metaanalysis to determine the predictive value of CT for laparotomy in hemodynamically stable patients with penetrating abdominal trauma. They identified 180 studies but included only 5 because of methodologic concerns. The pooled sensitivity, specificity, negative predictive value, positive predictive value, and accuracy were 94.90%, 95.38%, 98.62%, 84.51%, and 94.70%, respectively. This meta-analysis included studies using both single-contrast and triple-contrast techniques and thus does not clarify the necessity for contrast agents.
Overall, triple-contrast CT appears to be a safe management strategy in highly selected stable patients without peritonitis on examination. Losses to follow-up, variable inclusion criteria, and the likelihood of publication bias favoring positive outcomes in the published studies all contribute to a need for caution with a negative CT. Multiple studies have demonstrated the possibility of missed diaphragmatic injuries and, rarely, missed operative bowel injuries. Following a negative triple-contrast CT, observation or close follow-up should be ensured. Further study is needed to determine the true diagnostic value of oral and rectal contrast in this setting.
Interpretation of Images
Interpretation of X-Ray
Interpretation of chest and pelvis x-rays for trauma is described in detail in Chapter 6 , Chapter 13 , respectively. In blunt abdominal trauma, abdominal radiographs are not useful and should not be obtained. The chest x-ray should be evaluated for signs of free air (see Figure 6-11 , Figure 9-7 ), although the trauma chest x-ray is usually obtained in a supine position and is insensitive for pneumoperitoneum. The chest x-ray can reveal diaphragmatic rupture (see Figures 10-30 and 10-33 later in the chapter), more commonly on the left than on the right. Signs of diaphragm rupture include an elevated hemidiaphragm and herniation of abdominal contents into the thorax. If a nasogastric tube has been placed, it may be seen curling in the thorax. The gastric air bubble may be seen in an abnormally elevated position.
In penetrating abdominal trauma, an upright chest x-ray should be obtained to increase the sensitivity for free air. The subdiaphragmatic region should be inspected for lucencies suggesting pneumoperitoneum (see Figure 6-11 , Figure 9-7 ). The abdominal, chest, and pelvis x-rays should be inspected for retained missile fragments (see Figure 10-9 ) in the case of gunshot wounds. Bony injuries, particularly spine and pelvic fractures, should be sought. Hemothorax (see Figures 10-9 and 10-35 ) and pneumothorax are other common findings in this setting.
Interpretation of Ultrasound
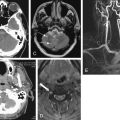
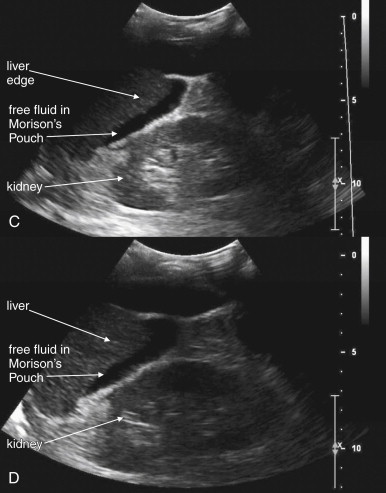
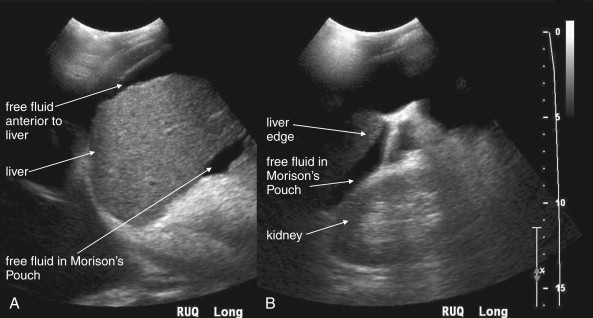
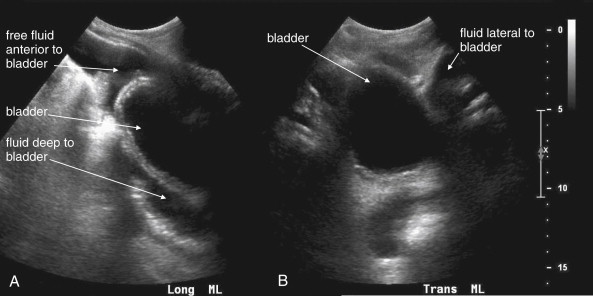
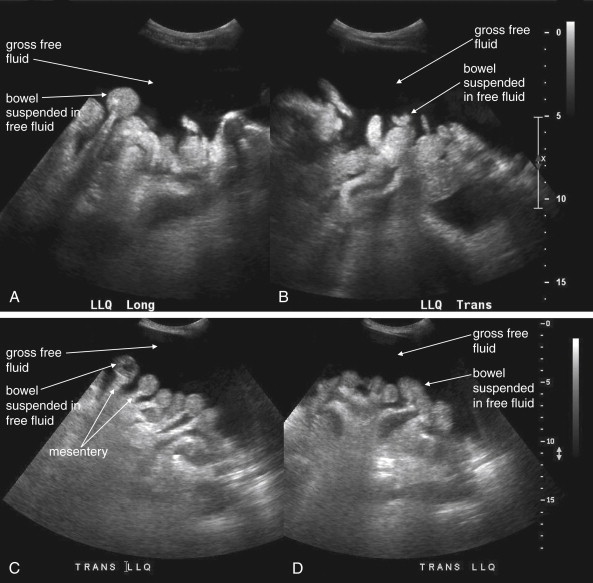
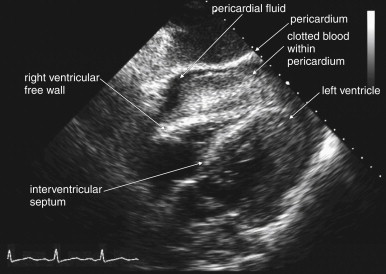
The key radiographic finding in ultrasound of blunt and penetrating abdominal trauma is free fluid, which is assumed to be hemoperitoneum in the setting of trauma. Patients with medical conditions causing preexisting ascites can have false-positive ultrasound exams in this setting. Fluid is anechoic (black) on ultrasound. In the case of small amounts of hemoperitoneum, fluid may be visible only as an anechoic stripe separating the liver and the kidney on the right ( Figure 10-1 ), or the spleen and the kidney on the left ( Figure 10-2 ). Fluid may also accumulate between the spleen and diaphragm. Free fluid pooled in the pelvis is visible as anechoic collections lateral to the bladder on a transverse view ( Figure 10-3 ). Free fluid may also be visible in the rectouterine recess (pouch of Douglas) in females using a sagittal view (see Figure 10-3 ). In cases of gross hemoperitoneum, loops of bowel may be seen floating in blood ( Figure 10-4 ). In some cases, coagulated blood may take on a more echogenic appearance or fibrinous strands may be seen suspended in anechoic collections. Abdominal trauma can also cause hemopericardium, visible as an anechoic layer surrounding the heart on a subxiphoid view ( Figure 10-5 ).

Pneumoperitoneum is also sometimes visible on ultrasound. Air is hyperechoic and disrupts the ultrasound beam, preventing visualization of deeper structures. Because bowel gas is normally present in the anterior midline abdomen, free air should be sought overlying the liver, where air is not normally present.
Interpretation of Computed Tomography
Approach to Abdominal CT
For the emergency physician, a systematic and targeted approach allows rapid and accurate identification of important injuries on abdominal CT. Because multiple injuries are common following abdominal trauma, it is extremely important to inspect all major abdominal structures. A common pitfall is to end the search after detection of a single injury. Three window settings are useful in evaluating abdominal structures: soft-tissue (sometimes called abdominal or vascular) windows, lung windows, and bone windows. Soft-tissue windows are used to assess solid organs and hollow organs, to detect free fluid, and to detect free air. Lung windows are used to assess for pneumothorax (recall that the lower lungs and pleural spaces are visible on the cephalad-most abdominal CT slices) and pneumoperitoneum, as described later. Bone windows are used to assess for fractures but can also reveal pneumoperitoneum. We recommend evaluating soft-tissue windows first, followed by lung windows, followed by bone windows. Window settings are discussed in more detail in Chapter 9 . In the descriptions of traumatic injuries that follow, soft-tissue windows are the appropriate setting for evaluation unless stated otherwise.
On soft-tissue windows, evaluate each organ in turn, rather than attempting to evaluate multiple structures on each slice. For example, follow the spleen through all CT slices in which it appears, evaluating for splenic injury. Do not attempt to evaluate the liver, kidneys, or pancreas during this process, even though they are visible, because this may distract you from a splenic injury. After completing evaluation of the spleen, repeat this process with other organs.
Common and Serious Injury Patterns on Computed Tomography
Imaging Findings of Shock: Inferior Vena Cava and Bowel
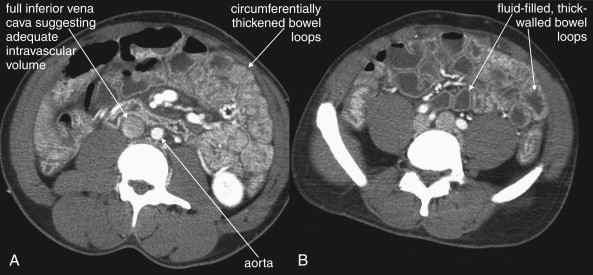
In cases of severe volume depletion (generally from hemorrhagic shock following trauma), the infrahepatic inferior vena cava (IVC) appears flattened ( Figure 10-6 ; see also Figure 10-20 ). This appearance can occur in patients before the development of clinical hypotension or hemodynamic collapse and demands immediate volume resuscitation. Rarely, it may be a normal variant. In a series of 100 trauma patients, a flattened IVC occurred in 7, 6 of whom had other evidence of severe blood loss. In 100 patients without trauma, a flattened IVC was not seen.

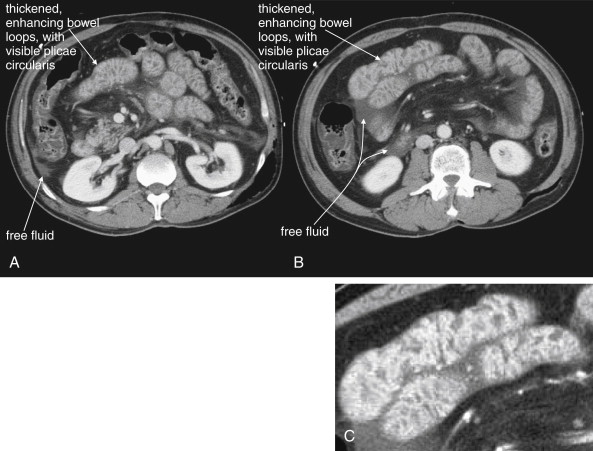
Shock bowel is a term for secondary bowel injury resulting from sustained systemic hypotension. The CT appearance includes diffuse bowel wall thickening, visible on CT without oral contrast ( Figures 10-7 and 10-8 ). This is in contrast to primary small-bowel traumatic injuries, which usually show focal regions of bowel wall thickening. Shock bowel is variably associated with IVC and aortic flattening, abnormal pancreatic enhancement and peripancreatic fluid, and poor enhancement of the spleen and liver because of hypotension. This constellation of findings is sometimes called the CT hypotension complex and has been reported in other conditions, including head and spine injury, post–cardiac arrest, septic shock, and diabetic ketoacidosis.
Pneumoperitoneum
Pneumoperitoneum is rare following blunt abdominal injury but can indicate bowel perforation. When detected on CT, it is not specific for bowel injury because air tracking from thoracic injuries can collect in the abdomen. Following penetrating abdominal injury, pneumoperitoneum detected on CT is likely to indicate bowel perforation and prompts laparotomy in most cases.
On soft-tissue windows, air including pneumoperitoneum appears black ( Figures 10-9 and 10-10 ; see also Figure 10-24 ). Large amounts of pneumoperitoneum are usually visible on this window setting, but smaller collections are more difficult to recognize because intraperitoneal and retroperitoneal fat appears quite dark on soft-tissue windows. On lung windows, all soft tissues and bones appear white, leaving only air black—thus emphasizing both pneumoperitoneum and bowel gas (see Figures 10-10 and 10-24 , B ). On bone windows, bone appears white or light gray, and all soft tissues are an intermediate gray, making black air readily visible. During trauma CT, the patient is generally supine, so pneumoperitoneum collects in the anterior midline and perihepatic spaces preferentially (60% in one study) rather than in a subdiaphragmatic location, as occurs on upright chest x-ray. Air can collect in other locations, including the pelvis and mesentery. CT can detect air collections as small as 1 mm.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree