The neoplastic lesions that can be found in the sinonasal space are numerous and varied. This article describes a general approach to narrowing down the differential diagnosis and provides the treating physician sufficient information to choose and deliver the best treatment modality. Computed tomography and MR imaging together provide complete radiologic assessment of sinonasal neoplasms.
Computed tomography and MR imaging complement each other in a complete evaluation of a sinonasal neoplasm.
Computed tomography and MR imaging complement each other in a complete evaluation of a sinonasal neoplasm.
Computed tomography and MR imaging
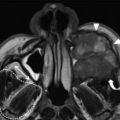
Only the superficial extent of a sinonasal neoplasm is visible on clinical examination and nasal endoscopy. The complete investigation of a sinonasal neoplasm mandates cross-sectional imaging. Both CT and MR imaging have played synergistic roles in the assessment of neoplasms of the sinonasal space.
Radiation issues for CT continue to stimulate debate around the world. The new, sensitive multidetecter scanners are significantly dose efficient, with resultant low mAs scans reducing the radiation dose delivered, yet maintaining spatial resolution. Because the coronal reconstructions from axial scans in multidetector CT allow the required quality, there is no need for the direct coronal scans, thereby reducing radiation dose further. Of particular concern has been the dose delivered to the lens and thyroid gland. It has been shown conclusively that, even after multiple scans, patients have a negligible risk for premature cataract formation and thyroid cancer.
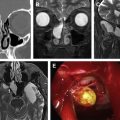
PNS is common in cases of adenoid cystic carcinoma ( Fig. 8 ). This phenomenon is also seen in melanoma and lymphoma. A few benign lesions like sarcoidosis can also show PNS.
The radiologic features of metastatic disease in a node are size greater than 1 cm, capsular invasion, and necrosis. Diffusion-weighted MR imaging and apparent diffusion coefficient values as well as dynamic contrast-enhanced MR imaging have been used to enhance the specificity of this diagnosis.
Contraindications for surgical extirpation of sinonasal neoplasms are controversial at best. Every case needs a multidisciplinary approach for management based on their merit. However, contraindications for surgery can include involvement of the nasopharynx, clivus, bilateral orbital cavities, or optic nerves. Involvement of the carotid artery is a relative contraindication for surgery. Brain or cavernous sinus involvement has been considered unresectable, but surgical management has also been described. Spread to the brain from sinonasal neoplasms is in a contiguous manner and resection of the portion of the gyrus rectus of the frontal lobe usually results in minimal functional deficits. Surgical resection of the cavernous sinus, in view of the extensive venous network and carotid artery, is an extremely challenging task and is associated with significant morbidity and a poor outcome. Very carefully selected patients must be considered for surgical resection in cases of cavernous sinus involvement. The limitations and indications for excision also depend on the abilities and experience of the surgical team.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree