Diagnostic imaging plays a critical role in the evaluation of many patients with blunt and penetrating chest trauma. In this chapter, we discuss the indications for imaging with chest x-ray, ultrasound, and computed tomography (CT). We review a systematic approach to interpretation of chest x-ray and CT. We also discuss and compare imaging findings of key thoracic injuries using chest x-ray, CT, and ultrasound in those cases where it is commonly applied. Our discussion highlights current controversies in imaging of thoracic trauma.
Thoracic Imaging Modalities
The major diagnostic imaging modalities for blunt and penetrating chest trauma are chest x-ray, ultrasound, and chest CT with intravenous (IV) contrast. Aortography is more rarely used, most often following an abnormal chest x-ray or CT result. We review these modalities here, including a detailed discussion of the indications for and interpretation of each imaging technique.
In this chapter, figures are clustered by patient to illustrate injuries using multiple modalities. As a consequence, the order of reference to figures in the chapter is not always sequential.
Chest X-ray
Chest x-ray is the most commonly used diagnostic modality for all forms of chest trauma. Benefits of chest x-ray include portability (allowing it to be used in the resuscitation bay without moving an unstable patient), speed of acquisition (seconds) and image availability (minutes), low expense (approximately $50 to $100), and low radiation exposure (0.01 mSv, equivalent to 1 day’s background exposure on Earth) ( Table 6-1 ).
| X-ray | Ultrasound | CT | |
|---|---|---|---|
| Portable | Yes | Yes | No |
| Speed | Seconds to acquire, minutes to view | Instantaneous acquisition, simultaneous viewing | Seconds to acquire, minutes to view |
| Expense | $50-$100 | Depends on local institution; is usually performed by emergency physician; and may be billed separately as a procedure at some institutions | Approximately $1000 charge to patient, around $100 institutional cost |
| Radiation exposure | 0.01 mSv, 1 day on Earth | None | 4-20 mSv, several years on Earth |
| Information provided |
|
| Detailed information about
|
Clinical Decision Rules: Which Patients Require Chest X-ray?
Chest x-ray historically has been routinely recommended following blunt or penetrating chest trauma. However, a number of studies have examined the sensitivity of history and physical examination in detection of thoracic injury in children and adults. These studies suggest that in stable and alert blunt trauma patients, injuries are extremely rare with a normal thorax examination and the absence of chest complaints.
Bokhari et al. performed a prospective study of 523 stable patients with blunt trauma and 153 stable patients with penetrating trauma ( Box 6-1 ). Before chest x-ray, patients were interviewed and examined for signs and symptoms of hemo- and/or pneumothorax, including chest pain or tenderness, tachypnea (greater than 20 breaths per minute), and abnormalities of bilateral lung sounds. Distracting injuries such as fractures or peritonitis were also noted. The authors found auscultation to be 100% sensitive for detection of hemo- and/or pneumothorax following blunt trauma. Chest pain and tenderness and tachypnea were insensitive (57% and 43%, respectively) but had negative predictive values of 99%. In the set of patients with penetrating chest trauma, history and examination were insufficient to exclude hemo- and/or pneumothorax. The authors conclude that stable blunt trauma patients with normal lung sounds and no chest pain, tenderness, or dyspnea do not require chest x-ray to evaluate for hemo- and/or pneumothorax. This study suffers from nonconsecutive enrollment with potential selection bias. Moreover, the rate of hemo- and/or pneumothorax in this population of blunt trauma patients was only 1.3% (7 of 523 patients), so negative predictive values provide a distorted view of the clinical value of history and physical exam. In a population with a higher rate of hemopneumothorax, the same sensitivity and specificity values would result in inadequate negative predictive values. Moreover, this study assessed the sensitivity of examination for hemo- and/or pneumothorax but did not assess for other important thoracic injuries such as mediastinal injury. In patients with a high-energy blunt injury mechanism suggesting possible mediastinal injury, the value of physical examination and history in excluding injury is uncertain. Nonetheless, in patients with a low-energy blunt trauma mechanism from which mediastinal injury is unlikely, a normal thoracic physical exam, and no complaints of chest pain, chest x-ray does not appear routinely necessary. FLOAT NOT FOUND
In children with blunt thoracic trauma ( Box 6-2 ), Holmes et al. performed a prospective study of 986 patients below the age of 16 years to derive a clinical decision rule for detection of pulmonary contusion, hemothorax, pneumothorax, pneumomediastinum, tracheal–bronchial disruption, aortic injury, hemopericardium, pneumopericardium, blunt cardiac injury, rib fracture, sternal fracture, or any injury to the diaphragm. Of their population, 8.1% sustained a thoracic injury. The following
Blunt Trauma
Chest x-ray may not be routinely indicated in stable, alert patients with normal thoracic physical examination and no complaints of chest pain or dyspnea.
Penetrating Trauma
Chest x-ray is routinely required for injuries penetrating the dermis.
Chest X-ray Technique and Limitations
For acute trauma patients, a portable chest x-ray is often the initial imaging test. The portable chest x-ray is performed as a supine or upright anterior–posterior (AP) examination ( Figure 6-1 ). The supine examination
Chest x-ray is not required in the absence of these criteria:
- •
Low age-adjusted systolic blood pressure
- •
Elevated age-adjusted respiratory rate
- •
Abnormal results of thorax exam
- •
Abnormal chest auscultation
- •
Femur fracture
- •
Glasgow Coma Scale score <15










Injuries that can be detected or suggested by chest x-ray ( Table 6-2 ) include bony injuries such as rib fractures, clavicle fractures or dislocations, scapular fractures, and thoracic spinal injury; pneumothorax, hemothorax, possible tracheobronchial injury, pulmonary contusion, and subcutaneous emphysema; mediastinal abnormalities, including cardiomegaly suggesting pericardial effusion, pneumopericardium, and a host of findings suggesting aortic injury; diaphragmatic injuries; pneumoperitoneum; and retained foreign bodies, such as bullet fragments.
| Injury Type | Specific Injury or Finding | Sensitivity |
|---|---|---|
| Bony injuries |
| Varies depending on degree of displacement. |
| Injuries to the lungs, pleura, or airways |
| Varies depending on degree of injury. Controversy exists about the necessity for explicit diagnosis and treatment of subtle injuries not evident on chest x-ray. Chest x-ray has been reported to be only 45% sensitive for pneumothorax compared with CT, but the necessity for treatment of CT-only pneumothoraces is unclear. |
| Mediastinal and cardiac injuries |
| Around 86%-93% sensitive for aortic injury. |
| Diaphragmatic injuries |
| Around 60%. |
| Abdominal injuries |
| Varies with degree of pneumoperitoneum. Sensitivity is reportedly around 38% for any pneumoperitoneum but as low as zero in patients with minimal free air (1-mm air pockets) and as high as 100% in patients with ≥13-mm collections. |
| Foreign bodies |
| Varies depending on size and density of object. |
Recent studies suggest that chest x-ray is relatively insensitive for a variety of clinical injury patterns. However, detecting radiographically occult injuries with more advanced diagnostic modalities such as CT scan may not always result in clinical benefits to patients. For example, when a hemothorax is visible on chest CT but not on chest x-ray, it is uncertain whether thoracostomy tube drainage is routinely necessary.
Interpretation of Chest X-ray for Trauma
Chest x-ray interpretation in the setting of trauma must be performed rapidly and systematically. Using a checklist of critical pathology can help you avoid the pitfall of stopping interpretation after recognition of a single abnormality. We review a few important points about the AP portable chest x-ray technique relevant to interpretation, and then we proceed with systematic interpretation.
The usual technique for acquisition of chest x-ray in blunt trauma is a supine AP portable chest x-ray. This technique allows maintenance of spinal precautions in patients with possible spine trauma, and it is appropriate for unconscious patients who are unable to sit or stand. The AP supine technique has several consequences:
- •
The heart and mediastinum appear enlarged, relative to an erect PA x-ray (see Figure 6-1 ). This results from the shortened distance from x-ray tube to film or digital media (3 feet, compared with 6 feet for a typical PA x-ray), and from the increased distance between the heart (an anterior chest structure) and the detector. The consequence is apparent cardiomegaly and a wide mediastinum in some patients, which may purely be artifacts of the x-ray technique. Unfortunately, these findings can simulate important pathology such as traumatic pericardial effusion or aortic injury. In one study, 38% of blunt trauma patients demonstrated a wide mediastinum on supine x-ray but a normal mediastinum on an upright view. When a high suspicion for mediastinal injury exists, chest x-ray abnormalities should be further evaluated by more definitive imaging, such as ultrasound (for pericardial effusion) or CT (for aortic injury or pericardial fluid). When a low suspicion exists—for example, in the stable, alert, and minimally symptomatic patient—an upright PA x-ray can be performed and is often normal enough to provide reassurance of the absence of injury.
- •
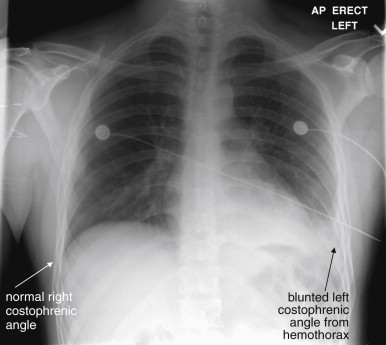
Pleural fluid and air tend to layer in the plane of the x-ray (see Figure 6-2 ). This often makes them less apparent. Blunting of the costophrenic angles by pleural fluid is often absent in a supine x-ray, even with large hemothorax. Even a large hemo- or pneumothorax may be invisible. Sometimes a subtle and diffuse density difference between the right and the left chest indicates an abnormality such as a hemothorax layered horizontally in the plane of the x-ray (see Figures 6-2 through 6-10 ). An upright chest x-ray may reveal layering of pleural fluid (hemothorax) with a more familiar meniscus sign (see Figures 6-6 and 6-7 ). Ultrasound or CT may also reveal findings not recognized on chest x-ray.
- •
The diaphragms are usually higher than in an upright x-ray. This is caused by the weight of abdominal contents pushing against the diaphragm. It results in a lesser degree of lung inflation, with denser-appearing lung parenchyma.
- •
Pneumoperitoneum may not be apparent. Air may not collect in a subdiaphragmatic location in a supine patient; instead, it may collect preferentially at the highest point in the midline abdomen. If free abdominal air is suspected (rare in blunt trauma but common in penetrating trauma), an upright AP or PA x-ray should be obtained whenever possible (see Figure 6-11 ).
In penetrating trauma, an upright chest x-ray is often obtained in stable patients, increasing the sensitivity for pneumoperitoneum and hemothorax. However, the AP portable technique still results in an enlarged cardiac and mediastinal silhouette, as described earlier. With these features in mind, we review a systematic approach to interpretation of the chest radiograph. Many approaches have been described, and any approach that allows rapid but comprehensive assessment is appropriate. Table 6-3 reviews a common mnemonic for interpretation of chest x-ray, which we introduced in Chapter 5 .
| A | Airway
|
| B | Bones and Breast Shadows
|
| C | Cardiac Silhouette
|
| D | Diaphragm
|
| E | Everything Else
|
| F | Lung Fields
|
| F | Foreign Bodies or Devices
|
Pneumothorax and Tension Pneumothorax
A pneumothorax is evident on chest x-ray as an area of increased lucency at the periphery of the lung. The normal lung markings are absent, giving the region of pneumothorax an unusually black appearance compared with the normal appearance ( Figures 6-12 through 6-23 ). Comparison with the contralateral side is useful, although bilateral pneumothoraces may be present. In some cases, the lung edge (visceral pleura) may be visible as a discrete line (see Figures 6-12, 6-13, 6-16, 6-20, and 6-21 ). The average distance from the ipsilateral thoracic cage to the pleural surface (based on three linear measurements) on upright chest x-ray has been described as predicting pneumothorax volume.









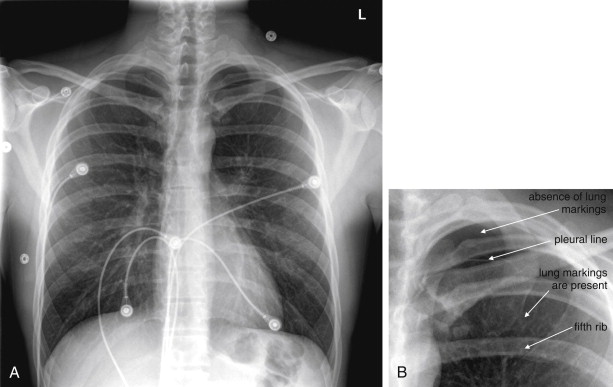


A common pitfall is mistaking the medial border of the scapula for such a pleural line or, conversely, mistaking a pneumothorax for a scapular marking. In cases of very large pneumothorax, the lung may be seen as a density contracted medially toward the lung hilum. Although this is a dramatic and overt finding, to the inexperienced viewer, it may not be recognized without forewarning of this possibility (see Figure 6-13 ).
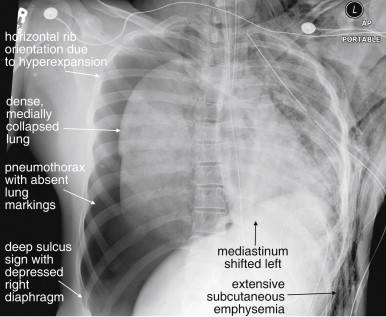
Large pneumothoraces can exert pressure effects, resulting in clinically important hemodynamic compromise. Medical dogma states that a tension pneumothorax should never be recorded on x-ray, as it should be treated empirically as soon as suspected. In reality, some large pneumothoraces are difficult to detect clinically, and some patients remain stable despite radiographic appearances suggesting tension pneumothorax. Classic findings of pressure effects associated with tension pneumothorax include the following ( Figures 6-24 through 6-28 ):
- •
A very lucent hemithorax, nearly black compared with the contralateral side, caused by a large pneumothorax.
- •
A collapsed lung medially contracted toward the hilum.
- •
The “deep sulcus sign,” a particularly deep costophrenic angle, resulting from air under pressure in the pleural space pushing the affected diaphragm inferiorly. In some cases, the sulcus is so deep that the full extent is not visible on the caudad margin of the chest x-ray.
- •
A depressed and flattened hemidiaphragm, again resulting from the effect of pressurized air in the pleural space pushing on the diaphragm. In the case of a right-sided tension pneumothorax, the right hemidiaphragm may appear lower than the left, reversing their normal relationship. (Remember that normally the right diaphragm is higher than the left, because the liver is larger than the spleen.)
- •
Mediastinal shift, in which the heart and other mediastinal structures are pushed toward the opposite side of the thorax by the effect of pressurized air in the pleural space. In addition to the shift of the heart, the trachea and medical devices such as endotracheal tubes and nasogastric tubes may be shifted to the contralateral side. The superior vena cava may appear kinked on chest x-ray. This can restrict venous return of blood to the heart, which, along with high intrathoracic pressure from the tension pneumothorax, impairs cardiac filling and output, leading to hypotension and the physical examination finding of jugular venous distension.
- •
Horizontally oriented ribs on the affected side, caused by hyperinflation of the hemithorax. The normal oblique course of the ribs from posterior to anterior is lost on the frontal chest x-ray projection.




Tracheobronchial Injury
Tracheobronchial injury (see chest x-rays and related CTs, Figures 6-25 through 6-30 ) is a rare but life-threatening injury usually associated with large or tension pneumothorax and requiring surgical intervention. Clues to the presence of this injury include the persistence of a large or even tension pneumothorax despite the apparently appropriate placement of a thoracostomy tube. This finding indicates that the rate of air leaking into the pleural space exceeds the rate at which it is being removed from that space by the thoracostomy tube. Two possibilities explain this scenario:
- •
Malfunction of the thoracostomy tube, which may be misplaced (outside of the pleural space), internally clogged with blood or debris, kinked or compressed within the chest cavity or external to the body, not connected to suction or to a pleural vacuum device, or placed so that one or more of its holes are external to the pleural space, allowing air to enter the thoracostomy tube and pleural space. See the later discussion about evaluation of thoracostomy tubes on chest x-ray.
- •
A rapid rate of air leak into the chest from a tracheobronchial injury or large pulmonary laceration, exceeding the thoracostomy tube capacity. When a large pneumothorax persists despite a large (e.g., 40-French) and properly functioning thoracostomy tube, a tracheobronchial injury is likely. In some cases this can be temporarily addressed by placement of additional thoracostomy tubes to allow faster egress of pleural air, but definitive surgical management will be necessary. In a stable patient, the injury can be confirmed with CT ( Figures 6-29 and 6-30 ). In an unstable patient, immediate surgical intervention is necessary. Intentional selective intubation of the unaffected main bronchus can prevent delivery of additional air into the affected pleural space.

Figure 6-29
Tracheobronchial injury with tension pneumothorax: CT with IV contrast viewed with lung windows.
A, B, Two sequential axial images. Same patient as in Figures 6-28 and 6-30 . This CT is highly suggestive of tracheobronchial injury. A right chest tube has been placed and is clearly seen entering the right pleural space. Despite this, a large tension pneumothorax is still present. The mediastinum remains deviated to the left. The most likely explanation is a large airway injury, which would allow air to enter the pleural space faster than it can be removed by a large-bore chest tube. An alternative explanation would be complete occlusion of the chest tube by kinking or internal plugging. The patient is intubated and receiving positive pressure ventilation, increasing the risk that a bronchial injury would result in tension pneumothorax. Massive subcutaneous emphysema has accumulated bilaterally.

Figure 6-30
Tracheobronchial injury with tension pneumothorax.
CT with IV contrast, lung windows. A, Axial CT image. B, Close-up from A. Same patient as in Figures 6-28 and 6-29 . The actual tracheobronchial injury is seen. The right main bronchus is seen in direct continuity with the large pneumothorax in right pleural space.
A rarer but more specific sign of tracheobronchial injury is the fallen lung sign, in which the collapsed lung falls away from the mediastinum rather than being retracted medially toward the hilum as a consequence of bronchial transection (see Figure 6-30 ).
Tracheobronchial and esophageal injuries are rare following blunt trauma (occurring in only about 1%) but may be suggested by CT. In cases of tracheobronchial injury, chest x-ray may be nondiagnostic in 30%, whereas CT may show a defect in the wall of major airways. Air in the airway may be contiguous with that in the pleural space or mediastinum when viewed with CT lung windows. In cases of esophageal injury, CT may show pneumomediastinum and esophageal thickening at the level of injury (see Figure 6-36 ). A Gastrografin swallow study followed by barium swallow can be diagnostic. Imaging of the esophagus is discussed in more detail in Chapter 4 . If aerodigestive injuries are suspected but the source of the air leak is unclear from diagnostic imaging, bronchoscopy and esophagoscopy can be used to differentiate the source.






Subcutaneous Air
Subcutaneous air, while itself almost never life-threatening, should be carefully sought because it can provide clues to other important injuries including pneumothorax. The appearance is increased lucency (black appearance) in soft tissues resulting from the presence of low-density air. The appearance can be extremely subtle (see Figure 6-22 ) or grossly evident (see Figure 6-28 ), with air outlining muscle fibers and multiple tissue planes. The chest wall, axilla, and neck should be thoroughly inspected. Air within soft tissue can have several sources:
- •
An external wound that has introduced air into soft tissues. Common associated findings would be radiodense foreign bodies. The presence of an external wound and foreign bodies do not rule out the concurrent presence of a pneumothorax as the source of subcutaneous air.
- •
A pneumothorax with leak of air from the pleural space into adjacent soft tissues (see Figures 6-22 and 6-28 ). Common associated findings are rib fractures in either penetrating or blunt trauma or radiodense foreign bodies in the case of penetrating trauma. The associated pneumothorax may not be visible on chest x-ray in all cases.
- •
An esophageal injury with air leak. This is extremely rare in the case of blunt trauma and occurs rarely with penetrating trauma. Radiographic clues to this injury pattern include associated pneumomediastinum.
- •
Valsalva maneuver against a closed glottis during blunt trauma. Again, associated pneumothorax is likely but may be small or invisible on chest x-ray.
- •
Barotrauma from mechanical ventilation. An associated pneumothorax is not always seen on chest x-ray.
- •
Necrotizing infections. These can produce soft-tissue gas but would not be expected in the setting of acute trauma.
Hemothorax
Hemothorax may be subtle (see Figure 6-6 ) or gross (see Figure 6-3 ) on chest x-ray. Technically, chest x-ray reveals the presence of pleural fluid but does not prove it to be blood; a preexisting pleural effusion would have an identical radiographic appearance. The clinical setting is essential to determining the course of action. As described earlier, the commonly used supine portable chest x-ray can compromise detection of hemothorax by causing fluid to layer in the plane of the horizontally positioned x-ray detector. Small amounts of hemothorax may be invisible on supine x-ray; on upright x-ray, these may appear as simple blunting of the costophrenic angles (see Figures 6-2 through 6-10 ). Large hemothoraces may give the entire thorax a denser (whiter) appearance relative to the normal side on supine x-ray, sometimes referred to as a “veiling opacity” (see Figure 6-9 ). On upright AP or PA chest x-ray, these may appear as obvious radiodense layered fluid collections with a curved meniscus where they meet the thoracic wall (see Figure 6-7 ). Other chest x-ray findings commonly associated with hemothorax include pneumothorax, rib fractures, pulmonary contusions, mediastinal injury, and spinal trauma. Large hemothoraces can obscure underlying pulmonary contusions. The diaphragm on the affected side may be obscured, and the possibility of concurrent diaphragmatic injury must be considered. Diaphragm injuries are discussed in more detail later in this chapter and in Chapter 10 . Particularly in the case of penetrating trauma, the subdiaphragmatic area should be assessed for pneumoperitoneum.
Pulmonary Contusion and Laceration
Pulmonary contusion, laceration, and hematoma refer to pulmonary parenchymal injuries that result in hemorrhage into the alveolar space and into interstitial spaces. In blunt trauma, the term contusion is common; in penetrating trauma, the term laceration is more often used, though the chest x-ray appearance is the generally the same. The accumulation of blood, other fluid, and cellular debris increases the density of the normally air-filled alveolar space, making it appear white on chest x-ray (chest x-rays and related CTs, Figures 6-37 through 6-46 ). The interstitial spaces also become more prominent. The affected lung tissue takes on the appearance of a solid organ or fluid. Much confusion exists about the appearance of pulmonary contusion on chest x-ray and the time course over which pulmonary contusion becomes radiographically apparent. Some authors have stated that pulmonary contusion may not be evident for hours, but a more common sense explanation must be understood: If sufficient hemorrhage and injury to lung has occurred to increase the density of the tissue, the injury is immediately apparent on chest x-ray. If a lesser degree of injury is present such that the density of the tissue remains relatively normal, the injury may be invisible initially. If continued hemorrhage or fluid accumulation into the injured tissue occurs, the appearance may become more evident over hours. Pulmonary contusion has no pathognomonic features; the same increased density can occur with pneumonia, aspiration, or pulmonary infarction—all processes that can result in alveolar consolidation. The context of trauma defines the appearance as contusion rather than one of these other processes. It is impossible to distinguish an evolving pulmonary contusion on chest x-ray from a pneumonia developing in the region, because both become visible on chest x-ray by the same process of alveolar and interstitial fluid accumulation. Clinical factors such as the presence of fever are used to make the distinction, which may be impossible even on these grounds. Pulmonary contusion, aspiration, and pneumonia may occur simultaneously. Associated chest x-ray findings can include rib fractures, hemo- or pneumothorax, or radiodense foreign bodies in the setting of penetrating trauma. CT is more sensitive than x-ray and may predict the need for ventilatory support—although it is the clinical state of the patient, not imaging findings, that defines the need for intervention.










Lobar Collapse
Following trauma or as a consequence of endotracheal intubation, lobar collapse with volume loss can occur. Familiarity with the chest x-ray appearance is essential, because this condition can be mistaken for other serious abnormalities, including mediastinal trauma, tension pneumothorax, pulmonary contusion, hemothorax, and diaphragm rupture. Treatment includes maneuvers to reexpand the affected lung segment, sometimes including repositioning of an endotracheal tube or altering ventilator settings. A collapsed lung segment appears dense on chest x-ray ( Figure 6-47 and CT Figure 6-48 ), similar in appearance to other parenchymal abnormalities, such as pulmonary contusion, or to pleural space abnormalities, such as hemothorax. However, because a collapsed lung segment occupies a smaller-than-normal volume, radiographic evidence of volume loss is present. Findings of volume loss include shift of structures toward the area of volume loss. This can include shift of the mediastinum, tracheal deviation, and elevation of the diaphragm on the affected side (see Figure 6-47 ). This is in stark contrast to tension pneumothorax, where structures are shifted away from the affected side. Nevertheless, to an inexperienced observer, the obvious shift of structures may be mistaken for tension pneumothorax. Elevation of the diaphragm can be mistaken for a diaphragmatic injury. If the area of lobar collapse abuts the mediastinum, the mediastinum may appear wide, simulating aortic trauma. In an intubated patient, the position of the endotracheal tube should be noted. Right main bronchus intubation commonly can result in left lung collapse or right upper lobe collapse (because the endotracheal tube may occlude the right upper lobe bronchus). Plugging of bronchi with blood, mucus, or aspirated material can also lead to lobar collapse.


Diaphragm Injury
Injury to the diaphragm is discussed in detail in Chapter 10 . On chest x-ray, the appearance depends on the degree of injury. In cases of overt herniation of intestinal contents into the chest, the appearance can be obvious. In subtle diaphragm tears without herniation of abdominal contents, no radiographic abnormalities may be seen on chest x-ray. Left diaphragmatic injuries are more common than right. In the case of left diaphragm rupture, the stomach (gastric air bubble) and loops of small bowel may be visible within the chest ( Figures 6-49 through 6-55 ). If a nasogastric (NG) or an orogastric (OG) tube is present, it may be visible curled within the thorax (see Figure 6-49 ). Sometimes the appearance suggests only an elevated hemidiaphragm, but diaphragmatic injury must be suspected. When right diaphragm injury is present, the liver may appear to occupy an unusually cephalad position (see Figure 10-33 ). Overall, initial chest x-ray is thought to be only about 17% to 50% sensitive for detection of diaphragm rupture, and positive pressure ventilation is thought to reduce sensitivity, likely resulting from positive pressure pushing the affected diaphragm to a more normal caudad position.







Mediastinal and Aortic Injuries
Life-threatening injury to the aorta and other mediastinal structures can occur with blunt or penetrating trauma. A variety of chest x-ray findings can provide clues to these injuries, as we describe later. Of paramount importance is understanding that an aortic injury may be present with a completely normal chest x-ray, albeit rarely. We discuss some controversies surrounding this rare event later in this chapter. Understanding the mechanisms behind aortic injuries can assist both in recognizing the radiographic appearance and in determining when chest x-ray abnormalities require further imaging. Because of the importance of this injury, we have included numerous example figures to illustrate the range of findings ( Figures 6-56 through 6-108 ).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree