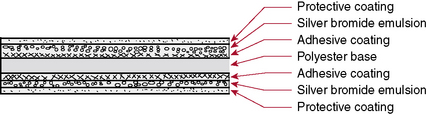
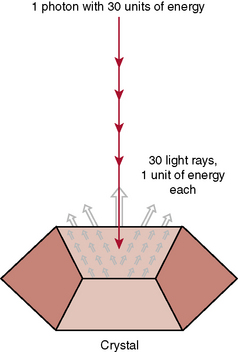
CHAPTER 10 On completion of this chapter, you should be able to: • List factors that affect digital imaging contrast. • List factors that affect film-screen contrast. • List the advantages of digital imaging. • Explain what is meant by image distortion and magnification. • Explain what is meant by detail and visibility of detail. • Compare film-screen imaging with digital imaging in terms of resolution and detail. • Discuss the technologist’s role in image production and evaluation. The diagnostic test begins with the positioning of the patient (Fig. 10-1, A). Next, the technologist determines the appropriate exposure factors to be used to place the image on the image receptor (Fig. 10-1, B). The image receptor may be the conventional film-screen or, most likely, a photosensitive phosphor plate as in computed radiography (CR) or a charged electronic device as in digital radiography, also known as direct digital radiography, (DR). The image receptor in CR is a photostimulable phosphor plate. The latent image is created when x-rays pass through the body part and strike the phosphor, some giving off light; however, some are held within the phosphor particles, creating a latent image. The image receptor in DR is a charged electronic device. The x-ray photons strike a scintillator or a photoconductor. The latent image is in the form of an electrical signal. In any case the image is latent; it is not visible to the human eye and needs to undergo processing to make it visible. Regardless of the image receptor used, the anatomic part to be radiographed will be positioned and evaluated to determine the thickness of the part and the overall tissue density. In addition, when the image is made visible, it must be checked for diagnostic quality (Fig. 10-1, C). The technologist may then consult a technique chart for the proper exposure factors. The exposure factors that affect image quality are discussed later in this chapter. Radiographic film is composed of emulsion spread on a thin transparent sheet of polyester plastic. Except for special uses such as mammography, the emulsion is spread on both sides of the polyester base sheet. The emulsion is the image component of the film and consists of microscopic silver bromide crystals in a gelatin suspension (Fig. 10-2). The film is loaded in the cassette and sandwiched between the two screens (Fig. 10-3). The intensifying screens are made of crystals that will fluoresce when struck by x-rays (Fig. 10-4). The light emitted from the screen crystals will fluoresce when struck by x-rays. The light emitted from the screen crystals exposes the film (Fig. 10-5). Only approximately 5% of the radiographic film density is a result of the x-rays; 95% of the density is a result of light from the screen crystals. FIGURE 10-5 X-ray energy is converted to light energy, thereby intensifying the effect of the x-rays.
Imaging
Conventional and Digital
Conventional and digital imaging
Conception in the Mind of the Physician
Film-Screen Receptor
Radiology Key
Fastest Radiology Insight Engine