While most patients with inflammatory rhinosinusitis are successfully diagnosed clinically, imaging is indicated in patients with recurrent or chronic sinusitis, atypical symptoms and complicated acute sinusitis. Non-enhanced high resolution, thin section computed tomography (CT) is the reference standard in evaluating such patients. It provides superb anatomical details and enables a fairly accurate diagnosis and delineation of the disease, addressing all concerns of the endoscopic surgeon prior to intervention. Contrast MR imaging is preferred for assessing intraorbital or intracranial complications. The radiologist must have a systematic approach to sinonasal CT and generate a clinically relevant report that impacts patient management.
Key points
- •
Noncontrast, multiplanar, high-resolution, thin-section CT is the accepted gold standard for imaging sinonasal inflammatory disease.
- •
MR imaging is preferred to assess intraorbital and intracranial complications, and is not suitable as the first or sole investigation in patients with inflammatory rhinosinusitis.
- •
The nature of sinonasal secretions on CT and MRI and the pattern of bone changes on CT offer important information about the disease.
- •
Patterns of inflammatory rhinosinusitis described at CT have a bearing on the prognosis, choice of treatment options, and therapeutic outcomes for the patients.
- •
A pre-FESS CT report should describe the disease and address all concerns of the endoscopic surgeon, delineating pertinent anatomy, variants and critical relationships.
Introduction
Rhinosinusitis constitutes a fairly large public health problem across the globe. Chronic rhinosinusitis (CRS) affects about 12% to 16% of the US population and is one of the commonest chronic illnesses in America. According to the statistics from the National Institute of Allergy and Infectious diseases (NIAID), about 1 in 8 Indians have this disorder.
Sinusitis, in its simplest definition, means inflammation of the sinus mucosa. It is almost always accompanied by inflammation of the nasal mucosa or rhinitis. Hence, the term rhinosinusitis is used by most otolaryngologists. Sinusitis can be viral, bacterial, allergic, vasomotor, or reactive in nature. Four basic forms are described based on the duration of symptoms:
- 1.
Acute sinusitis: symptoms present for 4 weeks or less
- 2.
Subacute sinusitis: continuation of the acute process and lasts anywhere between 4 and 12 weeks
- 3.
Chronic sinusitis: persistence of the symptoms for 12 weeks or beyond
- 4.
Recurrent acute sinusitis: occurrence of more than 4 episodes of acute sinusitis in 1 year with resolution of symptoms between the episodes
Mucociliary clearance and pathophysiology of sinusitis
The paranasal sinuses are covered by mucous-secreting ciliated columnar epithelium. The cilia move continuously to propel the mucous toward the sinus ostium, the nasal cavity, and finally into the pharynx, constituting mucociliary clearance of the sinonasal cavities. This pattern of mucociliary flow is specific for each sinus and continues even if alternative openings or ostia are created in the sinus. Any disturbance in this mucociliary clearance causes stagnation of secretions, secondary infection, and subsequent sinusitis. Sinus ostial obstruction causing disruption of the mucociliary flow accounts for majority of the cases of recurrent or chronic inflammatory sinusitis. Commonest cause of acute sinusitis is an upper respiratory viral infection. Mucosal congestion causes apposition of the mucosal surfaces of the sinus ostia and drainage pathways, disturbing the mucociliary clearance and predisposing the sinus to secondary bacterial infection. Symptoms may resolve in about a week or may progress to subacute sinusitis. Although most cases may resolve with conservative treatment, about one-third of patients remain refractory to treatment and progress to chronic or recurrent rhinosinusitis.
Indications for imaging
Sinusitis is largely a clinical diagnosis. Imaging is neither recommended nor performed for every patient who presents with sinusitis. The 1997 Task Force on Rhinosinusitis of the American Academy of Otolaryngology – Head and Neck Surgery recommended diagnosing acute rhinosinusitis (ARS) based on major and minor criteria that were further reviewed and simplified in 2007. The American College of Radiology has also laid down appropriateness criteria for imaging in sinonasal inflammatory disease. Table 1 briefly summarizes the indications for imaging in patients with sinusitis.
| Indication | Recommended Imaging Option |
|---|---|
| Acute sinusitis | Generally a clinical diagnosis; imaging adds little valuable information |
| Complicated acute sinusitis | Noncontrast and contrast CT or MR imaging of the paranasal sinuses including orbits and brain |
| Chronic sinusitis a | Noncontrast CT |
| Recurrent sinusitis a | Noncontrast CT |
a Patients with symptoms of recurrent or chronic sinusitis and those who do not respond to medical treatment generally undergo intranasal endoscopy. A CT scan is requested when medical therapy fails or intranasal endoscopy suggests surgically correctable causes.
Imaging options and protocols
With the developments in endoscopic sinus surgery, there has been a parallel supportive evolution in imaging technology and trends with a gradual but definite shift from the use of plain radiography toward CT for evaluating rhinosinusitis. CT has replaced plain radiography because of its greater precision in depicting sinonasal anatomy and pathology. A brief summary on the use of plain radiography, CT, and MR imaging in the evaluation of inflammatory sinonasal disease is provided in Tables 2–4 .
| Feature | Comment |
|---|---|
| Status | Almost obsolete |
| Advantages |
|
| Concerns |
|
| Patient preparation | None Sitting position preferred for depiction of air-fluid levels |
| Protocol |
|
| Feature | Comments |
|---|---|
| Status |
|
| Advantages |
|
| Concerns |
|
| Patient preparation |
|
| Protocol |
|

| Feature | Comment |
|---|---|
| Status | Complementary role in assessment of complicated sinusitis when it is preferred over contrast CT. Not preferred for primary evaluation or as a sole imaging tool for inflammatory sinonasal disease |
| Advantages |
|
| Concerns |
|
| Patient preparation |
|
| Protocol |
|
Imaging appearances
Acute Sinusitis
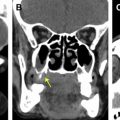
CT and MR imaging features include nonspecific mucosal thickening, submucosal edema, air-fluid levels, or sinus secretions interspersed with air bubbles ( Fig. 2 ). Acute sinonasal secretions are predominantly water and of a mucoid nature (−10 to 25 HU) on CT. They are hypointense on T1 and hyperintense on T2 sequences. An isolated air-fluid level as the only finding in the sinus is fairly characteristic for acute sinusitis, but may not be seen in all patients. The distribution of disease on CT may provide a clue to the cause of the acute disease. Allergic sinusitis is generally more diffuse and bacterial sinusitis is often fairly localized or asymmetric.

Chronic Sinusitis
Imaging features include mucosal thickening, sinus opacification, sclerosis of the bony walls of the sinus, and intrasinus calcifications. Air-fluid levels may be seen superimposed on chronic sinusitis ( Fig. 3 ). Retention cysts, polyps, polyposis, and mucoceles may be seen as sequelae to chronic sinusitis.

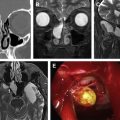
Mucosal thickening
Normal mucosa is generally not seen at CT or MR imaging, and whenever sinus mucosa is seen at the interface between air and bone, that mucosa is presumed to be thickened. Mucosal thickening may be smooth, irregular, or polypoid in morphology. MR is more sensitive to mucosal thickening than CT and depicts the thickened mucosa as a hyperintense signal on T2 images against the black background of sinus air and bone ( Fig. 4 ). In the maxillary sinuses, up to 3 mm mucosal thickening may be seen in healthy individuals and considered normal; any thickening in the frontal and sphenoid sinuses is always considered abnormal and is most likely to be symptomatic. In the ethmoid sinuses, mucosal thickening of up to 2 mm may be attributed to the physiologic phenomenon of the nasal cycle if there is coexistent mucosal swelling of the ipsilateral nasal cavity with prominence of the ipsilateral nasal turbinates ( Fig. 5 ).


Bone changes
The presence of a sclerotic thickened bone is a fairly characteristic feature of chronic sinusitis but may not be seen in all patients. Sclerosis of the bony walls of the sinuses reflects the chronic nature of the disease process ( Fig. 6 ). However, with progressive obstruction and chronicity, there may eventually be gradual pressure erosion and deossification of the marginal bone that is more commonly seen with mucoceles and polyps (see Fig. 19 ).

Secretions and opacification
The density of the secretions at CT and their signal intensity on MR imaging is largely dependent on the proportion of proteins in the secretions. With chronic obstruction, there is a gradual increase in the protein content of the secretions and the thin watery secretions become progressively more viscous and thick. This is seen as a progressive increase in the density of the secretions on CT and the chronic inspissated secretions are hyperdense on CT. A thin hypodense line is usually seen separating the dense sinus secretions from the bony wall and represents the thickened mucosa and submucosal edema ( Fig. 7 ). On MR imaging, various combinations of signal intensities on T1 and T2 images have been described with increasing protein concentration of the secretions (see Fig. 7 ; Figs. 8 and 9 ). These are tabulated in Table 5 . On contrast administration, if the thickened mucosa does not enhance, it is probably not actively infected and is fibrotic and scarred. Active infection has a thin zone of mucosal enhancement with a zone of submucosal edema separating this mucosa from the bony wall ( Fig. 10 ).



| Protein Content | T1 Images | T2 Images |
|---|---|---|
| Up to 5% | Hypointense | Hyperintense |
| 5%–25% | Hyperintense | Hyperintense |
| 25%–30% | Hyperintense | Hypointense (see Figs. 7 and 8 ) |
| 30%–35% a | Hypointense | Hypointense |
| >35% a | Signal void | Signal void (see Fig. 9 ) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree