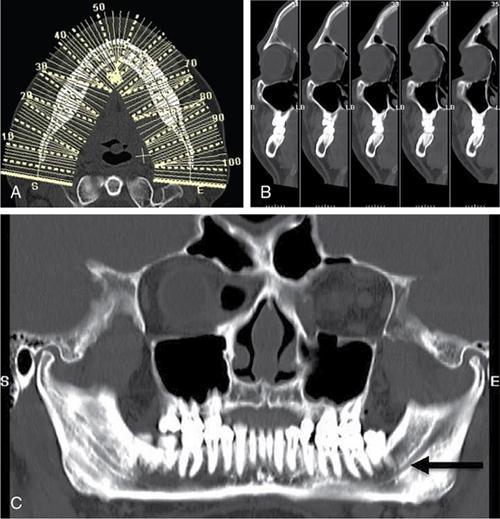
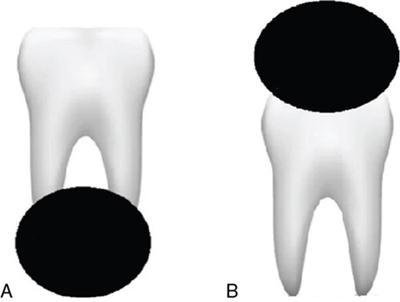
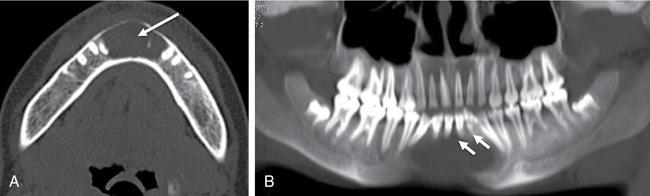
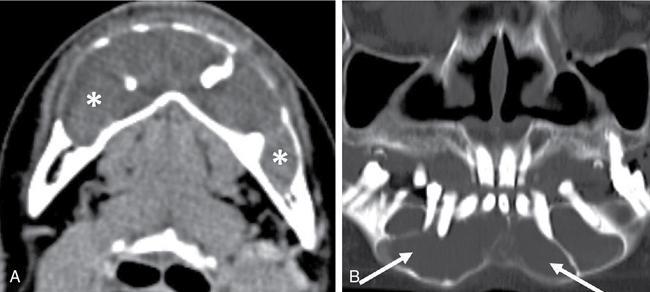
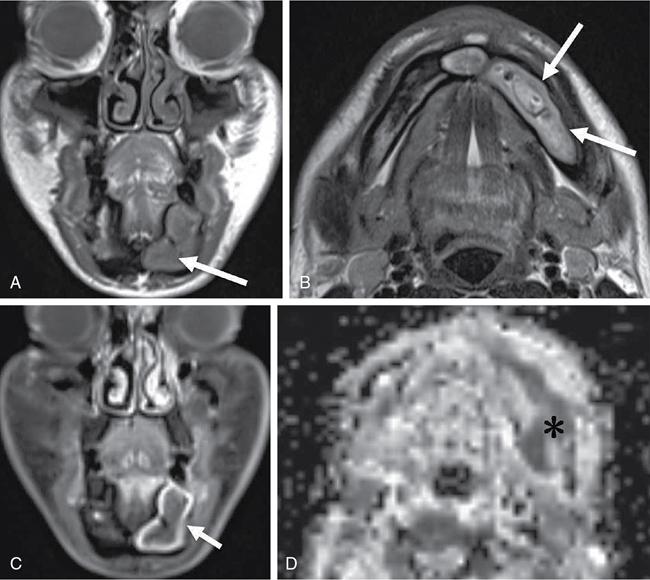
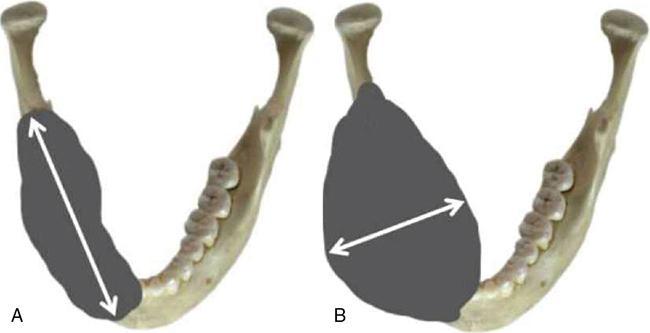
Jyoti Kumar, M. Sarthak Swarup A wide variety of benign and malignant lesions may involve the jaws, which can develop from both odontogenic and nonodontogenic tissues. Odontogenic lesions can arise from the tooth-forming epithelium, mesenchymal tissue or both. Nonodontogenic lesions are similar to other bony lesions seen elsewhere in the body. Imaging plays an important role in the diagnosis and management of these lesions. An attempt to differentiate odontogenic from nonodontogenic lesions may be made on imaging. This differentiation can be difficult in a large lesion. Besides this, imaging features such as cystic or solid appearance of lesions, their margins, internal contents and effects on adjacent teeth and inferior alveolar canal are essential in further narrowing the differential diagnosis. In addition to imaging appearance, age and gender of the patient and location within the maxilla and mandible are also important considerations in making the diagnosis. Despite this information, however, many lesions are impossible to differentiate without biopsy. In such cases, defining the degree of malignant potential or aggressiveness is very helpful to the treating surgeon. This topic will briefly describe the imaging features of common maxillomandibular lesions and provide a helpful approach for their diagnosis and differentiation. Radiography remains the initial modality of choice. This technique is highly effective in detecting abnormal maxillomandibular lesions and delineating their relationship with teeth. They provide better spatial resolution as compared with other imaging modalities and especially useful in lesions smaller than 2 cm. They accurately evaluate the vertical relationship between the lesion and tooth apex. Presence of a thin sclerotic rim, subtle cortical erosion and the nature of certain high-density substance within the lesion can be detected well by intraoral radiographs. However, it cannot be used for lesions larger than 3 cm, because of the small film size. They are used to examine larger lesions and have a broad coverage including teeth, maxillary and mandibular dental arches and facial bones (Fig. 3.22.1). Extraoral radiography has lower doses of radiation exposure than intraoral radiography, and it can be used in patients who are unable to open their mouths. However, panoramic radiographs have limited spatial resolution and may be limited by superimpositions, ghost images and technical artefacts. One important disadvantage of radiography is that it cannot evaluate the cortical bone along lingual and buccal surfaces of the mandible or determine the precise medial and lateral relationship of the mandibular canal to jaw lesions. These pitfalls can be overcome by additional imaging, including multidetector row CT (MDCT), cone-beam computed tomography (CBCT) and MRI, with delineation of the extent of the lesions in all three planes. CT images in bone window setting are highly useful for demonstrating the extent of bone resorption, osteosclerosis, cortical bone swelling/expansion, destruction and calcification. The lesions should also be evaluated on soft-tissue window settings, especially after contrast administration. These are particularly useful in delineation and characterization of jaw infections and tumours. In addition to multiplanar reconstructions (MPRs), the isotropic data set can be used for 3D processing and advanced dental reformations, which help to obtain multiple cross-sectional paraxial and panoramic images (Fig. 3.22.2). Paraaxial images are useful in preoperative planning and measurement of implants. The panoramic reconstructions simulate panoramic radiography and are immensely useful in the global evaluation of maxillofacial tumours and cysts with precise delineation of the relationship of the lesion to roots of the teeth, mandibular canal and maxillary antrum. This is a special CT technology that uses a cone-shaped X-ray beam and produces high-resolution images of bone and dental structures with a relatively lower radiation dose. However, soft-tissue evaluation and contrast-enhanced studies are not possible with this technique. This technique is discussed in the chapter on dental radiology. MRI is a complementary tool that helps better characterization of soft-tissue components of the lesion, enhancement pattern, wall thickness and nodularity as well as evaluation of extraosseous soft tissue infiltration, and detecting bone marrow changes of the jaw. As contrast enhancement is better picked up on MR, it is a more sensitive modality to differentiate cysts from tumours. Diffusion-weighted (DW) MR imaging is another technique that has shown promising results in differentiating odontogenic keratocyst from cystic tumours. The radiographic features in conjunction with advanced imaging can help the clinician in the differential diagnosis and planning management of the lesion. This is discussed in the chapter on dental radiology. Cancellous bone fills the medullary space within the cortical plates in both jaws. Thin radiopaque plates and bony spicules (trabeculae) create many small radiolucent pockets of marrow within the jaw. The mandibular canal, also known as the inferior alveolar canal, is located within the mandible and contains the inferior alveolar nerve, artery and vein. It starts at the mandibular foramen, on the lingual aspect of the ramus, runs through the mandible and ends at the mental foramen on the anterior aspect of the mandible, adjacent to the second mandibular premolar tooth. The diameter of the mandibular canal usually varies between 2 and 2.4 mm. Radiologic identification of the mandibular canal is important, as odontogenic lesions tend to originate superior to this. Neural and vascular lesions often originate within the mandibular canal, whereas lesions of nonodontogenic origin usually have their epicenter inferior to the canal. A wide range of pathology affects the maxillomandibular region. The latest fourth edition of WHO classification of odontogenic cysts, tumours and allied lesions published in 2017 has been depicted in Table 3.22.1. They may have similar imaging appearance, and differentiating one lesion from another sometimes becomes difficult. In this chapter, the lesions are primarily classified based on their radiographic density into three types. Odontogenic versus nonodontogenic origin, margins, solid/cystic nature are other criteria used to classify them further. The common lesions are enumerated in Tables 3.22.2 and 3.22.3. Each of these lesions is then described in detail highlighting the key imaging features. Jaw lesions are broadly classified as odontogenic and nonodontogenic depending on whether or not they originate from tissues involved in normal tooth development. Lesions with odontogenic origin typically occur in relation to a single tooth or a part of the tooth. For example, radicular cysts develop around the tooth apex, while dentigerous cysts surround the tooth crown (Fig. 3.22.3). Nonodontogenic lesions usually have either no specific relationship with teeth or involve a large part of the bone close to two or more teeth. While odontogenic lesions usually are seen above the level of the alveolar canal, lesions involving the canal or below the level of the canal are usually nonodontogenic in origin. Unilocular or multilocular, well-defined, radiolucent lesions have the highest incidence among jawbone lesions. They may be cystic or solid lesions. The radiographic features of cysts are, in general, similar to each other, appearing as lytic round or oval-shaped lesions, with well-defined corticated margins. The radicular cyst is the most common type of odontogenic cyst. It is usually seen in the 30–50 years age group with a slightly male predominance. It is found at the apex of a nonvital tooth resulting from inflammation of the periapical tissues secondary to caries or trauma. Most cysts (60%) are found in the maxilla, especially around incisors and canines. The extension of the infection from the pulp cavity to the tooth apex initially results in periapical periodontitis, which may develop into either an acute abscess or a chronic granuloma and ultimately lead to the formation of a radicular cyst. It appears as a rounded or pear-shaped unilocular radiolucent lesion in the periapical region with well-circumscribed and corticated margins (Fig. 3.22.4). Usually, it is small in size; occasionally, it becomes large enough to cause cortical expansion, displacement of adjacent structures including adjacent teeth and mandibular canal and sometimes mild root resorption. CBCT images may be superior compared with periapical radiographs in detecting a periapical lesion. CT better demonstrates the extent of the cyst and adjacent tooth involvement. Treatment options include endodontic treatment with cyst wall enucleation and sometimes tooth extraction. An important point to consider is that radicular cysts and periapical granulomas have a similar radiographic appearance and can be difficult to differentiate. Features that favour the diagnosis of radicular cysts are relatively large size (>200 mm3) and more well-defined borders. Inflammatory collateral cyst is an uncommon cystic lesion typically seen in children and primarily affects the mandibular permanent molar teeth during their eruption. It is categorized into paradental cysts and buccal bifurcation cysts. These are described in detail in the chapter on dental radiology. Residual cyst is essentially a radicular cyst that persists in the jaw after the surgical extraction of a nonvital tooth. It is fairly common and has similar radiological features as radicular cyst; however, the top of the cyst typically reaches alveolar crest with a corresponding missing tooth. Dentigerous cyst is the most common developmental odontogenic cyst and second most common odontogenic cyst overall. It is usually seen in adults in the third to fourth decades of life. The cyst forms in the pericoronal location around the crown of an unerupted tooth, commonly the maxillary and mandibular third molar. Other typical locations are along the maxillary canine and mandibular second premolar tooth. The cyst is caused by the proliferation of the enamel epithelium surrounding the crown and accumulation of fluid between the layers with its expansion. On radiographs, it is seen as a well-defined, expansile, unilocular lucent lesion, associated with an unerupted or impacted tooth. The pathognomonic imaging appearance is that the cyst attaches to the cementoenamel junction of the involved tooth with the crown projecting into the cystic cavity (Fig. 3.22.5). Dentigerous cyst can vary in size but has the potential to grow large and cause significant expansion of the jaw and considerable displacement of adjacent teeth with resorption of the roots. There is no associated periosteal reaction or soft tissue, and the cortical bone is usually preserved. CT is useful to evaluate large lesions and can show the origin, size and internal contents of the cyst and evaluate the expansion and integrity of the cortical plate and its relationship to adjacent anatomic structures. MRI is not required for diagnosis in most cases; however, it may aid in the characterization of large lesions. MRI typically shows homogeneous high T2 and low to intermediate T1 signal within the cyst, with thin rim enhancement on postcontrast images. Large lesion may mimic ameloblastomas and odontogenic keratocysts (OKCs) due to uneven expansion and development of undulating borders. Rarely, ameloblastoma can develop within the lining of a long-standing untreated cyst. Postcontrast CT/MRI can aid in differentiation by depicting solid enhancing component and thick irregular wall in an ameloblastoma. OKC may be uni- or multilocular and characteristically shows expansion along the anteroposterior axis with minimal expansion along the buccolingual axis. If associated with an unerupted tooth, it can envelop the entire tooth when large including the roots, unlike dentigerous cyst that usually envelopes only the crown. There have been ongoing controversies regarding the pathogenesis and biologic behaviour of odontogenic keratocyst. This was classified as a neoplasm and named as keratocystic odontogenetic tumour (KCOT) in the third edition of WHO classification owing to its aggressive growth pattern, recurrence after treatment and presumed overlapping molecular phenotyping with jaw tumours. It has now been categorized in the cystic lesions in the latest fourth edition of WHO classification of 2017 with changing of nomenclature back to OKC due to insufficient evidence to support the neoplastic nature of this lesion. It is typically found in adults in the second to fourth decades of life with a male predilection. OKC is most commonly located in the posterior mandible in relation to the third molar tooth and involves mandibular ramus and body, often in association with an impacted tooth. It develops from the dental lamina, which is found throughout the jaw and overlying alveolar mucosa and is lined by stratified keratinizing squamous epithelium. Multiple OKCs in a younger age group raise the possibility of basal cell nevus syndrome (Gorlin–Goltz syndrome) (Fig. 3.22.6) characterized by multiple basal cell carcinomas, odontogenic keratocysts, spinal and rib anomalies, midface hypoplasia and calcification of the falx cerebri. Due to its potentially aggressive and infiltrative behaviour, it has a high recurrence rate after resection. However, malignant transformation is rare. Radiographically, it presents as a well-circumscribed, radiolucent lesion with well-corticated or scalloped borders. Smaller lesion tends to be unilocular, whereas larger lesion tends to be multilocular, often with daughter cysts that extend to the surrounding bone. OKC has a tendency to grow in a predominantly anteroposterior direction while causing minimal buccolingual cortical expansion. If associated with an unerupted tooth, it can envelop the entire tooth when large including the root. The contents of the cyst cavity can be evaluated by CT or MRI. OKC has a specific paste-like keratinaceous material, which can result in heterogeneously increased attenuation on CT (40–50 HU) (Fig. 3.22.7). MRI shows intermediate to high signal intensity on T1-weighted MR image and heterogeneous signal on T2-weighted MR image due to variable protein content of cyst (Fig. 3.22.8). Postcontrast MR images reveal minimally enhancing, uniformly thin and regular cyst wall. Diffusion restriction of the proteinaceous contents of the cyst is a feature characteristically seen in OKC. It can mimic a dentigerous cyst if it occurs in a pericoronal location and associated with an impacted tooth. However, unlike dentigerous cyst, OKC when large envelopes the entire tooth and not just the crown. Although the potential for bone expansion and tooth displacement can be found in both entities, the cortex is usually preserved in dentigerous cysts, unlike OKC, which can lead to cortical erosion. A multilocular OKC may resemble an ameloblastoma on imaging. However, the predominant growth pattern of OKC along the length of the mandible with mild buccolingual expansion helps differentiate it from an ameloblastoma (Fig. 3.22.9). Moreover, resorption of the roots of adjacent teeth and displacement of adjacent structures is less frequent and less severe in OKC compared with ameloblastoma. Postcontrast MRI also facilitates the differentiation of OKC from ameloblastoma, which has a mixed pattern of solid and cystic components, irregular thick walls and avid enhancement of solid components. Diffusion-weighted MRI acts as an important adjunct in distinguishing OKC from ameloblastoma owing to the restricted diffusion and low ADC values seen in the viscous cyst fluid of the former, while it is only the solid component of ameloblastoma that shows restricted diffusivity. An ADC value of 2.137 × 10−3 mm2/s has been proven to be a useful cut-off to differentiate between the predominantly cystic ameloblastomas and OKC.
3.22: Imaging jaw lesions
Introduction
Imaging modalities
Radiography
a. Intraoral radiographs
b. Extraoral panoramic radiographs/orthopantomograms

Computed tomography
a. MDCT
b. CBCT
Magnetic resonance imaging
Relevant imaging anatomy
Tooth structure
Jaw bones
Pathologic conditions
WELL-DEFINED MARGINS
Cystic
Odontogenic
Nonodontogenic
Solid
Odontogenic
Non-odontogenic
ILL-DEFINED MARGINS
Odontogenic
Nonodontogenic
RADIOPAQUE LESIONS
Odontogenic
Nonodontogenic
MIXED-DENSITY LESIONS
Odontogenic
Nonodontogenic
Odontogenic versus nonodontogenic lesions
Well-defined radiolucent jaw lesions
Odontogenic cystic lesions
Radicular cyst
Differential diagnosis.
Imaging pearls
Inflammatory collateral cyst
Residual cyst
Imaging pearls
Dentigerous (follicular) cyst

Differential diagnosis.
Imaging pearls
Odontogenic keratocyst

Differential diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








