To image or not to image?
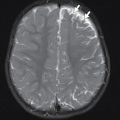
Quality in health care, as defined by the U.S. Agency for Healthcare Research and Quality, is “doing the right thing for the right patient, at the right time, in the right way to achieve the best possible results.” When a pediatric patient presents in the emergency setting, the decision of which, if any, imaging test should be performed can be challenging. Factors to consider include patient factors, such as age, developmental stage, and coexisting illness, and facility factors, including available expertise in pediatric imaging, clinical support such as pediatric surgical services, and whether sedation capabilities are available if needed. One must consider whether the imaging test answers the clinical question, as well as myriad other questions: Can the child cooperate for the study? Can intravenous (IV) access be obtained if necessary? Is a test necessary or can the diagnosis be made clinically, either at presentation or after an observation period? Can testing be delayed until other resources are available (e.g., the only pediatric sonographer arrives at 7:00 a.m.)? Do the benefits of the test results outweigh potential risks? One must consider whether an imaging strategy follows the “ALARA” principle: keeping patient exposure to ionizing radiation “as low as reasonably achievable” (see Chapter 2 ) while ensuring diagnostic quality of the imaging. If considering a test involving ionizing radiation, is there an alternative mode of making the diagnosis with less risk (e.g., rapid magnetic resonance imaging [MRI] for hydrocephalus in a patient with a ventricular shunt)? There may be a role for shared decision making, educating the patient or the parent/guardian, and involving them in the decision. The clinician should also consider whether the patient is best served by imaging at the current facility or whether the patient should be transferred to a more specialized facility for diagnosis and management.
Transition to evidence-based medicine
Traditionally, medical decision making has been based on an individual practitioner’s experience and what the practitioner had learned from what has been termed “eminence-based medicine”; however, more recently, there has been a transition to evidence-based medicine, with a major goal of improving outcomes for patients. “Eminence-based medicine” has been described as reliance on learning from experts, especially those encountered through medical training, national publications, and meetings, and this approach relies on years of practice experience. In evidence-based medicine, it is assumed that a single practitioner does not arrive at an unbiased assessment through experience alone. In this paradigm, assessment of appropriate medical care should be based upon evidence-based research. The practitioner does not just accept information from the expert but assimilates and critically assesses the research evidence in literature to guide a clinical decision. In this process, one formulates a clinical question, identifies pertinent medical literature, judges the quality of studies, produces a summary of evidence, and applies evidence to arrive at appropriate clinical action. For an individual clinician, with the volume of medical literature and the pace of imaging innovation, this task can become overwhelming, especially for one practicing in an emergency center environment, caring for patients with a wide variety of illnesses and injuries. A need for evidence-based imaging guidelines and support has developed.
Evidence-based imaging for the emergency patient
With increased availability and complexity of imaging technologies, the use of medical imaging can significantly increase without resulting in clinical gains and benefits for patients. A goal for evidence-based imaging is to ensure that patients receive quality care and the benefits of imaging, while minimizing risk. In 2015, the Society for Academic Emergency Medicine convened a multidisciplinary conference “Diagnostic Imaging in the Emergency Department: A Research Agenda to Optimize Utilization.” , Citing the increased use of diagnostic imaging in the emergency setting, the goals of this conference were to establish a priority research agenda for emergency diagnostic imaging, in order to guide the design of future investigations, and to develop evidence-based knowledge to improve quality, safety, and outcomes for patients. One of the priority topics was clinical decision rules (CDRs). CDRs are evidence-based algorithms derived from research and used to provide guidance for clinical decision making. CDRs can potentially reduce the use of diagnostic tests, reduce inappropriate variation in practice, and empower the clinician with risk assessments for a given set of clinical symptoms and signs.
Clinical decision support (CDS)
CDRs are a form of CDS (CDS, or CDSM for clinical decision support mechanism). Appropriate use criteria (AUC, or AC for appropriateness criteria®), such as those established by the American College of Radiology (ACR), are also a component of CDS. CDS, including AUC, such as the Pediatric Emergency Care Applied Research Network (PECARN) head injury rule and the Canadian Assessment of Tomography for Childhood Head Injury (CATCH) rule, enables provider education and provides evidence-based guidance for imaging.
A widely utilized CDR, the PECARN head injury rule, was developed using a large, multicenter prospective cohort to identify children at very low risk of clinically important traumatic brain injury (TBI) who could safely avoid computed tomography (CT). TBI prediction rules assist with decision making by identifying patients at either low risk for TBI, for whom CT scans may be safely avoided, or at high risk for TBI, for whom CT scans may be indicated. PECARN head injury prediction rules have been externally validated, shown to be reliable in clinical practice, with both excellent sensitivity and negative predictive value for clinically important TBI. , Prediction rules are best applied together with clinical judgment, based on factors including practice setting and clinician experience.
With the increased availability and complexity of advanced diagnostic imaging, it is important to realize that increased utilization of an imaging technology can decrease diagnostic yield and create harm due to unnecessary imaging. CDS can provide evidence-based guidance to diminish this effect. In a recent study, providers were given a choice of whether to use a CDS tool in the decision to order a CT scan for pulmonary embolus (PE). The percentage of positive tests for PE increased (38% higher diagnostic yield) when providers chose to use CDS, as compared to when providers chose not to use the CDS tool.
CDSMs can be integrated into clinical pathways and electronic health information systems, to be readily available to the clinician at the time of order entry. The ACR AC are a helpful resource for imaging evaluation guidance and are available, along with other evidence-based AUC guidelines, in the CareSelect Imaging product (National Decision Support Company, Madison, Wisconsin). The ACR AC are also available for free online at https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria® . In the United States, CDS vendors are required to provide a free online version of their product.
Although CDS tools are of value, individual practitioner experience and judgment remain important, as does the value of the radiologist consultation. As part of a study about how software-based CDSMs may integrate with current imaging CDS, pediatric emergency department physicians were interviewed. The emergency physicians emphasized that although they were optimistic that the newly provided CDSM may improve workflow, they stated that CDSMs are not a “fix-all”: radiologist consultation remained a valuable component of imaging CDS, and they sought out guidance through discussion with the radiologist, especially when a clinical scenario did not fit well within existing clinical pathways. The clinicians asserted that consultation with a radiologist allows discussion of the nuances of a clinical situation, allowing helpful discussion of the risks and benefits, potential harm, or patient factors.
ACR appropriateness criteria®
CDS tools have been effectively integrated in the management of pediatric head trauma, and the ACR AC for head injury in children depend upon the clinical PECARN head injury rule. The ACR AC for mild blunt head injury in a child with intermediate risk for clinically important brain injury by PECARN criteria ( Table 1.1 ) indicate that a head CT without IV contrast may be appropriate for initial imaging, but the other listed imaging tests are usually not appropriate. The relative radiation doses of the imaging tests are also given in a graphic manner in this ratings table.
To use the online ACR AC for CDS, from the main page ( Box 1.1 ), choose “Browse Topic” (or create a Login and choose “Search Topics”). After choosing “Browse Topic,” choose “Pediatric” ( Box 1.2 ), select “Search” and scroll to “Head Trauma–Child.” Choosing the “Narrative and Rating Table” will open a document containing the multiple clinical variants, showing the imaging rating chart for each variant, as seen in Table 1.1 . This document also includes a background narrative about that specific AC, including a summary of the literature review, imaging considerations by modality, a discussion of each imaging modality by clinical variant, a summary of recommendations, and a reference list. Other documents that can be chosen include an Evidence Table (summarizes the literature, rates the quality of studies, gives study results) and a Literature Search (shows what searches were performed, including dates, search strategies, and a summary of the literature review), and many AC include a link to a brief patient-friendly summary of the AC.