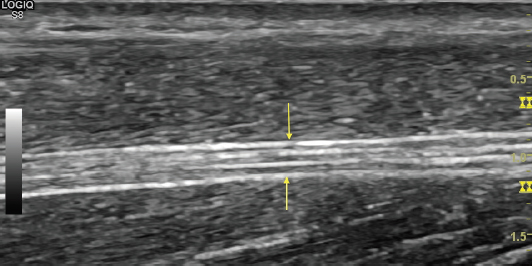
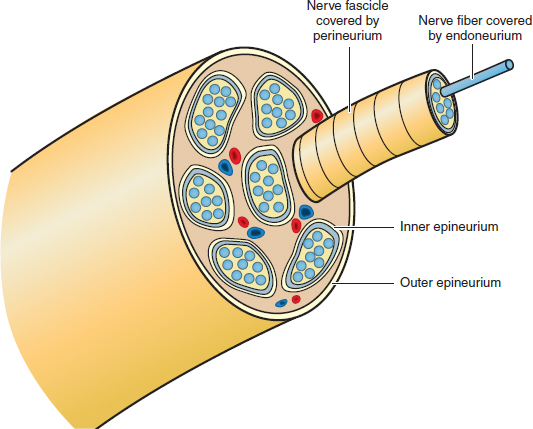
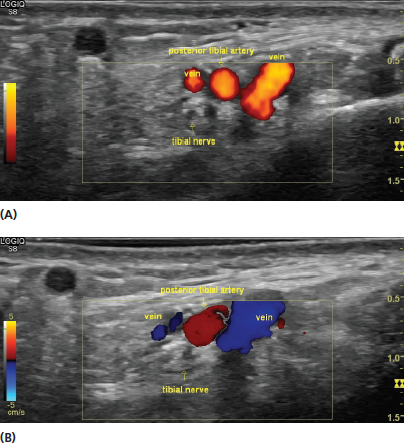
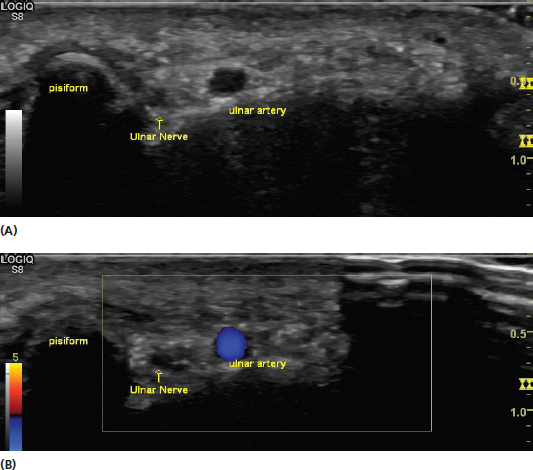
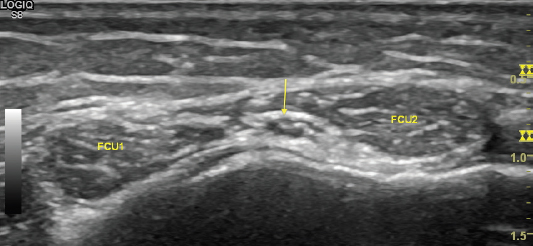
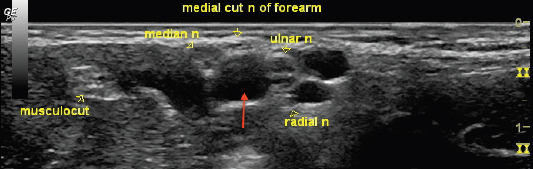
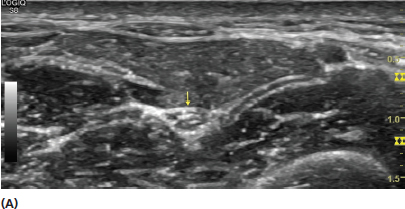
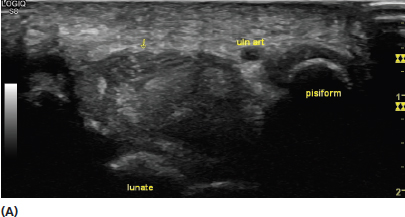
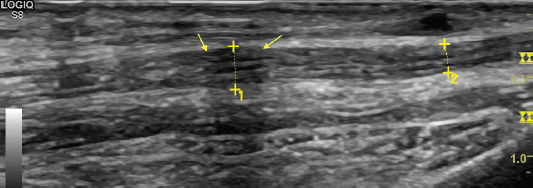
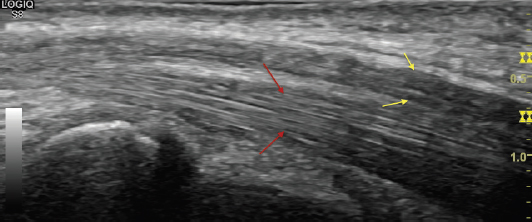
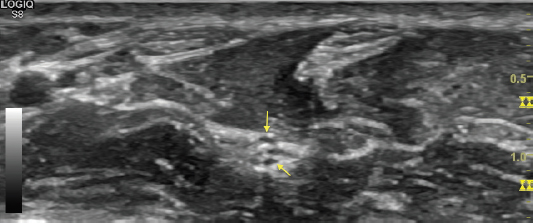
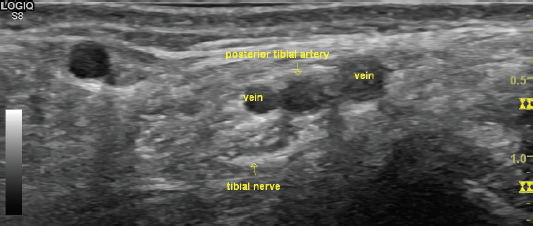
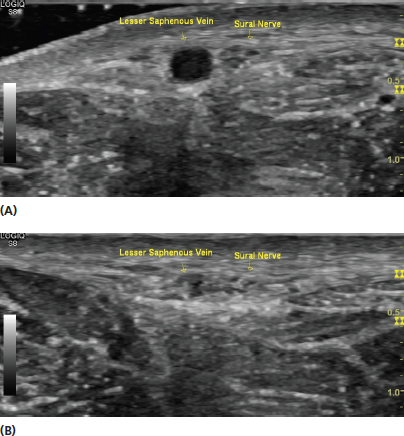
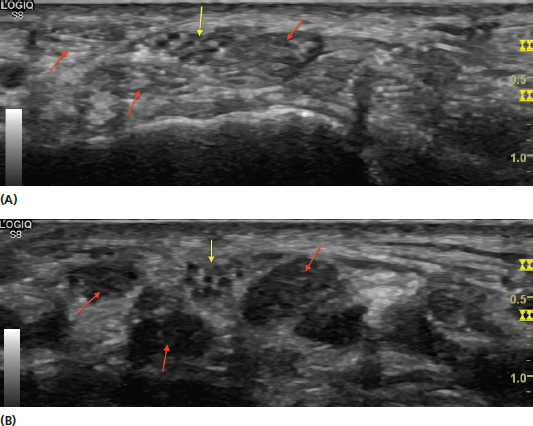
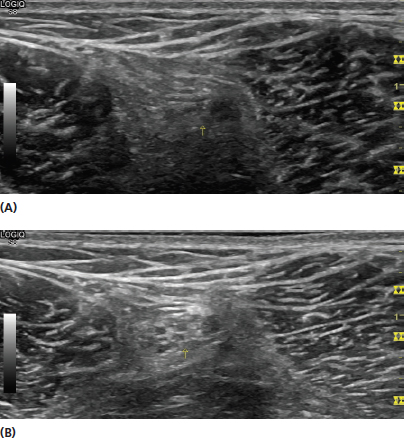
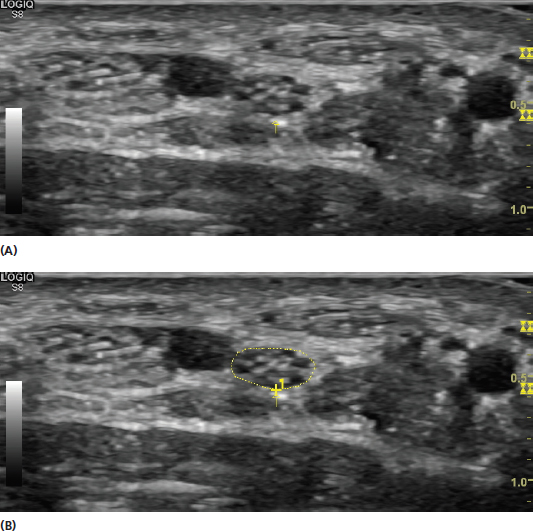
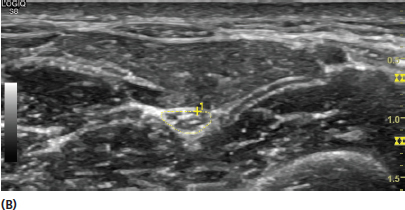
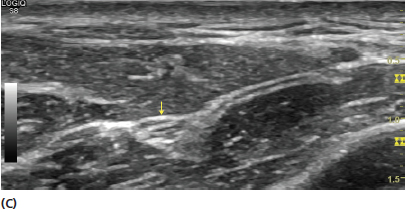
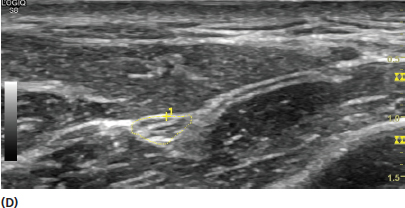
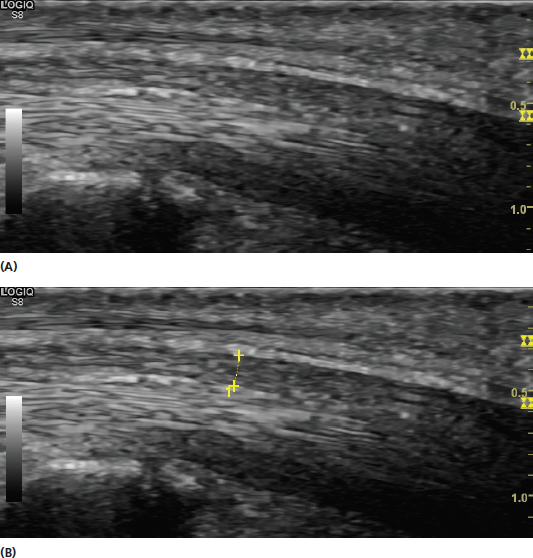
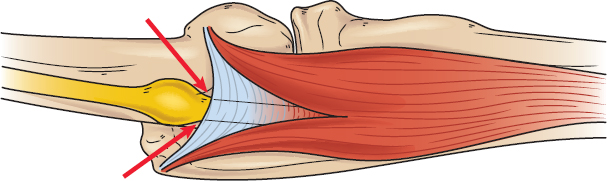
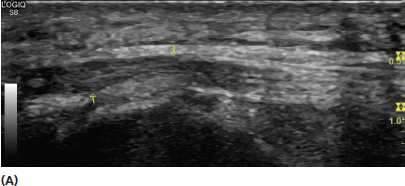
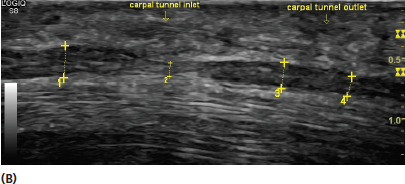
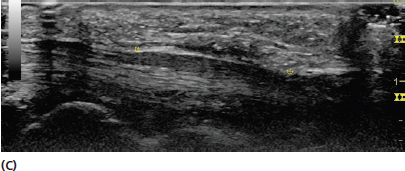
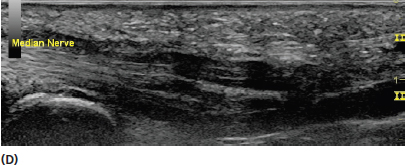
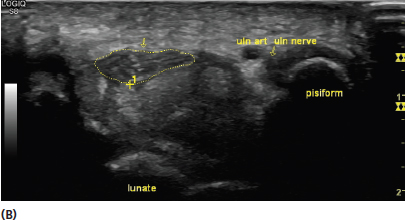
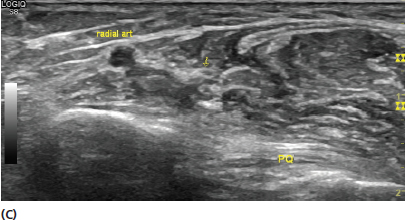
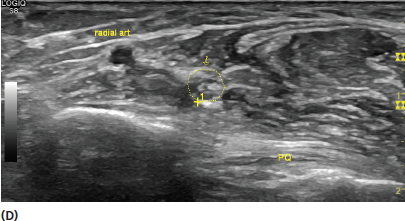
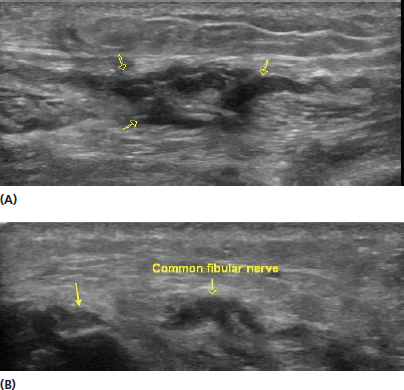
Ultrasound is an excellent modality for evaluation of peripheral nerve tissue. The high resolution and dynamic capabilities allow precise measurements of even subtle changes, detection of alteration of the internal structure, and dynamic effect of surrounding tissue. Developing skills for imaging peripheral nerves can be used for proper tissue recognition in musculoskeletal evaluations, diagnostic assessment of both focal and generalized neuropathies, and in identification for nerve blocks. The appearance of nerve on ultrasound is that of an uninterrupted fascicular pattern (Figure 9.1). This differs from the intercalated pattern typical of tendons (Figure 9.2). The hypoechoic (dark) nerve fascicles are seen among the hyperechoic (bright) epineurium. In short-axis view, this creates an appearance that is frequently described as resembling a “honeycomb” (Figure 9.3). Histologically, the fascicles are enveloped by perineurium and the nerve fibers are covered by endoneurium (Figure 9.4). The outer sheath is termed the epineurium or “outer epineurium” and the tissue between the fascicles and the outer epineurium is sometimes referred to as the “inner epineurium.” Nerves often have arteries and veins that accompany them and it is necessary to recognize them for reliable identification (Figure 9.5). Doppler imaging can be used to attempt to see flow in suspected vessels (Figure 9.6). Veins can be identified by their compressibility (Figure 9.7). Nerves generally have intraneural vessels; however, these are usually not readily identifiable on ultrasound. It is important to reliably identify the larger vascular structures so that they are distinguished from the nerve when performing measurements. Often, scanning proximally and distally can improve this determination. Use of Doppler is also helpful when needed (Figure 9.8). FIGURE 9.1 Sonogram demonstrating a long-axis view of the uninterrupted fascicular pattern of normal nerve (yellow arrows). FIGURE 9.2 Sonogram demonstrating a long-axis view of the fine intercalated fibrillar pattern of a tendon (red arrows) in contrast to the fascicular pattern of a nerve (yellow arrows). FIGURE 9.3 Sonogram demonstrating a nerve (yellow arrows) in short-axis view. Note the hypoechoic (dark) round fascicles surrounded by the hyperechoic epineurium. FIGURE 9.4 Illustration of the components of a peripheral nerve, demonstrating the nerve fiber covered by the endoneurium, the nerve fascicle covered by the perineurium, and the groups of fascicles covered by the epineurium. FIGURE 9.5 Sonogram demonstrating a short-axis view of the tibial nerve at the level of the ankle. The accompanying posterior tibial artery and veins can be used to help identify the nerve. FIGURE 9.6 Sonograms demonstrating the use of power (A) and color (B) Doppler to identify the tibial artery and veins. Flow is created through the veins by changing the amount of pressure from the transducer. FIGURE 9.7 Sonograms demonstrating a short-axis view of the sural nerve. The hypoechoic (dark) lesser saphenous vein is used as a landmark to identify the nerve. Note that the vein is highly visible with less transducer pressure (A) but is compressed and less conspicuous with more transducer pressure (B). FIGURE 9.8 Sonograms of a short-axis view of the ulnar nerve at the ulnar tunnel. The gray scale image (A) shows the nerve and artery both appear hypoechoic (dark) relative to the surrounding tissue. The use of Doppler (B) helps distinguish the ulnar artery from the nerve. Nerves are generally easier to identify in short-axis view. Efforts should be made to identify the fascicular architecture and distinguish it from the surrounding tissue (Figure 9.9). Scanning back and forth can help distinguish the nerve tissue from other surrounding tissue. Other techniques used to improve the conspicuity of the nerve include movement of the surrounding tissue, rocking or toggling the transducer, or moving to a position where there is more contrast from the surrounding tissue relative to the nerve (Figure 9.10). Using conspicuous anatomic landmarks can help identify the location of more challenging nerves (Figure 9.11). When following the course of a nerve in short axis, it is often more effective to scan rapidly rather than too slowly to accentuate the contrast in tissue. Using liberal amounts of coupling gel is helpful to facilitate that. FIGURE 9.9 Sonogram demonstrating a short-axis view of the ulnar nerve in the cubital tunnel. The nerve tissue is distinguished from the surrounding muscle tissue, in this case the two heads of the flexor carpi ulnaris (FCU1, FCU2). Following the nerve back and forth in short axis can help increase conspicuity by accentuating the contrast relative to other tissue. FIGURE 9.10 Sonograms demonstrating the use of anisotropy to help distinguish nerve tissue from tendon. The images demonstrate a short-axis view of the median nerve (yellow arrows) and surrounding flexor tendons (red arrows) in the carpal tunnel. Image (A) demonstrates the appearance with the transducer orthogonal to the nerve and tendons. In image (B), the transducer is toggled, decreasing the anisotropic artifact of the tissue. Note that the anisotropic artifact is considerably greater with the tendons resulting in a more dramatic change in echotexture. This illustrates how toggling the transducer can increase the conspicuity of the nerve. FIGURE 9.11 Sonogram demonstrating an example of identifying more challenging nerves based on another anatomic landmark. The different peripheral nerves are identified based on their position in relation to the axillary artery (red arrow). The examiner should be vigilant about the amount of pressure that is being placed on the tissue by the transducer. Excessive pressure can alter the shape of the underlying nerve as well as compress the surrounding tissue. This includes surrounding vascular structures such as veins that can often help with localization (Figure 9.7). In some circumstances, the use of higher transducer pressure can improve the image quality of a relatively deep nerve (Figure 9.12). FIGURE 9.12 Sonograms of short-axis views of the same sciatic nerve (yellow arrows) demonstrating the potential benefit of increased transducer pressure. The image in (A) is with light transducer pressure and the image in (B) has increased transducer pressure. Note the increased resolution of the fascicular architecture of the deep sciatic nerve with the increased transducer pressure (B). Nerves can also be precisely measured with most ultrasound instruments. Cross-sectional area measurements of nerves in short axis are the most commonly used. This can be performed both by direct tracing inside the border of the nerve or more indirectly by the use of calipers and an ellipse. With either technique, the measurement should be performed on the inner aspect of the outer epineurium (Figure 9.13). Once adequate experience has been gained, the direct tracing method is generally preferable for reliability. Care should be used to establish that the measurement of the nerve is being obtained with the image as perpendicular as possible to obtain a reliable measurement. This usually means that the transducer should be oriented to create the smallest cross-sectional area possible while maintaining a short-axis plain. Obliquity of the image can create an artifactually inaccurate large cross-sectional area (Figure 9.14). With nerves that are relatively small in size, measurement of the diameter in short axis rather than cross-sectional area is more practical because reliable cross-sectional area cannot be obtained. FIGURE 9.13 Sonograms of short-axis views of a nerve. The image in (A) is the nerve with the transducer place in perpendicular position noted by the smallest cross-sectional area. The image in (B) is the same picture with the nerve measured using the direct tracing method. Note that the trace is at the inner border of the outer epineurium. FIGURE 9.14 Sonograms of short-axis views of the median nerve in the forearm. The image in (A) demonstrates the nerve with the transducer in the proper perpendicular position and (B) shows the direct tracing for cross-sectional area of that image. The image in (C) demonstrates the nerve with the transducer in a somewhat oblique position to the nerve creating an appearance of an abnormally large cross-sectional area. The image in (D) shows the direct tracing method with the oblique image. These images illustrate the importance of being precisely perpendicular to the nerve to obtain accurate cross-sectional area measurements. The diameter is also used for measurement of nerves in long-axis view (Figure 9.15). Measurement in this plane is often more challenging because the nerves often do not follow a straight course. The nerve should be scanned sufficiently to establish that the transducer is appropriately aligned over the maximum diameter of the nerve. The surrounding region should be assessed to reliably confirm that only nerve tissue is being measured. The diameter measurements should also be correlated with those obtained in short-axis view to confirm accuracy. FIGURE 9.15 Sonograms of a long-axis view of the median nerve (A) as well as a view of the same image with diameter measurement (B). The appearance of peripheral nerves on ultrasound due to focal injury or generalized disease can be variable and is often related to the extent of the pathology. Focal neuropathies often present with abnormal swelling that is usually just proximal to the site of the injury (Figure 9.16). However, there can be some variation in the presentation (Figure 9.17). Precise measurements and use of side-to-side comparisons when appropriate can be helpful. The measurements most frequently used are in short axis but long-axis views also provide needed perspective. At the current time, there is considerable variation between published normal values with respect to cross-sectional areas with many peripheral nerves. This seems to reflect variation in the manner in which the nerves are measured, among other factors. The median nerve at the carpal tunnel has been the most frequently studied nerve with ultrasound. Many studies of the median nerve have established slightly different normal values, but there is general consensus that a cross-sectional area of greater than 13 mm2 is highly predictive for the presence of median neuropathy at the carpal tunnel. Many feel that a cross-sectional area in the realm of 10 to 13 mm2 is also abnormal. Ultrasound also has sensitivity for identifying median neuropathy that is relatively similar to electrodiagnostic studies. Ultrasound, to this point, has not been shown to be as valuable as electrodiagnosis for determining the relative severity of neuropathies. FIGURE 9.16 Illustration of a nerve entrapment. The nerve shows focal enlargement just proximal to the entrapment site (red arrows). Peripheral nerve size has variation with body mass index, gender, age, and other factors. Using unaffected areas of a peripheral nerve for reference can be helpful in determining pathology (Figure 9.18). In addition to size measurement, identification of changes in the normal architecture of the nerve can also reveal neuropathy (Figure 9.19). There is no consistently good correlation between the size of nerves and relative severity of the neuropathy, but visual disruption of the normal fascicular architecture is more often associated with axonal injury. Complete transection of the nerve (neurotmesis) can typically be distinguished from a nonfunctional nerve with the connective tissue intact (complete axonotmesis) on ultrasound (Figure 9.20). This is an advantage of ultrasound over routine physical examination and electrophysiologic studies, which cannot reliably distinguish these conditions. This determination can enhance acumen for treatment decisions, including surgical intervention. FIGURE 9.17 Sonograms demonstrating long-axis views of nerve swelling in different entrapment neuropathies. The image in (A) shows a typical entrapment pattern with an ulnar neuropathy at the elbow with distal constriction (superior yellow arrow to the right) and a more proximal focal enlargement (inferior yellow arrow to the left). The other images show postoperative median neuropathy at the carpal tunnel. In (B), there is focal constriction from scarring in the middle and enlargement both proximally and distally to that level. The image in (C) shows a diffuse enlargement in between two areas of focal constriction. In (D), the median nerve is diffusely swollen with multiple areas of tethering from scar. These images demonstrate examples of different presentations of focal neuropathies and reflect the need to examine the entire area of potential pathology. FIGURE 9.18 Sonograms demonstrating short-axis views of the median nerve (yellow arrow) in an individual with median nerve at the carpal tunnel. The image in (A) shows the median nerve at the carpal tunnel and (B) shows the direct tracing method for calculating the cross-sectional area. The image in (C) shows the median nerve at the level of the distal forearm in the region of the pronator quadratus (PQ). The image in (D) shows the direct tracing of the nerve at this level. The use of an unaffected area, in this case the distal forearm, helps illustrate the relative degree of abnormality seen at the site of entrapment. FIGURE 9.19 Sonogram demonstrating a long-axis view of a focal median neuropathy (yellow arrows) in the distal forearm from a crush injury. Note that there is relatively minimal swelling at the area of injury but significant enlargement of the fascicular architecture. FIGURE 9.20 Sonograms demonstrating long-axis views of injuries to peripheral nerves. Ultrasound can often demonstrate the difference between a functional axonotmesis with connective tissue still in continuity (A) and a complete neurotmesis where the connective tissue is not in continuity (B). Note in (B) that the nerve tissue is separated (yellow arrows). This is an important feature of imaging tools such as ultrasound, because this distinction cannot be reliably made with conventional electrodiagnostic techniques. 1) Peripheral nerves have a fascicular architecture that differs from the fibrillar architecture of tendons. 2) Use easy to recognize anatomic landmarks when attempting to visualize nerves that are challenging to identify. 3) Short-axis measurements of peripheral nerves should be made at the inner border of the outer epineurium. 4) Peripheral nerves should always be measured in both short and long axis when distinguishing pathology. 5) Assessment of peripheral nerve pathology should always be considered in the appropriate clinical context.
Imaging Nerve
NORMAL NERVE ARCHITECTURE
NERVE SCANNING TECHNIQUES
NERVE PATHOLOGY
REMEMBER
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree