Abdominal pain is a common cause for emergency department visits in the United States, and biliary tract disease is the fifth most common cause of hospital admission. Common causes of acute hepatobiliary include gallstones and its associated complications and multiple other hepatobiliary etiologies, including infectious, inflammatory, vascular, and neoplastic causes. Postoperative complications of the biliary tract can result in an acute abdomen. Imaging of the hepatobiliary tree is integral in the diagnostic evaluation of acute hepatobiliary dysfunction, and imaging of the biliary tree requires a multimodality approach utilizing ultrasound, computed tomography, nuclear medicine, and MR imaging.
Key points
- •
Abdominal pain is a common cause for emergency department visits in the United States, and biliary tract disease is the fifth most common cause of hospital admission.
- •
Common causes of acute hepatobiliary include gallstones and its associated complications and multiple other hepatobiliary etiologies, including infectious, inflammatory, vascular, and neoplastic causes.
- •
Postoperative complications of the biliary tract can result in an acute abdomen.
- •
Imaging of the hepatobiliary tree is integral in the diagnostic evaluation of acute hepatobiliary dysfunction, and imaging of the biliary tree requires a multimodality approach utilizing ultrasound, computed tomography, nuclear medicine, and MR imaging.
Introduction
Abdominal pain is 1 of the top 5 causes of emergency department visits in the adult population. Within this population, biliary tract disease is the fifth most common cause of hospital admission in the 18 year old to 44 year old age group. Common causes of acute hepatobiliary include gallstones and its associated complications. There are many additional hepatobiliary etiologies, however, including infectious, inflammatory, vascular, and neoplastic causes. Postoperative complications of the biliary tract also may be seen in the setting of an acute abdomen. In addition to a comprehensive history and physical along with appropriate laboratory tests, imaging is an integral part of the diagnostic evaluation of acute hepatobiliary dysfunction, and imaging of the biliary tree often entails a multimodality approach, including any combination of ultrasound (US), computed tomography (CT), nuclear medicine, and MR imaging.
Imaging modalities
Ultrasound
In the setting of biliary disease, US is often the imaging modality of choice. It is an excellent modality for detection of gallstones, in particular those that are radiolucent on CT. US can be used for the assessment for ductal dilatation or presence of fluid collection. US often is limited, however, in its ability to identify a cause for these findings. Doppler US also can be useful for assessment of hepatic vasculature. This is of particular importance in the post-transplant patient.
Computed Tomography
CT is the most commonly utilized imaging modality to assess acute abdominal pain and plays a major role in the evaluation of acute hepatobiliary disease. It is best performed after administration of intravenous contrast, when possible, and is an excellent modality for assessing hepatic parenchyma and adjacent structures, such as the pancreas, kidney, and stomach. CT also is useful for identifying fluid collections, but, as with US, there are limitations, including inability to definitely characterize intraabdominal and pelvic collections and to identify an etiology for the patient’s symptoms and potential underestimation of gallstone burden because many stones are radiolucent.
Nuclear Medicine
Hepatobiliary iminodiacetic acid scan (HIDA) scan is performed by administering a technetium Tc 99m iminodiacetic acid analog, which is taken up by hepatocytes and excreted into the biliary tree. It is an excellent modality for the detection of cystic duct obstruction in the setting of acute cholecystitis. False-positive results may occur in the settings of severe liver disease, prior sphincterotomy, prolonged fasting, and prior administration of cholecystokinin. HIDA scan also may offer complementary information to US or CT, in the postoperative setting for diagnosis of biliary leak.
MR Imaging
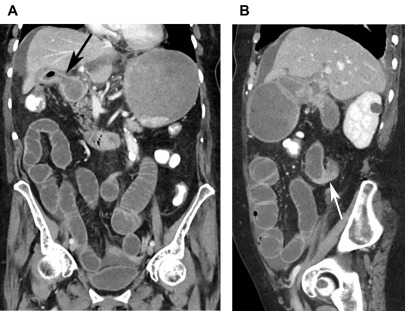
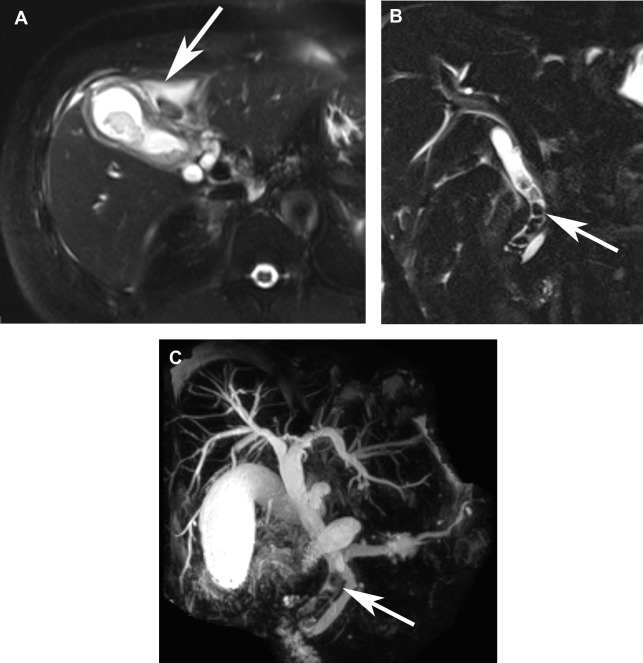
As with CT, MR imaging offers excellent soft tissue characterization, specifically in evaluating hepatic parenchyma as well as the adjacent organs. Unlike CT, it also is sensitive for detecting gallstones. MR cholangiopancreatography (MRCP) also may be performed, taking advantage of heavily T2-weighted images, to evaluate the biliary tree ( Fig. 1 ). In the postcholecystectomy patient, administration of a hepatobiliary agent may offer functional and anatomic information, including assessing the anatomy and detecting a biliary leak. Patients with normal liver function excrete contrast into the common bile duct in approximately 20 minutes after administration of gadoxetate. This also offers anatomic information because excreted contrast delineates the biliary tree and in the presence of a leak can localize the site of injury.
Inflammation/infection
Acute Cholecystitis
Cholelithiasis is present in 10% to 15% of the American population. Approximately 2% to 4% of patients with gallstones develop symptoms, most commonly biliary colic. Acute cholecystitis should be suspected in the setting of fever and is caused by cystic duct obstruction with secondary irritation of the gallbladder by bile salts.
US is the preferred imaging modality for detection of cholelithiasis. Because cystic duct obstruction cannot always be assessed on US, acute cholecystitis also must be identified based on secondary signs, such as cholelithiasis, gallbladder wall thickening, wall edema, and pericholecystic fluid ( Fig. 2 A, B). A distinct advantage of US is its ability to elicit a sonographic Murphy sign. Despite being rapid and effective, sonographic findings often are difficult to interpret given that gallbladder wall abnormalities are nonspecific and also can be seen in the setting of liver, heart or renal disease.
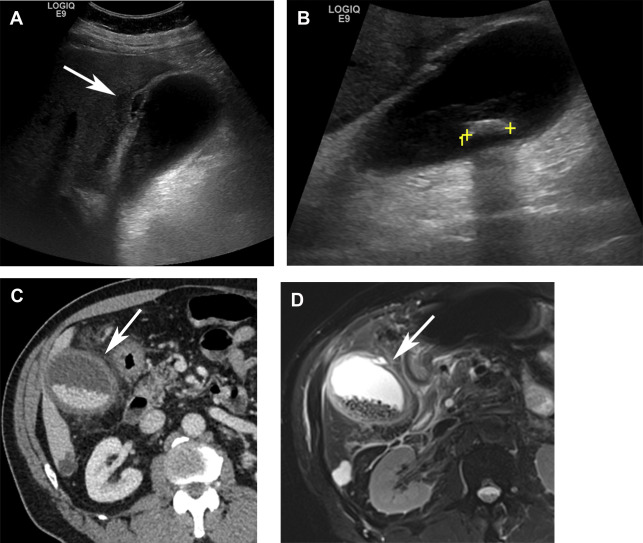
CT may offer complementary information and can diagnose acute cholecystitis by identifying a distended gallbladder with wall thickening, wall edema, pericholecystic fluid, and pericholecystic stranding ( Fig. 2 C). Gallstones may or may not be seen on CT. Use of dual-energy CT, however, with creation of monochromatic low or high kiloelectron volt images, has been shown to increase conspicuity of stones ( Fig. 3 ). MR/MRCP may show similar findings to CT with the added benefit of the T2-weighted sequence, which has a higher sensitivity for stone detection ( Fig. 2 D). Review of diffusion-weighted images also has been shown helpful for differentiation of acute from chronic cholecystitis.
Equivocal cases can be further evaluated with HIDA. On HIDA scan, acute cholecystitis can demonstrate cystic duct obstruction by showing radiotracer excretion into small bowel without accumulation in the gallbladder. Morphine administration can be attempted to increase muscle tone in the sphincter of Oddi and promote gallbladder filling. In cases of chronic cholecystitis, the cystic duct is patent and radiotracer can accumulate in the gallbladder. These cases may demonstrate delayed gallbladder filling or delayed transit to small bowel. Administration of cholecystokinin and evaluation for an impaired ejection fraction can be helpful in these cases.
Acute Acalculous Cholecystitis
Acute acalculous cholecystitis (AAC) is characterized by gallbladder inflammation without obstruction from gallstones. It often affects critically ill patients particularly after surgery, trauma, burn injury and cardiac arrest. Diabetes, abdominal vasculitis, and congestive heart failure also have been associated with AAC. AAC in critically ill patients tends to have a worse prognosis with a mortality rate of up to 50% and these patients also are more likely to develop complications of cholecystitis, such as gangrene and perforation. As such, it is of critical importance to diagnose and treat these patients in a timely manner. Early imaging is necessary for these patients and demonstrates similar findings to acute calculous cholecystitis, including gallbladder distention, wall thickening, and pericholecystic fluid without the presence of gallstones. The sonographic Murphy sign generally is unreliable in these cases because the patients are too ill and may be medicated.
Complications of Acute Cholecystitis
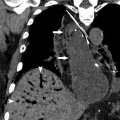
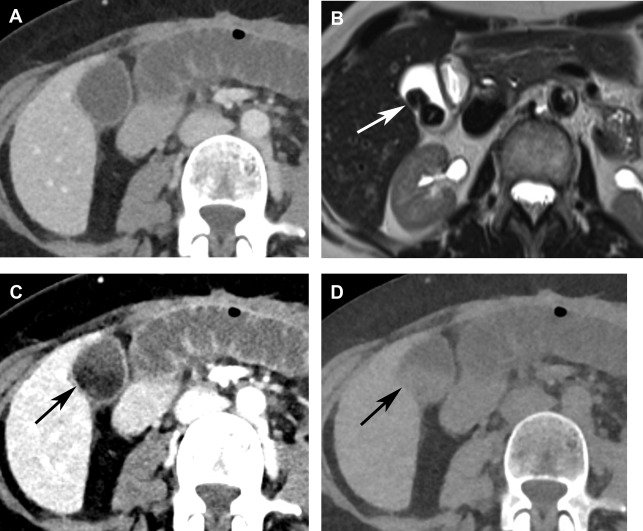
Acute cholecystitis can be complicated by secondary infection of the inflamed gallbladder, which can lead to emphysematous cholecystitis and gangrenous cholecystitis. Emphysematous cholecystitis is the result of superinfection of the gallbladder by a gas-forming organism and commonly affects diabetics, men more than women, and patients 40 years old to 60 years old. On imaging, it is readily identified on CT with intramural gas involving the gallbladder. US can be difficult because gas in the gallbladder wall can obscure the gallbladder or be mistaken for bowel gas. Early diagnosis is important because these patients are prone to develop gangrene, perforation ( Fig. 4 ) and abscess.
Gangrenous cholecystitis is associated with increased morbidity and mortality. It is characterized by the presence of intramural hemorrhage, necrosis, and development of microabscesses. On imaging, mural irregularity, sloughed intraluminal membranes, and intraluminal debris suggest the presence of gangrenous cholecystitis. In these cases, evidence of perforation as evidenced by focal wall discontinuity, extraluminal gallstones, and pericholecystic abscesses also may be detected. Dual-energy CT images may be helpful because the gallbladder wall may demonstrate areas of absent iodine uptake.
Xanthogranulomatous Cholecystitis
Xanthogranulomatous cholecystitis (XGC) is a rare and chronic form of cholecystitis characterized by a destructive inflammatory process with features of perforation, abscess formation, fistula, and invasion of adjacent structures, and which often is difficult to differentiate from gallbladder carcinoma. Radiologic findings include diffuse or focal gallbladder wall thickening with hypoattenuating intramural nodules, heterogeneous wall enhancement, infiltration of the liver and adjacent pericholecystic fat, and continuity of the enhancing gallbladder mucosa ( Fig. 5 ). Similar findings are demonstrated on MR imaging, noting high T2 signal corresponding to hypoattenuating intramural nodules on CT, which represent xanthogranulomas. This finding has been suggested to be a discriminating feature from gallbladder carcinoma; however, cholecystectomy is often performed to confirm the diagnosis and plan definitive treatment.

Acute Ascending Cholangitis
Acute cholangitis occurs in the setting of common biliary obstruction. The most common cause for cholangitis is choledocholithiasis, but other causes include malignant obstruction or prior biliary manipulation. The diagnosis of cholangitis is made clinically by the presence of Charcot triad of fever, jaundice, and right upper quadrant pain. Reynolds pentad also includes hypotension and altered mental status. Imaging with US may detect the presence of ductal dilatation. CT evaluation of the biliary tree may demonstrate choledocholithiasis, periductal inflammation, ductal wall thickening and mural enhancement. MRCP shows similar findings but may also show parenchymal changes related to cholangitis, specifically wedge-shaped or peribiliary regions of T2 hyperintensity or enhancement. Unless stones are impacted, choledocholithiasis on both CT and MR imaging often are dependent in position. On CT, stones commonly are angulated and lamellated with an anterior crescent of fluid or gas. MRCP may have a higher sensitivity for detecting radiolucent stones but CT is a better modality for differentiating pneumobilia from choledocholithiasis.
Mirizzi Syndrome
Mirizzi syndrome is defined by common hepatic duct obstruction from extrinsic compression due to stone in the gallbladder infundibulum or cystic duct. As with other acute biliary disease, patients present with fever, jaundice, and/or right upper quadrant pain. Anatomically, a parallel configuration of the cystic and common hepatic ducts along with a long, low inserting cystic duct predisposes patients to this entity. On imaging, US may detect an ectatic common hepatic duct. CT may show a similar finding and also may demonstrate periportal inflammation. MRCP is the preferred imaging modality given its ability to delineate ductal anatomy. On heavily T2-weighted images, MRCP may demonstrate a stone impacted in the cystic duct or gallbladder infundibulum compressing the common hepatic duct, which is dilated proximal to the level of the stone. Distally, the common bile duct is normal in caliber.
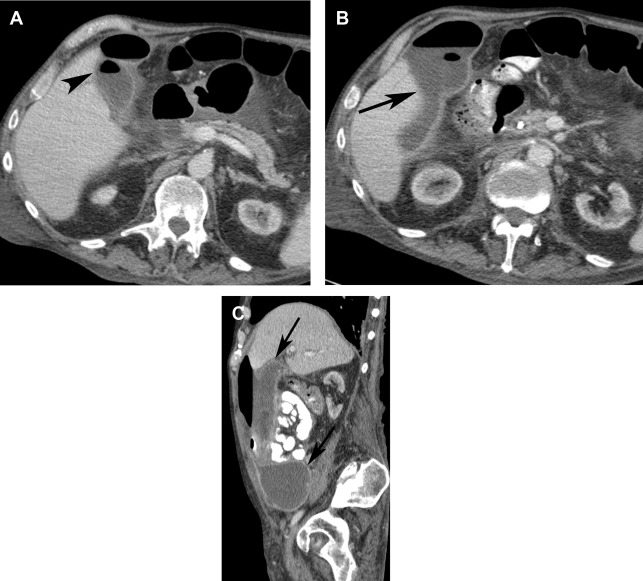
Gallstone Ileus
A rare complication of gallstones is gallstone ileus, which is characterized by mechanical obstruction of the gastrointestinal tract secondary to an impacted gallstone. Large stones (>2 cm) within the gallbladder can pass into the gastrointestinal tract by eroding into an adjacent bowel loop. It then can cause obstruction at sites of decreased luminal diameter, most commonly the terminal ileum and ileocecal valve. Rarely, the gallstone can migrate proximally causing gastric outlet obstruction, a phenomenon known as Bouveret syndrome. Cases of gallstones ileus are best diagnosed on CT, which demonstrate dilated bowel loops to the level an ectopic gallstone, pneumobilia as well as a fistulous connection between the gallbladder and adjacent bowel loop ( Fig. 6 ).