Central nervous system infections account for 1% of primary hospital admissions and 2% of nosocomial infections and when encountered require prompt diagnosis and initiation of specific treatment. Imaging findings are mostly nonspecific with respect to the causative pathogen. This article describes the anatomy of cranial meninges and extra-axial spaces of the brain. Characteristic findings and recent advances in neuroimaging of meningitis and its complications and ventriculitis are summarized, and certain noninfectious causes of meningitis and meningitis mimics are described.
- •
Meningeal enhancement is nonspecific and can be seen in meningitis of any cause, including noninfectious processes.
- •
Imaging helps in noninvasive differentiation of infective from the noninfective conditions and helps in better clinical decision making.
- •
In acute meningitis, meningeal enhancement is located over the cerebral convexity, whereas in chronic meningitis it is most prominent in the basal cisterns.
- •
The role of neuroimaging is to confirm suspected meningitis, rule out meningitis mimics, evaluate for complications, and rule out increased intracranial pressure before lumbar puncture.
- •
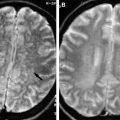
Magnetic resonance imaging is critical in evaluating complications of meningitis (eg, ventriculitis, extra-axial collections, cerebritis and abscess, herniations, cranial neuropathy, and vasculopathy).
Introduction
Central nervous system (CNS) infections account for 1% of primary hospital admissions and 2% of nosocomial infections and when encountered, require prompt diagnosis and initiation of specific treatment. The brain has some unique peculiarities like absence of lymphatics, lack of capillaries in the subarachnoid space, and presence of cerebrospinal fluid (CSF), which is an excellent culture medium for dissemination of infectious processes, in the subarachnoid space and into the ventricular system. The normal brain responds to these insults in a limited and stereotypical fashion, and in most cases there is concomitant abnormality of the blood-brain barrier, with associated enhancement. Therefore, the imaging findings are mostly nonspecific with respect to the causative pathogen. However, imaging techniques are sensitive for detecting an abnormality, localizing it, and in many cases categorizing the lesion into infectious or inflammatory disease versus neoplastic. Contrast enhancement is generally useful, and in the light of clinical history and examination findings the radiologist can provide a probable differential diagnosis. Whereas analysis of CSF remains the gold standard to identify the infectious agent, neuroimaging plays a pivotal role not only in diagnosis but also in monitoring therapeutic response. This article begins by briefly describing the anatomy of cranial meninges and extra-axial spaces of the brain. Characteristic findings and recent advances in neuroimaging of meningitis and its complications and ventriculitis are then summarized, and certain noninfectious causes of meningitis and meningitis mimics are described.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree