Prevascular mediastinal masses include a wide range of benign and malignant entities. Localization of mediastinal masses to specific compartments together with characteristic imaging findings and demographic and clinical information allows formulation of a focused differential diagnosis. Radiologists may use these methods to distinguish between surgical and nonsurgical cases and thus inform patient management and have an impact on outcomes. Treatment of choice varies based on the pathology, ranging from no intervention or serial imaging follow-up to surgical excision, chemotherapy, and/or radiation.
Key points
- •
Various neoplastic and non-neoplastic entities may affect the prevascular mediastinum.
- •
Most prevascular mediastinal masses are discovered incidentally and are characterized further with contrast-enhanced chest computed tomography.
- •
Correlation of specific imaging features with demographic and clinical information may allow radiologists to provide a focused differential or a specific diagnosis.
- •
By distinguishing surgical from nonsurgical lesions, radiologists play a crucial role in the multidisciplinary approach to the management of prevascular mediastinal pathologies.
Introduction
The mediastinum contains many organs, structures, and tissues. A wide variety of entities may arise primarily from these structures or secondarily involve this region, including neoplasms, glandular enlargement, congenital and vascular abnormalities, lymphadenopathy, and mesenchymal lesions. Localization of mediastinal masses to specific compartments, together with demographic and clinical information, allows formulation of a focused differential diagnosis and helps guide further evaluation and management. Anterior, middle, and posterior mediastinal compartments have been used for decades in radiographic interpretation. The International Thymic Malignancy Interest Group recently redefined the mediastinal compartments based on cross-sectional imaging, separating the mediastinum into prevascular, visceral, and paravertebral compartments. Contents of the prevascular compartment include the thymus, fat, lymph nodes, left brachiocephalic vein, small vessels, nerves, and lymphatic channels. The most common pathologies that occur in this compartment include thymic lesions, germ cell neoplasms (GCNs), lymphoma, lymphatic malformations, metastatic disease, and glandular lesions.
Mediastinal masses are uncommon. They typically are discovered on radiography and are characterized further with computed tomography (CT) and/or MR imaging. More than half of all mediastinal masses arise from the prevascular compartment. When classic imaging features are present, a specific diagnosis may be suggested based solely on CT imaging features. The appearances of prevascular mediastinal lesions may overlap, however, and additional imaging studies, laboratory tests, and tissue sampling often are required for a definitive diagnosis.
The true incidence of prevascular mediastinal masses is difficult to determine largely due to historical variability in clinical and radiologic classification systems of mediastinal compartments in published studies, which may or may not include congenital and nonsurgical lesions and due to variability regarding the inclusion of lymphoma. The most common tumors of the prevascular mediastinum are thymic epithelial neoplasms and lymphoma. Other neoplasms include neuroendocrine tumors, GCNs, and a variety of thymic neoplasms. The most common non-neoplastic masses are cystic lesions, which may be congenital or acquired. Vascular abnormalities, lymphatic malformations, mediastinal thyroid and parathyroid tissue, and thymic enlargement also may occur.
Imaging of the prevascular mediastinum
Radiography
Chest radiography is the imaging study performed most commonly and often is the first imaging modality to demonstrate a mediastinal abnormality. A systematic approach to radiographic analysis and knowledge of normal mediastinal lines, stripes, and interfaces allow radiologists to identify and localize mediastinal lesions. Although small mediastinal lesions may produce normal or subtle findings, large lesions typically produce contour abnormalities or distortion of the aforementioned lines, stripes, and interfaces on posteroanterior (PA) radiography ( Fig. 1 ). The lateral radiograph then is used to localize the lesion to the anterior mediastinum. Identification of the hilum overlay sign allows differentiation of an anterior mediastinal lesion from a hilar mass.

Computed Tomography
Contrast-enhanced CT is the modality of choice for evaluating mediastinal masses and is equal to or superior to MR imaging in diagnosing most lesions, with the exception of thymic cysts. CT analysis of a prevascular mediastinal lesion should be systematic and should address multiple characteristics, including (1) location, size, morphology, and margins; (2) density/attenuation and enhancement characteristics; (3) internal composition, including soft tissue, fat, fluid, and calcification; (4) relationship with adjacent structures, including mass effect and/or invasion; and (5) presence or absence of lymphadenopathy.
MR Imaging
MR imaging is not performed routinely for the assessment of mediastinal masses but is the optimal imaging modality for distinguishing cystic from solid lesions, identifying cystic and/or necrotic lesion components, characterizing cystic lesions as to the presence of septations and mural nodularity, and distinguishing normal or hyperplastic thymic tissue from neoplasia.
Fluorodeoxyglucose PET/Computed Tomography
18 F-fluorodeoxyglucose (FDG) PET/CT has a limited role in the evaluation of mediastinal masses and often is nonspecific given that many infectious and inflammatory processes result in increased FDG uptake, which can be mistaken for malignancy. Although FDG PET/CT has been used to distinguish between low-grade thymoma, high-grade thymoma, and thymic carcinoma, , there is significant overlap between FDG-avid neoplasms, including high-grade thymic epithelial neoplasms, lymphoma, paraganglioma, and nonseminomatous malignant GCNs. FDG PET/CT, however, is the imaging modality of choice for staging and restaging lymphoma. The overall consensus suggests that FDG PET/CT may have an ancillary role in the diagnostic workup of prevascular mediastinal masses, but accuracy and specificity are limited, with significant overlap between different mediastinal pathologies.
Thymic hyperplasia
Normal thymic tissue typically is identified in the prevascular mediastinum of young patients and gradually decreases with age, with fatty replacement usually complete by age 40. When uniform thymic enlargement with a bilobed morphology and intercalated fat is present, thymic hyperplasia is the leading consideration. Rebound hyperplasia is defined as an increase in thymic volume by greater than 50% compared with baseline and typically occurs after chemotherapy, radiation therapy, prolonged corticosteroid treatment, or after physiologic stress from severe injuries or burns. Thymic hyperplasia, specifically lymphoid (follicular) hyperplasia, is characterized by thymic lymphoid follicles with or without concurrent increase in glandular size. It typically occurs in patients with underlying systemic disorders, such as myasthenia gravis, collagen vascular disease, systemic lupus erythematosus, human immunodeficiency virus infection, and hyperthyroidism ( Fig. 2 A).

Thymic hyperplasia may manifest on CT as a diffuse, focal, or asymmetric nodular or masslike heterogeneous soft tissue lesion with lobular margins and may mimic a mediastinal neoplasm. If suspicion for thymic hyperplasia is high, short-term interval follow-up CT can be obtained, with an expected decrease in size. Alternatively, chemical-shift MR imaging may be performed to confirm intralesional fat, an expected finding in thymic hyperplasia ( Fig. 2 B), or suggest the diagnosis of thymic neoplasia.
Thymic epithelial neoplasms
Thymic epithelial neoplasms are rare and account for 0.2% to 1.5% of all malignancies in the United States, but are the most common nonlymphomatous primary neoplasm of the prevascular mediastinum. , These tumors include thymomas and thymic carcinomas. Complete resection when possible is the treatment of choice for these neoplasms. Neoadjuvant and/or adjuvant systemic therapy and radiation often are utilized for invasive lesions. ,
Thymoma
Thymoma is the most common primary neoplasm of the prevascular mediastinum and is the most common thymic epithelial neoplasm, with a reported 0.15 cases per 100,000 persons, accounting for 20% of prevascular mediastinal masses in adults. , The highest incidence occurs in middle-aged patients, typically between 40 years and 60 years, without gender predilection. , These generally are slow-growing encapsulated neoplasms but may invade vascular structures and/or involve the pleura and pericardium. Distant metastases are rare. , Affected patients may be asymptomatic, may have symptoms related to mass effect or local invasion, or may present with a paraneoplastic syndrome. Such parathymic syndromes include myasthenia gravis, pure red cell aplasia/Diamond-Blackfan syndrome, aplastic anemia, and hypogammaglobulinemia. Thymomas are also associated with autoimmune disorders such as Hashimoto’s thyroiditis, systemic lupus erythematosus, polymyositis, and rheumatoid arthritis. The most common symptoms reported at presentation are chest pain, dyspnea, cough, dysphagia, diaphragmatic paralysis, and superior vena cava (SVC) syndrome.
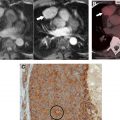
More than 80% of thymomas are diagnosed accurately on CT or MR imaging. CT of suspected thymoma should be performed with contrast for more accurate identification of invasive features. Thymoma should be the leading diagnostic consideration when a homogeneous or slightly heterogeneous rounded or lobular prevascular mediastinal mass is present in a patient over the age of 40. A tissue plane between the mass and adjacent structures may be visible in encapsulated lesions ( Fig. 3 ). Heterogeneity within the mass due to internal cystic or necrotic foci, irregular lobular contours, and intrinsic calcifications suggest invasive thymoma , ( Figs. 4 and 5 ). Invasive lesions may exhibit infiltration of the mediastinal fat, vascular encasement or frank invasion, and/or pleural and pericardial metastases. Lymphadenopathy typically is absent. The presence of local invasion, lymphadenopathy, pleural effusion, or distant metastases should raise concern for more aggressive neoplasms, such as thymic carcinoma or carcinoid ( Fig. 6 ).




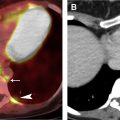
Thymic Carcinoma
Thymic carcinomas are uncommon but represent approximately 20% of thymic epithelial neoplasms, and affected patients are often symptomatic. The mean age at presentation is 50 years. Imaging features may be indistinguishable from those of thymoma, but thymic carcinoma typically exhibits aggressive features, such as invasion of adjacent structures, lymphadenopathy, pleural/pericardial effusions, and distant metastases ( Fig. 7 ). Approximately 50% to 65% of patients have distant metastases at the time of diagnosis. In contrast to thymoma, paraneoplastic syndromes rarely are associated with thymic carcinoma.

Thymic neuroendocrine neoplasms
Thymic neuroendocrine neoplasms are the least common primary thymic tumors, comprising 2% to 5% of these lesions, and most frequently are carcinoids, specifically atypical carcinoids. The reported median age at presentation is 57 years, with a 3:1 male-to-female ratio. Approximately 25% develop in patients with multiple endocrine neoplasia (MEN) type 1. Most patients are symptomatic at diagnosis secondary to local invasion and mass effect and may present with paraneoplastic syndromes, most commonly Cushing syndrome, due to ectopic production of adrenocorticotropic hormone. Other paraneoplastic syndrome of inappropriate secretion of antidiuretic hormone (SIADH), and rarely carcinoid syndrome. Approximately one-third of affected patients are asymptomatic and may be diagnosed incidentally or during surveillance for MEN 1.
On imaging, these typically are aggressive, prevascular mediastinal soft tissue masses that may invade surrounding structures and often are associated with mediastinal lymphadenopathy ( Fig. 8 ). Surgical resection is the treatment of choice, with or without adjuvant or neoadjuvant systemic therapy and/or radiation therapy.

Lymphoma
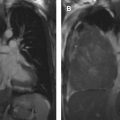
Lymphomas are heterogeneous neoplasms with frequent intrathoracic involvement and account for 4.9% of newly diagnosed malignancies. Lymphoma may arise primarily in the mediastinum or secondarily may involve it. A diagnosis of lymphoma should be favored over thymoma in younger patients and in those with a mediastinal mass and associated lymphadenopathy. Primary mediastinal lymphomas are rare, comprising approximately 1% of all lymphomas. Diagnosis of primary mediastinal lymphoma necessitates involvement of mediastinal lymph nodes, the thymus, or both, without evidence of extranodal or systemic disease at presentation. The most common cell types to primarily or secondarily involve the mediastinum are diffuse large B-cell lymphoma and Hodgkin lymphoma. Less common cell types include primary mediastinal (thymic) B-cell lymphoma, gray zone lymphoma (GZL), T-cell lymphoblastic lymphoma (TCLL), mucosa-associated lymphoid tissue (MALT) lymphoma, and peripheral T-cell lymphoma (PTCL). ,
Lymphoma should be considered when large, lobular, soft tissue masses and/or enlarged lymph nodes are identified in the prevascular mediastinum, particularly if there is involvement of other mediastinal compartments and lymph node stations or infiltration between or encasement of vascular structures, with or without mass effect or local invasion ( Fig. 9 A). Systemic B symptoms, such as fever, night sweats, and weight loss, in combination with typical imaging features, are highly suggestive of the diagnosis. More aggressive subtypes, such as GZL and TCLL, often exhibit increased heterogeneity and invasion of adjacent structures.