In this chapter, we discuss imaging of the cervical, thoracic, and lumbar spine. Although differences exist, many common themes are shared in both the selection and the interpretation of diagnostic studies for all regions of the spine. Our discussion of all spinal regions starts with interpretation of images, with a focus on computed tomography (CT) scan. We correlate CT findings with x-ray when possible, and we demonstrate associated soft-tissue abnormalities identified on magnetic resonance imaging (MRI). Don’t be daunted by the number of figures in this chapter—we explore injuries and nontraumatic spinal pathology in many imaging planes and in multiple modalities to maximize your three-dimensional understanding. The figure captions are designed to allow the figures to stand alone, so we spend relatively little time discussing specific fracture patterns in the text. The figures in the chapter span a range of important spinal pathology, moving from cephalad to caudad. The list in Table 3-1 can guide you to the relevant figure, where diagnostic features are discussed in detail.
| Content | Figure Number |
|---|---|
| Three-dimensional CT reconstructions of the normal cervical spine | 3-1 through 3-7 |
X-rays of the normal cervical spine
| |
| Normal sagittal CT views | 3-19 and 3-20 |
| Normal coronal CT view | 3-21 |
| Normal axial view | 3-22 |
| Occipital condyle fractures | 3-24 through 3-27 |
| C1 burst (Jefferson) fractures | 3-28 through 3-31 |
| Atlantoaxial (C1-C2) rotary fixations | 3-32 through 3-38 |
| C1 posterior arch fracture | 3-39 |
| C2 dens fractures, type II | 3-40 through 3-43 |
| C2 dens fractures, type III | 3-44 through 3-48 |
| Hangman’s fractures of C2 | 3-49 through 3-57 |
| Transverse process fractures | 3-58 and 3-98 |
| Cervical burst compression fractures | 3-59 through 3-62 |
| Teardrop flexion fractures | 3-63 through 3-66 |
| Jumped facets, bilateral and unilateral | 3-67 through 3-75 |
| Cervical facet fractures with spinal cord injury on MRI | 3-76 and 3-77 |
| Cervical lamina fractures | 3-78 through 3-80 |
| Acute cervical ligamentous injuries with x-ray, CT, and MRI findings | 3-81 through 3-84 |
| Three-column concept of spinal stability | 3-85 |
| T2 corner avulsion fractures (extension teardrop) | 3-86 and 3-87 |
| Thoracolumbar compression and burst fractures | 3-88 through 3-101 |
| Chance fractures | 3-99 through 3-101 |
| Thoracic spine metastatic disease with cord compression | 3-102 through 3-104 |
| Vertebral osteomyelitis and discitis | 3-105 through 3-107 |
| Spinal epidural abscesses | 3-108 through 3-110, 3-115, and 3-116 |
| Vertebral tuberculosis (Pott’s disease) | 3-111 through 3-116 |
| Degenerative joint disease and disc herniation | 3-117 through 3-120 |
| Cauda equina, normal and compression | 3-119 and 3-120 |
| Osteopetrosis | 3-121 and 3-122 |
| Ankylosing spondylitis | 3-123 through 3-127 |
| Spinal cord injuries on MRI | 3-77 and 3-127 |
| Penetrating spinal trauma | 3-128 through 3-131 |
| Motion artifact on MRI | 3-132 |
| Syrinx | 3-133 |
| Pseudosubluxation | 3-134 and 3-135 |
In many ways, the more difficult task for the emergency physician is not the interpretation of the image but the decision to image the spine. We review two well-validated clinical decision rules (CDRs) that can identify patients at low risk of cervical spine injury who do not require any imaging. Similar decision instruments can identify patients who require thoracic and lumbar imaging.
Imaging of the spine has undergone a revolution with the advent of multidetector CT with multiplanar reconstructions. We review the evidence for use of CT and x-ray, comparing their sensitivity for detection of fractures. Remarkably, the latest version of the American College of Radiology (ACR) Appropriate Guidelines for Imaging of Suspected Spine Trauma (2009) advocates thin-section CT as the primary screening study for suspected cervical spine injury in adults, removing plain radiography (x-ray) from this position. The three-view radiograph that has been the long-standing screening test in the emergency department is now recommended by the ACR “only when CT is not readily available.” Radiography is described in this document as “not … a substitute for CT.” The ACR cites a lack of evidence for recommendations of CT or x-ray as the primary screening tool for suspected cervical spine injury in children. We discuss the radiation burden and cost of cervical CT. The new ACR recommendation for a CT-first strategy guarantees an increase in the radiation exposure resulting from any screening for cervical spine injury. Consequently, an even greater emphasis should be placed on applying reliable CDRs. Let’s begin our discussion with the cervical spine, followed by a parallel discussion of the thoracic and lumbar spine.
Epidemiology of Cervical Spine Injury
Cervical spine injuries occur in approximately 2% to 4% of blunt trauma cases, and diagnostic imaging plays a pivotal role in the evaluation of patients for these potentially life-threatening or seriously debilitating injuries. In addition, nontraumatic cervical spine pathology occasionally requires imaging in the emergency department. This evaluation differs from the evaluation in trauma, as fractures or other bony pathology may not be present. The incidence of cervical injuries is relatively independent of the setting—level I, II, and III trauma centers (the U.S. designation) all encounter cervical spine injuries with similar frequency, and emergency physicians must be intimately familiar with the imaging required to diagnose these dangerous injuries. In one study of 165 U.S. medical centers involving 111,219 patients, 4.3% of patients had injuries, at similar rates, in both academic and nonacademic centers, regardless of trauma center type (I through III). The National Emergency X-radiography Utilization Study group, which is discussed in more detail later in regard to its CDR, found similar rates of injury: 2.4% of 34,069 patients in 21 U.S. medical centers.
Imaging the Cervical Spine Following Trauma: Application and Interpretation of Imaging Modalities
Cervical spine imaging following trauma must perform a number of clinical functions. These include identification of fractures, ligamentous injuries, and injuries to neurologic structures, including the spinal cord and nerve roots. Diagnostic modalities for cervical spine imaging are plain film, CT scan, and MRI. We consider each of these in turn, with examples of the types of pathology detected or ruled out and the limitations of each technique. Although the ACR now recommends CT rather than x-ray as the primary screening tool in adults, plain x-ray is still widely used in children, and CT is not available in all settings. We review the interpretation of x-rays and CT, recognizing that some patients may not undergo both tests. At this time, MRI is more rarely interpreted by emergency physicians, and we thus review MRI interpretation in less detail.
Evaluating for Fracture or Dislocation with Plain X-ray
Plain films in a neutral anatomic position with the patient immobilized in a cervical collar have long been the standard test to evaluate for bony fractures and dislocations. Although plain x-rays are still widely used, CT has increasingly become the primary modality for evaluation of fracture due to its higher sensitivity. Nonetheless, plain x-rays continue to play an important role in screening for fractures. Because of their limited sensitivity, plain x-rays should not be used to “rule out fracture” in cases with a high pretest probability of cervical spine injury.
Plain x-rays of the cervical spine identify fractures by three major methods:
- •
Direct visualization of fractures (discontinuity of the bony cortex)
- •
Misalignment of bony structures, suggesting possible fracture or dislocation
- •
Soft-tissue changes, suggesting underlying fracture
Plain x-rays do not directly identify abnormalities of soft tissues such as spinal ligaments, although gross misalignment of vertebral bodies almost always indicates concurrent ligamentous injury. Plain x-rays also do not directly identify spinal cord injuries, although x-ray abnormalities showing impingement upon the spinal canal imply cord impingement. Direct visualization of ligamentous and cord injuries requires MRI. CT scan is useful in delineating fractures and dislocations in greater detail. As described later, CT with multiplanar reconstructions can visualize some soft-tissue injuries and, when normal, indicates a low likelihood of unstable cervical spine injury.
Standard Plain X-ray, Three Views
Figures 3-1 through 3-7 demonstrate three-dimensional CT models of the cervical spine. Review these, as they will assist you in understanding cervical spine anatomy and the information to be gleaned from the two-dimensional projections obtained in plain x-ray. An adequate cervical spine plain x-ray series consists of three images: a lateral, an anterior – posterior (AP), and an open-mouth odontoid view ( Figure 3-8 ). It is extremely important that adequate x-rays are obtained to maximize the sensitivity of this technique.







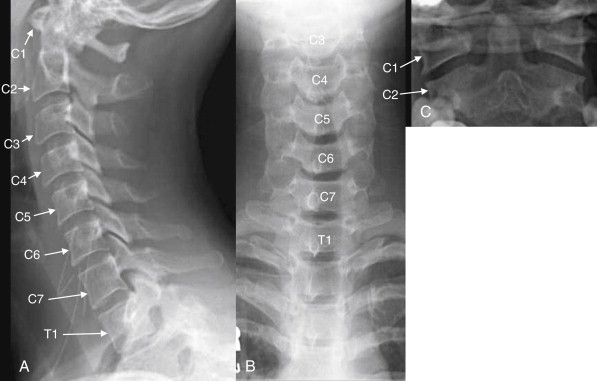
Normal Features of the Lateral X-ray
The lateral x-ray ( Figures 3-8 through 3-13 ; see also 3-19 and 3-20 ) provides information about gross fractures, as well as alignment of vertebral bodies relative to one another. In addition, prevertebral soft tissue widening may suggest soft-tissue hematoma or swelling, a surrogate marker of fractures that may themselves be invisible on plain film. The x-ray must visualize the cervical spine from the skull base to the C7-T1 (cervical seventh vertebra–thoracic first vertebra) junction. This is not an arbitrary definition of an adequate plain film. An x-ray that fails to visualize the entire cervical spine and its junctions with the adjacent skull and thoracic spine may miss injuries. Widening of the space between the C1 vertebra and the skull base may be a subtle indication of a devastating occipital–cervical dissociation—although this injury is usually clinically evident with a moribund patient with quadriplegia. At the caudad end of the cervical spine, it is essential to visualize the C7-T1 junction to avoid missing subluxation of these vertebral bodies relative to one another. This injury is made more likely by the sudden change in the mobility of the spine, from the highly mobile cervical spine to the relative immobile thoracic spine, which is supported by the buttresses of the ribs.


- 1
Anterior longitudinal ligament line (follows the anterior border of the vertebral bodies)
- 2.
Posterior longitudinal ligament line (follows the posterior border of the vertebral bodies)
- 3.
Spinolaminar line (follows the anterior border of the posterior spinous processes, where the lamina converge)
- 4.
Spinous processes line (follows the posterior border of the posterior spinous processes and does not fully parallel the other lines due to the increasing length of the spinous processes from C1 to C7)
The spinal canal, which houses the spinal cord, lies between lines 2 and 3.
If all lines are intact, the vertebral bodies should be properly aligned and the spinal canal should be preserved.


A normal lateral cervical spine image shows a gentle cervical lordosis—a curve with its convex border oriented anteriorly (see Figure 3-10 ). This lordosis may be straightened slightly due to the presence of the cervical collar. When all cervical vertebrae are intact and in normal alignment with one another, this cervical lordosis results in four parallel curved lines, for which the lateral x-ray should be inspected (the numbered lines in Figure 3-10 ):
- 1.
The anterior longitudinal ligament line, which follows the anterior border of the vertebral bodies.
- 2.
The posterior longitudinal ligament line, which follows the posterior border of the vertebral bodies.
- 3.
The spinolaminar line, which follows the anterior border of the posterior spinous processes, where the lamina converge.
- 4.
The spinous processes line, which follows the posterior border of the posterior spinous processes. It does not fully parallel the other lines because of the increasing length of the spinous processes from C1 to C7. The space between the posterior longitudinal ligament line and the spinolaminar line is the spinal canal. If these lines are intact and parallel, the spinal canal should be intact, and the spinal cord should be safely contained within it.
In addition, the lateral film should be examined with attention to the following:
- 5.
The predental space (see Figure 3-11 ), which separates the dens from the anterior ring of C1. Widening suggests dens or C1 ring fracture, or subluxation of the transverse ligament, which binds the dens to the anterior ring of C1. In adults, this space should be no more than 3 mm, and in children it should be no more than 4 to 5 mm.
- 6.
Prevertebral soft tissues (see Figure 3-12 ). Widening suggests cervical spine injury with soft-tissue swelling or hematoma. In adults, this distance should be less than 7 mm at C2 and less than 5 mm at C3 and C4. In children, a commonly cited distance is less than half the width of the adjacent vertebral body. False widening may occur in children under the age of 2 years if the image is obtained during expiration. Below C4, the airway moves anteriorly, the esophagus occupies the prevertebral space, and soft-tissue widths vary considerably, usually between 10 and 20 mm in adults. Soft-tissue width exceeding the width of the adjacent vertebral body suggests injury.
- 7.
The spinal facet joints ( Figure 3-13 ), which should overlap like shingles on a roof. Decreased overlap can occur in the case of a jumped or perched facet joint.

Figure 3-13
Assessment of facet joints.
A, Lateral cervical spine x-ray. B, Close-up. The facets should overlap like shingles on a roof. In the case of jumped or perched facet joints, the degree of facet overlap at the level of injury will be less than the overlap at uninjured levels. The facets can be recognized by their rhomboid shape in profile. Fracture through the facets and lamina is also common and should be looked for carefully.
- 8.
Widening of the distance between posterior spinous processes, which can indicate fracture or ligamentous injury.
Normal Features of the Anterior-posterior X-ray
The AP x-ray ( Figure 3-14 ) provides information about lateral alignment of vertebral bodies with one another. A small number of additional fractures ( particularly oblique fractures) may be noted on the AP x-ray, and subtle abnormalities from the lateral film may be confirmed. The posterior spinous processes should be centered in the midline and aligned with one another. The cortex of each vertebral body should be intact. The height of and spacing between adjacent vertebral bodies should be uniform.

Open-Mouth Odontoid X-ray
The open-mouth odontoid view ( Figures 3-15 and 3-16 ) is essential for evaluation of two important injury patterns:
- •
Burst fractures of the C1 ring, also called Jefferson fractures
- •
Fractures of the odontoid process or dens, which is a structure of C2


The open-mouth odontoid view is so called because it is obtained with the patient’s mouth opened as wide as possible, with the x-ray tube aimed into the open mouth. This gives a direct view of C1 and C2. Issues that may prevent adequate visualization include an obtunded or uncooperative patient who is unable to comply with this maneuver; a patient with trismus, temporomandibular joint disease, or other injuries (e.g., mandibular fractures) that prevent full opening of the mouth; and the presence of significant metal dental work. Sometimes, the cervical spine collar may restrict mouth opening too much to allow an adequate open-mouth odontoid view. When an adequate open-mouth odontoid view cannot be obtained, CT should be performed to avoid a missed injury of C1 or C2.
An adequate open-mouth odontoid view visualizes the entire dens and the lateral margins of both C1 and C2. A fully visualized dens is essential for evaluation of dens fractures. The cortex of the dens should be carefully inspected for defects. Shadows of overlying structures such as central incisors can simulate or hide fractures, so a wide-open view with no overlap of teeth with the dens is desirable. When the ring of C1 is intact, the lateral margins of C1 should align with the lateral margins of C2. When fractured, C1 typically “bursts,” with the fracture fragments spreading outward. Consequently, an indirect sign of C1 fracture is misalignment of the lateral margins of C1 with the lateral margins of C2. Frequently, the lateral margins of C1 appear displaced laterally compared with the lateral margins of C2, although medial displacement of C1 is also possible. This finding may be unilateral or bilateral. When C1 is intact and the patient is facing directly forward, the distance between the dens and the medial borders of the C1 ring should be bilaterally symmetrical. When C1 is fractured, displacement of fracture fragments typically renders this distance asymmetrical. The lateral margins of C1 and C2 may be hidden by radiopaque dental fillings, especially if the patient’s mouth is not fully opened.
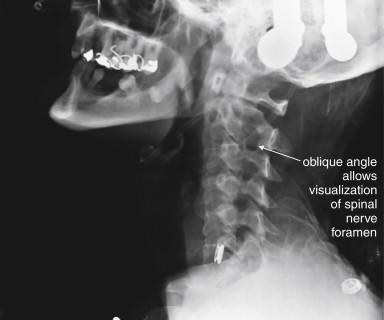
The standard three-view series just described is sometimes augmented with additional plain x-ray views. Adding two oblique views allows visualization of the pedicles, lamina, and neural foramina. Although this technique may be useful in selected cases, this “five-view” technique has been compared with the standard three views and does not detect additional injuries at a rate high enough to make five views a useful standard. The five-view series was insensitive (44%) compared with CT in a high-risk group of patients with altered mental status and a high rate of cervical spine injury (>10%). CT should be obtained if subtle lamina, pedicle, or neural foramen injuries are suspected.
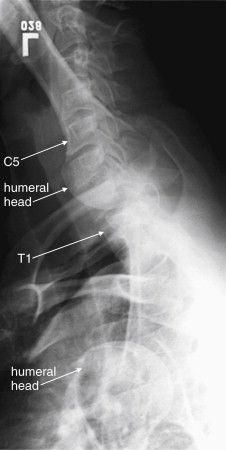
In cases in which the C7-T1 junction is not visualized on the lateral x-ray, “swimmer’s” ( Figure 3-17 ) or “traction” views may allow visualization of this region. In a swimmer’s view, the patient is positioned with the arm closer to the x-ray detector raised above the head. This elevates the humeral head above the C7-T1 junction, preventing it from obscuring this area. The opposite arm is held at the patient’s side, resulting in that humeral head lying somewhat lower that the C7-T1 junction. Variations on this theme include having the patient raise both arms directly in front of the body or over the head. In a traction view, a health care worker pulls on the patient’s arms from a position at the foot of the bed, distracting the humeral heads down to reveal the C7-T1 junction – a method now discouraged because of the possibility of worsening spinal injury. When these maneuvers do not allow adequate visualization of C7-T1, CT is indicated. In many cases, these views are skipped in favor of CT. Flexion and extension views ( Figure 3-18 ) are sometimes obtained to assess for ligamentous instability—the evidence for these views is discussed in detail later.

Computed Tomography of the Cervical Spine
CT scan evaluates for fractures and dislocations with high sensitivity and specificity. Soft-tissue injuries are demonstrated less directly and accurately ( Box 3-1 ). CT scan should be performed in several situations ( Box 3-2 ):
- •
As a follow-up to plain x-rays to further evaluate any fracture, dislocation, or soft-tissue abnormality on x-ray.
- •
As a follow-up study when adequate x-rays cannot be obtained. Examples include obese patients, obtunded or intoxicated patients, and patients with pre-existing spine disease.
- •
As the primary imaging study (rather than plain x-rays) when high pretest probability of cervical spine injury is present. It makes little sense to perform plain x-rays in this circumstance, because abnormal plain films would mandate CT and because normal plain films should be suspected of having missed cervical spine injury.
Interpreting Cervical Computed Tomography
Interpretation of cervical CT can be based on many of the same criteria used for plain x-ray. We make some direct comparisons of imaging findings on CT and x-ray, so skills you may already have from x-ray can be translated to CT. For those with little experience with either modality, starting with CT may prove easier, with CT findings then clarifying subtle findings on x-ray. We take a step-by-step approach, using the sagittal, coronal, and axial images for different purposes. Each image series should be reviewed, because fractures in the plane of a given image series are difficult to see in that series but are readily apparent in perpendicular planes. We spend relatively little time up front on normal findings; instead, we concentrate on pointing out abnormalities in the figures that follow, with comparison to normal findings.
CT has high resolution for bony injury and directly detects fractures and dislocations. Modern CT scanners allow multiplanar and three-dimensional reconstructions, facilitating injury characterization. Image data is helically acquired as the patient passes through the CT gantry, typically at 1-mm or submillimeter slice thickness. Reconstructions are performed in sagittal, coronal, and axial planes ( Table 3-2 ). The sagittal plane yields information similar to that from the lateral plain x-ray. The coronal plane yields information similar to that from the AP and odontoid plain x-ray views. Axial views give detailed anatomy of individual vertebral bodies, including clear views of the lamina, pedicles, transverse foramen enclosing the vertebral arteries, and spinal canal. Although the spinal cord is not well visualized on CT, the preceding image sets allow the canal to be carefully inspected for fracture fragments or dislocations that might impinge on the spinal cord. CT is considered to have outstanding sensitivity for fractures and dislocations—a normal CT viewed on bone windows effectively rules out these injuries. Nevertheless, it remains common practice to continue spine immobilization following a normal CT if the patient cannot be clinically evaluated for neurologic complaints or continued pain, though recent studies suggest a low risk of unstable cervical injuries following normal CT (see later discussion).
| Abnormality | Sagittal Images | Coronal Images | Axial Images |
|---|---|---|---|
| Three-column stability | Yes | No | Yes |
| AP subluxation | Yes | No | No |
| Lateral subluxation | No | Yes | No |
| Loss of vertebral body height | Yes | Yes | No |
| Loss of disc height | Yes | Yes | No |
| Burst injury | Yes | Yes | Yes |
| Nondisplaced fractures | Yes, if not in sagittal plane | Yes, if not in coronal plane | Yes, if not in axial plane |
| Retropulsion of fragments into spinal canal | Yes | No | Yes |
Step 1: Examine the Sagittal Computed Tomography Reconstructions
The sagittal CT reconstructions provide detailed information about the AP alignment of the cervical spine, as well as fractures or subluxations that may impinge on the spinal canal. Start your evaluation by selecting bone windows, and then move to a slice in the middle of the sagittal series, corresponding to the midsagittal plane ( Figure 3-19 ). If you are experienced in interpreting cervical spine x-rays, this image should look familiar—it strongly resembles the lateral cervical spine x-ray, without the confusing overlay of bones and soft tissues from other planes. Just as with the lateral x-ray view, the midsagittal CT image allows assessment of alignment, using the curves of the anterior and posterior longitudinal ligaments and the spinolaminar line. In this view, the spinal canal can be seen in detail and inspected for any fracture fragments or subluxation of vertebral bodies that could impinge on the spinal cord. Remember that you are only looking at a single plane—you need to scroll laterally to the patient’s right and then left to perform these same steps in planes moving away from the patient’s midline. In the midsagittal plane, notice how large the dens is—perhaps you did not appreciate this on x-ray, but look now at the lateral x-ray for comparison. Check the contour of the dens for fracture lines, and if fracture is present, inspect for retropulsion of the dens into the spinal canal. Inspect the predental space for widening. Look at prevertebral soft tissues for increased thickness suggesting soft-tissue injury. Inspect each vertebral body for fracture lines. Check the spinal lamina and posterior spinous processes for fracture. Notice that in the midsagittal plane, the facet joints are not visible. These are lateral structures and are seen in the far lateral parasagittal images ( Figure 3-20 ). Inspect these joints for unilateral or bilateral dislocation (jumped facets, shown in a later figure). At the cephalad limit of the cervical spine, inspect the articulation of the occipital condyles with C1 (see Figure 3-20 ). It may take you some time to become accustomed to imagining the cervical spine in three dimensions as you scroll through it in this plane.


Step 2: Inspect the Coronal Images
Use the coronal CT images ( Figure 3-21 ) to simulate the open-mouth odontoid and AP cervical x-rays. Scroll through the “stack” of coronal images until you see the odontoid process projecting between the lateral masses of C1. Check for the same features you would expect on the open-mouth odontoid view. The lateral masses of C1 and C2 should align along their lateral borders. The spaces between the odontoid process and the lateral masses of C1 should be symmetrical. The odontoid process itself should have a smooth contour, with no fracture lines present. Once you have completed this evaluation, scroll in anterior and posterior directions through the stack of images, inspecting for fractures of the vertebral bodies, facets, and transverse processes. Fractures in the sagittal plane are visible on coronal images, and may be missed on the sagittal images reviewed first. Look for lateral displacement of vertebral bodies with respect to one another. Spend some time reviewing the figures in this chapter to familiarize yourself with the most common fracture patterns.

Step 3: Inspect the Axial Computed Tomography Images
The axial CT images ( Figure 3-22 ) have no immediate analogue in the normal three-view x-ray series. They can provide additional information not readily seen on the sagittal and coronal views. Particularly, they demonstrate fractures of the canals housing the vertebral arteries (foramen transversarium), which are more difficult to assess on other views. They also provide good views of fractures in the sagittal and coronal planes, which may not be seen well on those image series as they lie parallel to the plane of the image. From the sagittal images, you should already have a good idea of the alignment of the cervical spine, although the axial images can also demonstrate jumped facet joints. The axial images provide an en face view of the spinal canal. As you scroll from the level of C1 to T1, imagine yourself traveling down the spinal canal, and watch for fracture fragments that narrow the canal and may impinge on the spinal cord. Check the body, pedicles, lamina, and transverse and posterior spinous processes for fractures. We review many abnormal findings on the axial images in the figures throughout this chapter (see list, Table 3-1 ).

Clinical Decision Rules: Who Needs Cervical Spine Imaging?
Indications for cervical spine imaging have been studied extensively, resulting in two well-validated clinical decision rules (CDRs) to aid the clinician in identifying patients who require cervical spine imaging. We review both rules in detail, discussing their strengths and weaknesses.
The National Emergency X-radiography Utilization Study
The National Emergency X-radiography Utilization Study (NEXUS) was a prospective study of 34,069 patients at 21 U.S. medical centers, examining blunt trauma patients undergoing cervical spine imaging ( Box 3-3 ). This study was well planned and conducted and identified 818 patients with cervical spine injuries, comprising 2.4% of the study population. The study evaluated a CDR consisting of five clinical criteria, which had been suggested by prior studies ( Box 3-4 ). Cervical spine imaging was considered necessary if any one of the five was present. The investigators prospectively defined a group of clinical unimportant cervical spine injuries which they did not expect their proposed rule to identify, as they would not be anticipated to lead to patient harm if undetected. This rule proved 99% sensitive, though only 12.9% specific for clinically important acute cervical spine fracture. The negative predictive value of the rule was 99.8%, with a positive predictive value of only 2.7%. Application of the rule would have reduced cervical spine imaging by 12.6%. The rule failed to identify 8 of 818 injuries—2 which would have been clinically significant, 1 of which was treated surgically. Application of this rule is estimated to miss one injury in 125 years of clinical practice by a typical emergency physician.
The Canadian Cervical Spine Rule
The Canadian Cervical Spine Rule (CCR) ( Figure 3-23 ) is a classic example of a methodologically rigorous CDR. CDRs are aids to bedside decision making, intended to reduce the cost, time, and adverse consequences of care, such as radiation exposures from diagnostic imaging. CDRs must be rapid to apply, inexpensive, and sensitive to avoid missing important pathology. They must be specific enough to reduce subsequent test utilization; otherwise, they fail their primary objective. Typically, CDRs use readily available information from the history and physical examination, occasionally supplemented by simple, rapid, and inexpensive bedside tests such as urinalysis.