Emergency conditions of the genitourinary tract include the life threatening, such as ruptured ectopic pregnancy and renal avulsion, and threats to organ function, such as testicular and ovarian torsion. The diversity of potential clinical scenarios and differential diagnoses means that our discussion is best presented in the context of the chief complaint or specific pathologic entities, rather than in a single algorithm to evaluate the entire genitourinary tract. We begin with nontraumatic urinary tract conditions. Next, we address conditions of the male and female reproductive organs, including conditions in the pregnant patient. Finally, we discuss imaging of genitourinary trauma.
Clinical Presentations and Differential Diagnosis
A variety of chief complaints may suggest genitourinary pathology. In some cases, no imaging is required. In other cases (such as back pain with suspected aortic aneurysm or renal colic), the nongenitourinary differential diagnosis is most important and drives imaging decisions. In still others, a targeted genitourinary differential requires emergency imaging. Table 12-1 outlines chief complaints, selected differential diagnoses, and appropriate imaging modalities.
| Chief Complaint | Differential Diagnosis | Imaging Modalities |
|---|---|---|
| Nontraumatic Urinary Complaints | ||
| Flank pain with or without abdominal pain |
|
|
| Painless hematuria |
|
|
| Dysuria |
|
|
| Urinary retention |
|
|
| Abdominal pain |
|
|
| Fever |
|
|
| Perineal pain |
|
|
| Male Genitourinary | ||
| Testicular or scrotal pain |
|
|
| Testicular or scrotal mass |
|
|
| Urethral discharge |
|
|
| Prostatic pain or suspected prostatic hypertrophy |
|
|
| Female Genitourinary | ||
| Pregnant Patient | ||
| Vaginal bleeding |
|
|
| Abdominal or pelvic pain |
|
|
| Fluid leak or vaginal discharge |
|
|
| Recently Pregnant Patient | ||
| Abdominal pain, vaginal bleeding or discharge, or fever |
|
|
| Nonpregnant Patient | ||
| Vaginal bleeding |
|
|
| Abdominal or pelvic pain |
|
|
| Vaginal discharge |
|
|
| Trauma | ||
| Blunt abdominal or torso trauma |
|
|
| Traumatic hematuria (gross) ∗ |
|
|
| Traumatic vaginal bleeding |
|
|
| Direct genitourinary trauma |
|
|
| Abdominal or pelvic trauma in the pregnant patient |
|
|
| Penetrating abdominal or torso trauma |
|
|
∗ Microscopic hematuria generally does not require imaging in adults but does require it in pediatric patients.
Imaging Nontraumatic Genitourinary Complaints
Abdominal or Flank Pain With or Without Hematuria
Abdominal and flank pain with or without hematuria can suggest renal colic or pyelonephritis, although an array of other conditions can present with similar symptoms. Conditions such as abdominal aortic aneurysm (AAA), renal cell carcinoma, renal infarction, and perinephric abscess can cause flank and abdominal pain with hematuria. A variety of imaging options are available for evaluation of these signs and symptoms. The choice of imaging study should reflect the differential diagnosis under consideration, the clinical certainty of the diagnosis, radiation exposure concerns, contrast nephrotoxicity or allergy, time, and cost. In some cases, particularly in patients with recurrent urolithiasis, the diagnosis is virtually certain and no imaging may be required. Moreover, in patients with recent prior imaging, other diagnostic concerns such as AAA can often be ruled out based on measurements made from existing images. Later, we discuss the imaging options with strengths and weaknesses of each. Noncontrast computed tomography (CT), CT with intravenous (IV) contrast, CT with IV and oral contrast, IV urography (IVU), x-ray, renal ultrasound, and rare tests such as Lasix renal scan all have roles in the evaluation of potential renal colic.
To select the best imaging test, the emergency physician should generate a differential diagnosis that is comprehensive yet tailored to the patient. If the differential diagnosis seriously includes entities other than renal colic, CT is likely the best test. If vascular abnormalities are considered, CT with IV contrast is useful, assuming the patient is stable and has an acceptable creatinine (because of concerns about nephrotoxicity of IV contrast). When the differential diagnosis is particularly broad, including renal, reproductive, vascular, bowel, and other abdominal pathology, CT with IV and oral contrast provides the most information. The decision to perform immediate noncontrast CT, CT with IV contrast, or oral and IV–contrasted CT should be based on the most dangerous pathology suspected. In young patients, in whom vascular disasters such as AAA are rare, radiation concerns may outweigh the impetus for rapid imaging. In these patients, the delay for oral contrast may be acceptable to avoid repeated radiation exposure if noncontrast CT were negative. In older patients with concern for vascular catastrophes, immediate CT without any contrast may be wise, with enhanced CT performed later if more information is needed. The danger of repeated radiation exposure in patients over the age of 50 pales in comparison with the risk for delayed diagnosis of AAA rupture. Vascular catastrophes are discussed in more detail in Chapter 11 . If urolithiasis is the only suspected diagnosis, IVU can be performed. In pregnant patients, renal ultrasound can be used to assess for obstruction complicating urolithiasis, avoiding radiation exposure. This strategy may also be useful in patients of either gender with recurrent episodes of renal colic to avoid high cumulative radiation exposures from CT. Figure 12-1 shows an algorithm for CT imaging in acute flank and abdominal pain. Table 12-2 lists the information provided by the various imaging modalities, along with cost, time, and radiation information. We begin with a discussion of CT scan, followed by descriptions of other imaging modalities.

| Modality | Information Provided | Radiation Dose | Contrast | Approximate Cost | Time |
|---|---|---|---|---|---|
| CT |
| 4-10 mSv | No | $750-$1000 | Less than 5 minutes to perform, 30 minutes for interpretation |
| CT with IV contrast |
| 4-10 mSv | Yes | $750-$1000 | Less than 5 minutes, after delay to measure creatinine |
| CT with IV and oral contrast |
| 4-10 mSv | Yes | $750-$1000 | Less than 5 minutes, after delay of approximately 2 hours to ingest oral contrast |
| IVU |
| 1.5 mSv | Yes | $350 | Approximately 75 minutes |
| X-ray |
| 0.5-1 mSv | No | $250 | Less than 5 minutes |
| Ultrasound |
| No | No | $150 | Approximately 15-30 minutes—bedside ultrasound is quicker |
Imaging Options for Suspected Renal Colic
Computed Tomography Scan
CT scan ( Figures 12-2 to 12-15 ) is sensitive for many types of spontaneous disease of the kidneys, ureters, and bladder, including renal tumors and urolithiasis. It is less helpful in delineating disease such as transitional cell carcinoma within the ureters or bladder. For suspected renal colic, no IV or oral contrast is needed. A calcified stone within the kidney, ureters, or bladder usually is evident as a high-density (white) lesion on abdominal windows (see Figures 12-2 to 12-6 ). These lesions are easily seen without contrast because few other white structures should be present in the vicinity of the kidneys, ureters, or bladder. Calcified phleboliths in the pelvis may occasionally be confused with intraureteral stones.














Noncontrast CT has become a test of choice because it can be performed immediately and provides several key pieces of information:
- •
Acute abdominal pathology outside of the urinary tract, such as ruptured AAA, appendicitis, bowel obstruction, and free air. Studies suggest that between 4% and 10% of CT scans performed for evaluation of suspected renal colic demonstrate alternative or additional diagnoses.
- •
Presence of stones within the entire urinary tract, from kidneys to urethra.
- •
Size and location of urinary stones, information that is useful in predicting chance of spontaneous stone passage or need for urologic intervention.
- •
Presence of hydronephrosis or hydroureter resulting from an obstructing stone (see Figures 12-7 to 12-9 ).
- •
Additional stone burden within the kidney, which may predict future symptomatic urolithiasis. Stones currently in the kidney are rarely thought to cause symptoms, except in the case of staghorn calculi (see Figures 12-5 and 12-6 ).
Compared with IV urography, CT is also advantageous because it does not require contrast administration, which can cause nephrotoxicity in patients with already obstructed urinary systems. In addition, IVU does not routinely reveal nonurinary pathology. Studies comparing emergency department length of stay show an advantage to CT over IVU, the traditional standard.
Is Intravenous or Oral Contrast Needed for Detection of Stones? Does Contrast Interfere With the Diagnosis of Urinary Stones?
For detection of intrarenal and intraureteral stones, no contrast of any form is needed. Administration of oral and IV contrast can interfere with diagnosis of urologic stone disease; for this reason, noncontrast CT is often performed immediately before an IV-contrasted study. This also allows comparison of the noncontrast and contrasted CT for identification of lesions that enhance with IV contrast. The addition of contrast makes identification of stones more difficult by providing an array of white (contrast-filled) structures among which a white urolith must be sought. The kidneys enhance intensely after administration of IV contrast, so stones within the kidneys may be difficult or impossible to discern. Soon after IV contrast is administered, contrast is filtered and excreted by the kidneys and begins to fill the ureters, again potentially disguising stones within the ureters (see Figures 12-8 and 12-9 ). In cases of suspected high-grade obstruction, additional delayed images of the kidneys and ureters can be performed following IV contrast administration to assess for normal filling of the ureters, or pathologic nonfilling. This information is similar to that obtained from a standard intravenous pyelography (IVP) using conventional radiography. Oral contrast agents are not needed to detect urologic stone disease. Some CT protocols place the patient in a prone position, rather than the supine position commonly used for abdominal CT. This position leaves bowel and other intraabdominal organs in a dependent position, whereas ureters and kidneys are held tightly in their retroperitoneal position. Calcifications in the ureters may be more easily discriminated from nonurinary calcifications by this technique.
When Should Noncontrast CT Be Performed? When Should Noncontrast CT Be Followed by Contrasted CT?
This is a clinical decision, and it should be driven by the differential diagnosis. Several factors warrant consideration. First, is a life-threatening diagnosis, such as ruptured AAA or aortic dissection, under serious consideration? If so, immediate CT should be considered, perhaps without any contrast agents, depending on the stability of the patient (bedside ultrasound and surgery consultation may be appropriate in an unstable patient). AAA can be diagnosed without any contrast agents, whereas aortic dissection requires IV contrast for diagnosis. Second, is the patient old enough that the radiation exposure from multiple CT scans is not an important consideration? In patients older than 50 years, the radiation exposure from CT is unlikely to cause a clinically important cancer, and rapid diagnosis of an immediate life threat such as AAA easily trumps radiation risk. In younger patients, especially those in whom an imminent life threat is not suspected, it may be more reasonable to perform a single CT scan with IV and oral contrast to maximize the possibility of detecting nongenitourinary pathology. This strategy may be more beneficial to the patient in the long run than scanning without contrast and then scanning with contrast if no pathology is detected. At the same time, studies suggest that CT without contrast has good sensitivity for many conditions traditionally examined with contrast, including appendicitis. These studies are discussed in more detail in Chapter 9 , Imaging of Nontraumatic Abdominal Conditions. Depending on the specific differential diagnosis being considered, noncontrast CT may be the only imaging needed—for example, contrasted CT may not be required if the appendix is well visualized on noncontrast CT. An additional factor to be considered is the patient’s renal function and allergies—IV-contrasted CT should be avoided in patients with renal insufficiency or dye allergies, and noncontrast CT may be adequate to evaluate fully the differential diagnosis under consideration. Noncontrast CT generally is not performed after contrasted CT because orally administered agents may remain present for a day or more and IV contrast agents are visible for minutes to hours (in the case of urinary obstruction) within the renal collecting system, ureters, and bladder as they are excreted.
Besides the Presence of Stones, What Genitourinary Abnormalities Can Noncontrast CT Identify? What Genitourinary Abnormalities Can Be Seen With the Addition of IV Contrast?
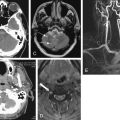
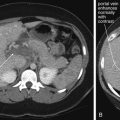
Noncontrast CT can reveal the presence of ureteral obstruction. Hydronephrosis is recognized by the presence of a dilated renal collecting system. The unobstructed contralateral side serves as a useful comparison (see Figures 12-7 to 12-9 ). Variation in size of the proximal ureter can occur because of the presence of a normal variant extrarenal pelvis, which can simulate significant proximal hydroureter. Hydroureter (see Figures 12-7 to 12-9 ) proximal to an obstructing stone can be detected on noncontrast CT. The upper limit of normal diameter for an unobstructed ureter is 3 mm. Stranding of perirenal fat (see Figures 12-8 and 12-11 ) can be seen without any contrast agents and can occur in the setting of obstruction or infection. Stranding is caused by lymphatic capillary leak, resulting in infiltration of fluid into the perirenal fat. This increases the density of the perirenal fat relative to normal fat. Increased density on CT results in a whiter appearance, compared with the usual dark gray appearance of fat. This finding may also occur in pyelonephritis, so the urinalysis should be examined for infection. Importantly, stranding alone does not indicate infection, unless other clinical indicators of infection (such as a positive urinalysis) are present. Emphysematous pyelonephritis (see Figure 12-10 ) can be observed on noncontrast CT because air appears black and does not require contrast for visualization. Perinephric abscess (see Figure 12-11 ) can be seen as a low-density (dark gray) fluid collection adjacent to the kidney, often with stranding. Addition of IV contrast enhances an abscess. Urine collections (urinomas) surrounding a kidney because of a leaking renal pelvis or ureter have a similar appearance to abscess on noncontrast CT but may lack stranding and do not enhance with IV contrast. Isolated simple renal cysts (see Figure 12-12 ) are visible on noncontrast CT. These structures have a low Hounsfield unit density near zero because they contain fluid similar in density to water. The surrounding renal parenchyma is slightly denser and thus slightly brighter without contrast. When IV contrast is administered, renal cysts become more conspicuous because the surrounding normal kidney enhances dramatically but cysts do not. Solitary simple cysts are not usually diagnostically important because they are not typically a cause of acute pain. Polycystic kidneys may be the cause of acute or chronic pain and are readily seen on noncontrast CT. Unilateral, horseshoe, or pelvic kidneys are recognized on noncontrast CT, though these are not associated with acute abdominal or flank pain. Solid renal tumors such as renal cell carcinoma (see Figures 12-13 and 12-14 ) can be difficult to identify on noncontrast CT when small. They may be exophytic and can invade adjacent structures (see Figure 7-56 ). Addition of IV contrast helps in detection of small lesions by allowing enhancement. Renal infarction is not easily identified on noncontrast CT but is readily apparent with IV contrast, as the infarcted region fails to enhance while normal renal parenchyma vividly enhances (see Figure 12-15 ). Retroperitoneal hemorrhage ( Figure 12-16 ), whether spontaneous or resulting from trauma, can be seen on noncontrast CT. Addition of IV contrast is important in these cases as it can reveal active bleeding.

IV contrast results in intense enhancement of the normal kidney because of the enormous blood flow to this organ. An abnormal kidney may fail to enhance compared with the normal kidney. Examples include aortic dissection (see Figure 7-83 ) or renal artery dissection. In addition, hypoperfused renal segments may not enhance normally. Examples include renal infarcts in the context of atrial fibrillation (see Figure 12-15 ). Hypoperfusion of renal segments also is seen in some cases of pyelonephritis, although no clinical significance is known and contrasted CT is not recommended for this diagnosis. As mentioned earlier, renal abscesses with rim enhancement may also be demonstrated on CT with IV contrast, though noncontrast CT or ultrasound may show a fluid collection around the kidney (see Figure 12-11 ). Perirenal fluid collections may also indicate urinomas because of a leaking urinary tract—these do not demonstrate rim enhancement with the addition of IV contrast and can be seen on noncontrast CT. Renal masses such as renal cell carcinoma (hypernephroma; see Figures 12-13 and 12-14 ) are also detected as enhancing masses on contrasted CT (these lesions may be detected, though not as perfectly delineated, on noncontrast CT). Exophytic bladder lesions such as transitional cell carcinomas may become visible as IV contrast excreted by the kidneys fills the bladder. The tumor mass may be visible as a void or filling defect in the contrast-filled bladder. Clot may have a similar effect and appearance. Dense contrast settles in the dependent portion of the bladder. As a consequence, if the bladder is not completely filled with contrast, lesions in the nondependent portion of the bladder may not be visible.
How Sensitive Is Noncontrast CT for Renal Stones?
CT is highly sensitive for most calcified ureteral stones. Its sensitivity and specificity approach 100%, with better positive and negative likelihood ratios than IVU. In some cases, no stone is seen because the patient passed the stone just before CT scan. Stones formed from indinavir, a poorly soluble protease inhibitor used in the treatment of human immunodeficiency virus infection, are not visible on CT because they are isodense with urine. However, findings of obstruction from these stones, such as hydroureter and hydronephrosis, are still readily recognized on CT. These stones can be seen by modalities such as ultrasound, and on IVU they create an obstruction picture identical to that seen with other stones.
What Is the Prognostic Value of CT for Renal Stones? What Size of Stone Will Pass? How Quickly can Stones Develop? What If the Patient Had a Scan Without Stones 1 Week Ago?
Stone size as measured on CT scan is predictive of the rate of spontaneous passage or need for surgical or procedural intervention. Only 2.2% of patients with stones smaller than 6 mm require a procedure, whereas 80% of patients with stones of at least 6 mm require a procedure. The rapidity with which stones can develop is not well studied, but in general, the absence of stones on recent CT imaging likely indicates that a large obstructing stone is unlikely.
Ultrasound
Ultrasound is a valuable tool for the assessment of obstruction of the ureters. Ultrasound has the advantage of being noninvasive, with no radiation exposure and no need for IV contrast. It is relatively inexpensive compared with CT and can be repeated over time without harm to the patient. Ultrasound is portable, and it can be used to assess for important alternative causes of symptoms, from aortic aneurysm to appendicitis to complications of pregnancy. It is the standard test for suspected renal colic in the pregnant patient because it does not expose the fetus to ionizing radiation. Renal ultrasound assesses for hydronephrosis and hydroureter ( Figures 12-17 and 12-18 ). It is limited to some extent by body habitus and operator experience, and it does not always allow visualization of the cause of the obstruction, whether that is an intraureteral stone or extrinsic compression of the ureter by a mass or retroperitoneal fibrosis. On ultrasound, calcified renal stones are hyperechoic (bright white) (see Figure 12-17 ), reflecting the ultrasound beam and preventing its transmission deep to the stone. As a consequence, they also create an acoustic shadow deep to the stone. Ultrasound can be used to detect other renal disease including atrophic kidneys, renal cysts including polycystic kidney disease, and renal masses. With the addition of Doppler ultrasound, flow in the renal arteries and renal artery stenosis can be diagnosed.


Studies comparing ultrasound and CT for the diagnosis of ureterolithiasis show comparable sensitivity and specificity (91% and 95%, respectively, for CT and 93% and 95%, respectively, for ultrasound). Some studies have shown lower sensitivity of ultrasound (61%) compared with CT (96%). Overall, ultrasound is a reasonable alternative to CT when the differential diagnosis is limited to ureteral stones and radiation reduction is a priority, as in pregnancy or young patients with multiple episodes of renal colic.
Plain Film X-ray
Plain film x-ray plays a limited role in evaluation of nontraumatic urologic emergencies. In the setting of suspected renal colic, a single plain film of the abdomen was commonly performed before the era of CT. This x-ray is often called a KUB (for kidneys, ureters, bladder)—ironically, because none of these structures is usually visible, though they may be included in the field of view. X-ray is likely insensitive for detection of renal stones: 18.6% in one study compared with a gold standard of unenhanced CT. The specificity is high, around 95%. This method may have some limited value when other imaging techniques are unavailable. It can demonstrate likely ureteroliths, although it may fail to detect noncalcified stones. In addition, extraurinary calcifications such as phleboliths may be misidentified as urinary stones ( Figures 12-19 and 12-20 A ). Although the size of the stones may be measured, plain film does not allow assessment for obstruction. In addition, sensitivity for a broader differential diagnosis, including aortic aneurysm, appendicitis, and bowel obstruction, is quite limited. Perhaps the greatest benefit of a single plain film in this setting is that the radiation exposure to the patient is low—though the information gleaned from the study is so limited that no imaging is nearly as useful. Sometimes a single x-ray to evaluate for radiodense stones is combined with ultrasound to evaluate for hydronephrosis and hydroureter. When a stone has been visualized on a prior x-ray, x-ray can be used to monitor its progression. X-ray is also used to assess the position of medical devices such as ureteral stents.


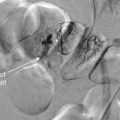
Intravenous Urography
IVU (also called IVP) is a series of plain film images taken over time (see Figure 12-20 ). In addition to providing information about the structure of the urinary system, including the presence of stones or obstruction, this is a “functional study,” because it provides a view of renal excretion of injected contrast. First, a plain film image of the abdomen and pelvis is obtained, before the administration of contrast. This image can be examined for radiopaque stones and medical devices such as ureteral stents, as described earlier. Occasionally, an alternative diagnosis such as appendicitis or AAA may be recognized, although this modality should never be relied on to exclude these diagnoses because it is insensitive. Next, around 50 mL of iodinated contrast is injected intravenously, and the plain film (KUB) is repeated after a delay of 5 minutes. Additional images are repeated at approximately 15-minute intervals until both kidneys have been observed to fill and then empty of contrast, allowing excretion of the contrast material to be observed over time. Depending on the speed of excretion, the examination usually takes less than 1 hour, though several hours may be required in cases of severe obstruction. A normal IVU demonstrates rapid and symmetrical enhancement of both kidneys, followed by complete filling of the ureters and bladder. Several abnormalities may be observed. First, congenital anomalies may be observed, including duplications of the collecting system, and unilateral, horseshoe, or abnormally positioned (e.g., pelvic) kidneys. In the setting of ureteral obstruction from any cause, the kidney on the affected side may show delayed enhancement and delayed emptying, called a “delayed nephrogram” (see Figure 12-20 E ). This is because of diminished renal filtration and excretion of contrast in the setting of obstruction. In addition, the affected ureter may fail to fill with contrast beyond the point of a complete obstruction, or the contrast may appear less intense beyond the point of a partial obstruction. IVU provides anatomic and functional information about the location and degree of obstruction, which may be important for planning urologic intervention.
Is Intravenous Urography Preferable to CT for Evaluation of Renal Colic or Ureteral Obstruction?
IVU and CT provide similar but not identical information. CT is superior in delineating a range of emergency alternative diagnoses, explaining its rapid incorporation into the imaging algorithm for suspected renal colic in the United States. CT also has the advantage of not requiring the administration of any contrast material, with the obvious benefit of not posing a threat of contrast nephropathy or dye allergy. In addition, CT can be performed immediately and diagnostic results are available within minutes, in comparison to IVU, which takes around 1 hour in most cases and longer in cases of severe obstruction. A number of studies have compared the time, expense, and radiation exposure of CT and IVU. CT generally results in slightly shorter emergency department length of stay, similar costs (depending on whether institutional or patient costs are compared), and somewhat higher radiation exposure, though new protocols have reduced radiation exposures.
Lasix Nuclear Medicine Scan: An Alternative Test for Ureteral Obstruction
A patient with recurrent renal calculi may develop an appearance of chronic obstruction with a dilated renal pelvis and ureter by ultrasound, CT scan, or IVP. A Lasix nuclear medicine scan ( Figures 12-21 and 12-22 ) can discriminate obstruction from a flaccidly dilated but currently unobstructed collecting system. Though rarely used in the emergency department, this test may be requested by a urologic consultant. In this test, a radiopharmaceutical, technetium-99m mercaptoacetyltriglycine, is administered intravenously. Dynamic blood flow phase images of the kidneys are obtained during bolus injection of the radiotracer. Sequential 2-minute acquisitions posteriorly over the abdomen are obtained through 30 to 60 minutes, allowing generation of graphs of radioactivity over time for the renal cortex and entire kidney. Lasix (50 mg IV) is administered after around 20 minutes. In a normal scan, rapid uniform excretion occurs after administration of Lasix. This is consistent with a flaccid but unobstructed collecting system. Lack of excretion of the tracer following Lasix administration suggests obstruction.


Is Any Imaging Needed for Suspected Renal Colic?
When a broad differential diagnosis is being considered, nongenitourinary diagnoses may drive the imaging strategy. Important diagnoses such as suspected AAA rupture or appendicitis may require CT or other imaging for diagnosis. In effect, though CT may confirm urolithiasis, the most important function of CT may be to exclude other diagnoses. When renal colic is the only serious diagnosis under consideration, the emergency physician should carefully consider whether any imaging is required. CT carries a moderately high radiation exposure, and patients with renal colic often have recurrent symptoms, resulting in multiple CT exposures over time. When complications such as infection or renal insufficiency are not present, deferring CT imaging may be reasonable. In first-time episodes of suspected renal colic, clinical judgment is incorrect in as many as 20% of cases, even when suspicion of stone is 90% or greater. Imaging of first episodes is likely warranted. Alternative or additional diagnoses are reported in approximately 10% of patients undergoing CT for suspected renal colic, although not all of these diagnoses require specific emergency treatment. In patients with recurrent symptoms, another reasonable strategy may be ultrasound to evaluate for hydronephrosis or hydroureter. Ultrasound may show a stone, though with lower sensitivity than CT. In patients older than 50 years, the risk of repeat CT radiation exposures may be relatively unimportant, and the risk of alternative causes of symptoms rises. CT may be a prudent strategy in this age group.
Painless Hematuria
Painless hematuria generally is not associated with urolithiasis because the latter condition is usually painful. Painless hematuria can indicate urinary infection, renal infarction, systemic illness such as glomerulonephritis or thrombocytopenia, or masses of the genitourinary tract, including renal cell carcinoma (see Figures 12-13 and 12-14 ) and transitional cell carcinoma of the ureters or bladder. Painless hematuria is an important complaint for this reason, but emergency imaging is only required in selected cases, depending on the specific differential diagnosis being entertained. For example, in the patient with atrial fibrillation, renal infarction (see Figure 12-15 ) should be considered. Imaging can alter patient management because confirmation of renal infarction can suggest a cardiac embolic source. When important but less urgent pathology such as renal mass is suspected, imaging can be deferred to an outpatient setting. Patients with poor follow-up may benefit from definitive imaging in the emergency department to allow appropriate referral. When the decision is made to perform imaging, CT without IV contrast followed by CT with IV contrast is most useful because it identifies enhancing renal masses such as renal cell carcinoma. CT with IV contrast can also demonstrate areas of abnormal renal parenchymal enhancement consistent with infarction. Noncontrast CT alone may fail to fully delineate these lesions. Oral contrast is not needed for these indications. CT scan does not evaluate intraluminal pathology of the bladder or ureters well, so additional follow-up for cystoscopy is indicated if transitional cell carcinoma is suspected. Exophytic bladder lesions such as transitional cell carcinomas may become visible as IV contrast excreted by the kidneys fills the bladder. Delayed CT images are often acquired to allow detection of such pathology. The tumor mass may be visible as a void or filling defect in the contrast-filled bladder. Clotted blood within the bladder may have a similar effect and appearance and may sometimes confuse the diagnosis. Renally excreted contrast within the ureters on CT or IVP may occasionally show a filling defect suggesting a ureteral mass.
Dysuria
Isolated dysuria can suggest urinary tract infection, infectious urethritis, or sterile urethritis such as Reiter’s syndrome. This symptom generally does not require emergency imaging.
Urinary Retention
Obstruction of the bladder outlet and inability to urinate is a common emergency department complaint, particularly in men. Usual causes are benign prostatic hypertrophy and hematuria with clot formation leading to urethral obstruction. Ureteral obstruction rarely causes urine retention because bilateral ureteral obstruction would be required. Retroperitoneal causes such as retroperitoneal fibrosis or tumors may occasionally obstruct both ureters. Urinary retention from a neurologic cause should be considered, but in the absence of other neurologic signs or symptoms, back pain, or other red flags for spinal pathology, mechanical bladder outlet or urethral obstruction is the most common cause. Prostatic malignancies and bladder masses may also lead to obstruction, but emergency imaging is not generally required when symptoms are relieved by placement of a urinary catheter. Urologic follow-up is necessary. If a neurologic cause is suspected, spine magnetic resonance imaging (MRI) is usually required. Ultrasound of the bladder can be performed at bedside and reveals a full bladder in cases of urethral obstruction or neurogenic bladder. Renal ultrasound commonly reveals bilateral hydronephrosis but is not necessary if the obstruction is relieved by urinary catheter placement.
Nontraumatic Abdominal Pain
Nontraumatic abdominal pain can result from a host of serious and benign conditions. The chapters on abdominal imaging explore this in detail. Some causes of abdominal pain include genitourinary abnormalities, as described later in the sections on male and female genitourinary complaints. Flank pain with or without abdominal pain was discussed earlier.
Fever
Isolated fever without other genitourinary signs or symptoms rarely requires genitourinary imaging. Fever associated with abdominal, flank, or pelvic pain requires imaging as indicated for the evaluation of the associated pain. Serious genitourinary infections such as tuboovarian abscess, perinephric abscess (see Figure 12-11 ), or Fournier’s gangrene ( Figures 12-23 and 12-24 ), described in the next section, may have associated fever but are usually accompanied by localizing pain and examination findings that direct imaging. One exception is the obtunded septic patient with fever. Complicated urinary infections such as perinephric abscess and infected obstructing ureteral stone should be considered and may require imaging.