In Situ Thrombosis
In 1860, Virchow postulated that thrombus can form as a result of vessel injury, disturbance of blood flow and hypercoagulability. A spectrum of diseases can be associated with one or all three of these precipitating factors, with the aftereffect of in situ thrombosis in the pulmonary vasculature. The criteria for in situ thrombus include (1) the presence of thrombus at the site of vessel injury and/or site of disturbance of blood flow and (2) the absence of other pulmonary vessel thrombi remote from the site of vessel abnormality. This chapter illustrates examples of in situ thrombosis of the pulmonary arteries and veins.
 Tumor-Related Pulmonary Artery Thrombosis
Tumor-Related Pulmonary Artery Thrombosis
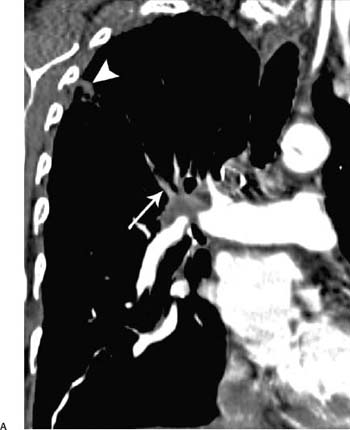
 In patients who have lung cancer, all three factors may be present: vessel injury from local tumor invasion, disturbance of blood flow, and hypercoagulability (Fig. 5.1).
In patients who have lung cancer, all three factors may be present: vessel injury from local tumor invasion, disturbance of blood flow, and hypercoagulability (Fig. 5.1).
 The differentiation between direct tumor growth along a vessel lumen and in situ thrombosis may be impossible based on imaging at one time point. Pathologically, the two often coexist.
The differentiation between direct tumor growth along a vessel lumen and in situ thrombosis may be impossible based on imaging at one time point. Pathologically, the two often coexist.
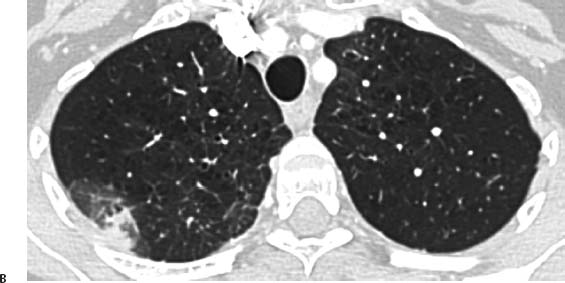
Fig. 5.1 (A,B) Peripheral infarction in a 71-year-old man with central adenocarcinoma of the lung. (A) Coronal reconstruction CT demonstrates the primary lung neoplasm invading the right pulmonary artery and a filling defect within the posterior segmental artery of the right upper lobe (arrow). There is also a peripheral pulmonary opacity (arrowhead). Peripheral infarction in a 71-year-old man with central adenocarcinoma of the lung. (B) On axial CT, this opacity has almost a wedge-shaped configuration, consistent with peripheral infarction.
 Radiotherapy-Related Pulmonary Artery Thrombosis
Radiotherapy-Related Pulmonary Artery Thrombosis
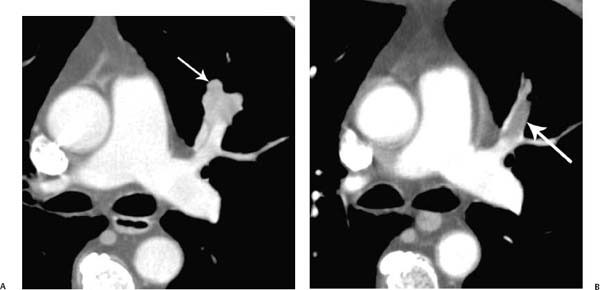
 The early effects of radiation on endothelial cells are characterized by swelling and sloughing.
The early effects of radiation on endothelial cells are characterized by swelling and sloughing.
 Such vessel-wall injury can lead to in situ thrombosis (Fig. 5.2).
Such vessel-wall injury can lead to in situ thrombosis (Fig. 5.2).
 Pulmonary Artery Stump Thrombosis
Pulmonary Artery Stump Thrombosis
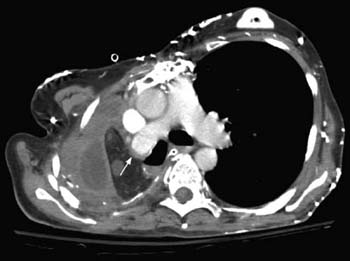
 In patients who have undergone resection for lung cancer, all three prothrombotic factors are present: vessel injury, disturbance of blood flow, and hypercoagulability.
In patients who have undergone resection for lung cancer, all three prothrombotic factors are present: vessel injury, disturbance of blood flow, and hypercoagulability.
 The prevalence is 12%.
The prevalence is 12%.
 There is a relationship between stump length and the development of in situ thrombosis.
There is a relationship between stump length and the development of in situ thrombosis.
 The shape of the thrombus can be convex (Fig. 5.3) or concave (Fig. 5.4).
The shape of the thrombus can be convex (Fig. 5.3) or concave (Fig. 5.4).
 Stump thrombosis appears to have a benign natural history.
Stump thrombosis appears to have a benign natural history.
Fig. 5.2 (A,B) Primary squamous cell carcinoma of the lung in a 74-year-old man. (A) CT demonstrates the tumor immediately adjacent to the anterior segmental artery of the left upper lobe (arrow). (B) After radiotherapy, there is now a well-defined filling defect within the anterior segmental artery of the left upper lobe, consistent with in situ thrombosis (arrow).
Fig. 5.3 Pulmonary artery stump in situ thrombosis in a 69-year-old man who underwent right pneumonectomy for lung cancer. CT scan demonstrates a convex pulmonary artery stump in situ thrombosis affecting the right pulmonary artery (arrow).
Fig. 5.4 Pulmonary artery stump thrombosis in a 55-year-old woman who underwent right pneumonectomy for recurrent chest infection resulting from post-irradiation fibrosis. CT scan at the level of main pulmonary artery obtained 9 months after pneumonectomy shows intravascular soft tissue that has a concave margin with respect to the contrast material (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree