Computed tomography (CT) and magnetic resonance (MR) imaging may demonstrate a wide variety of incidental findings in the breast, including primary breast carcinoma, the second most common cancer in women. It important to recognize the spectrum of pathologic conditions in order to properly assess the need for further workup. Some findings may be diagnosed as benign on the basis of CT/ MR imaging and clinical history alone, whereas others will require evaluation with dedicated breast imaging and possibly biopsy. This article serves to guide radiologists’ management of the wide spectrum of incidental breast findings encountered on cross-sectional imaging.
Key points
- •
Examination of the breasts, if included entirely or partially on cross-sectional imaging performed for unrelated reasons, is essential and can result in a substantial number of incidentally detected breast cancers.
- •
When an incidental breast abnormality is identified, one should evaluate its characteristics, as well as the clinical history and prior imaging examinations, to determine the need for further workup.
- •
In the absence of long-term stability or previous characterization, most breast masses detected at computed tomography (CT) and magnetic resonance (MR) imaging will require further workup, generally with mammography and targeted ultrasound. Breast imaging evaluation of women younger than the age of 40 should include ultrasound, and mammography can be performed at the discretion of the radiologist/breast imager.
- •
“Routine” cross-sectional imaging is not sensitive for the detection of breast cancer, and large cancers may be present in the breast but not identified on CT or on non-breast-dedicated MR imaging.
- •
Evaluation of axillary lymphadenopathy should be based on clinical context and imaging appearance. Biopsy is appropriate for suspected breast cancer metastases and for lymphadenopathy of unknown cause.
Introduction
A wide range of incidental breast findings may be identified on computed tomography (CT) and magnetic resonance (MR) imaging of the chest/abdomen. It is important to be familiar with the CT and MR imaging appearance of the spectrum of breast abnormalities, which can then be correlated with mammography and ultrasound if necessary. Some findings may be attributable to benign causes on the basis of CT/MR imaging and clinical history alone, whereas others will require evaluation with dedicated breast imaging and possibly biopsy. This article serves to review the gamut of incidental breast findings to help guide management.
Normal anatomy and standard imaging technique
Normal breast tissue consists of fibroglandular elements and fat. Lactiferous ducts extend from the nipple and branch into excretory, interlobular, and terminal ducts that branch into multiple rounded acini forming the functional unit for milk production. Each lactiferous duct is drained by approximately 15 to 20 lobes in a fanlike distribution. The highest density of glandular tissue is typically present in the upper outer quadrant of the breast. Cooper ligaments are thin, fibrous structures that attach to the skin fascia and pectoralis muscle, surrounding the glandular elements and fat. Between the glandular elements and the pectoralis muscle is retroglandular fat.
Breast density, the density of glandular tissue compared with fat, varies between patients because of multiple factors and may decrease with age as glandular tissue undergoes fatty involution. The American College of Radiology (ACR) publishes a Breast Imaging Reporting and Data System (BI-RADS) lexicon, which classifies breast density into 4 categories: extremely dense, heterogeneously dense, scattered areas of fibroglandular density, and almost entirely fatty. ,
Lymph nodes are most commonly seen in the axilla and in the upper outer quadrant of the breast along blood vessels but can be found anywhere in the breast (intramammary nodes; Fig. 1 ). Normal lymph nodes classically demonstrate a well-circumscribed, reniform shape with fatty hilum and can vary in size.

Mammography is the foundation of breast imaging and is used for both screening and diagnostic purposes. Breast ultrasound is commonly used for further evaluation of findings on mammography, but also as a screening tool in patients with dense breasts. MR imaging is typically not used as first-line breast imaging, although women with dense breasts as well as high-risk patients may elect supplemental screening breast MR imaging. Other indications for breast MR imaging include breast cancer staging, response evaluation to chemotherapy, and implant evaluation. At a minimum, a standard breast MR imaging examination comprises a T2-weighted/bright fluid sequence, a T1-weighted fat-suppressed precontrast sequence, and T1-weighted fat-suppressed postcontrast sequences. The postcontrast subtraction sequences allow for analysis of dynamic kinetic curves.
Prevalence and clinical relevance
Epidemiology
Breast cancer is the second most common malignancy in women (after skin cancer), and approximately 1 in 8 women in the United States will develop breast cancer during her lifetime. The World Health Organization estimates 2,261,419 new cases of breast cancer worldwide in 2020, with 684,996 deaths.
Prevalence of Incidental Breast Findings and Frequency of Malignancy
Numerous studies have investigated incidental breast findings on cross-sectional imaging performed for unrelated reasons, most of which are retrospective. Overall, the prevalence of incidental breast findings on CT is reported to be approximately 0.10% to 7.63%, noting that these numbers reflect findings explicitly dictated in the radiology report and may underestimate the true prevalence.
The reported malignancy rates regarding incidental breast findings on CT vary widely, ranging from 9% to 70%. Overall, the incidental cancer detection rates in women are approximately 0.004% to 0.30%. , Because of the high frequency of malignancy, the workup of incidental breast findings identified on cross-sectional imaging reflects a very low economic burden compared with primary breast screening. Furthermore, an even higher rate of malignancy (∼50%) can be seen when examining only those breast findings for which further workup is explicitly recommended by the interpreting radiologist. Unsurprisingly, a significantly increased rate of malignancy has been shown in older patients.
Data on incidental breast findings on MR imaging are even more limited compared with data on CT. The reported rate of abnormality detection on MR imaging is less than on CT, at 0.1% to 3%. , In a study of incidental breast findings on abdominal MR imaging, 3% (292/11,462) of examinations reported a breast abnormality, and dedicated breast imaging was recommended in 66%. The frequency of incidental breast cancer was 11% of patients who underwent follow-up imaging at their institution, 3% of all patients with reported abnormalities, and 0.99% of patients who underwent abdominal MR imaging. Other studies have reported cancer rates of 8% to 14%. ,
Approach
Diagnostic Criteria (Imaging Findings Predictive of Malignancy)
When an incidental breast mass is identified, the initial question is raised: is it malignant? The assessment begins by characterization of features, such as shape, margins, density, pattern of enhancement, and associated findings. Ideally, differentiation of benign and malignant breast findings on CT and MR imaging would be straightforward. However, imaging features of benign and malignant disorders are variable and not specific, with most studies evaluating breast findings on CT showing conflicting results. Some investigators report that ill-defined, spiculated, irregular, or lobular shapes/margins are predictive of malignancy when identified on CT. , , , However, others have found no significant difference in shape and margin characteristics between benign and malignant processes, and 1 study even found that what proved to ultimately be benign findings were more often lobular with spiculated margins. ,
A significant difference in enhancement between benign and malignant breast abnormalities has been shown. , However, most CT scans are performed as single-phase examinations, and, even in multiphasic examinations, quantitative enhancement analysis is not routinely performed. Nonetheless, contrast-enhanced examinations can reveal nonmass enhancement, and breast findings with fibroglandular background may be obscured on nonenhanced CT. It has even been shown that some abnormalities that could not be detected on mammography or sonography were identified on CT. Abnormalities can be better seen on CT than mammography particularly in the setting of dense breasts or location adjacent to the chest wall. However, it is important to note that CT is not sensitive and can lead to missing large, biopsy-proven breast cancers ( Fig. 2 ).

CT and MR imaging can also show local invasion of a malignant breast tumor into the pectoralis muscle or other structures. Although prior work has shown potential utility of CT for assessing the local spread of breast cancer, dedicated breast MR imaging is now used for this purpose.
Finally, axillary lymphadenopathy may be associated with malignant breast tumors. However, this is infrequently seen , and may be due to non–breast conditions, including lymphoma, arthritis/connective tissue disorders, sarcoid, and infectious disease.
Prior Studies
Although many incidentally discovered breast findings on cross-sectional imaging will require dedicated breast imaging, it is important to review the patient’s chart for any prior examinations that may be useful in the diagnosis or prevent the need for further imaging. It may also be prudent to review prior relevant examinations with a breast imaging colleague to correlate with findings seen on CT or MR imaging with the patient’s prior mammogram. Review may potentially obviate further workup, as demonstrated in a study on breast incidental findings on abdominal and chest MR imaging, where 92% (240/261) of documented abnormalities corresponded to known benign breast findings.
Guidelines/Imaging Workup
No published guidelines exist for the evaluation of incidentally detected breast findings, to the authors’ knowledge. The ACR does address workup of palpable breast abnormalities in the ACR Appropriateness Criteria, which could potentially be used as a framework. The criteria recommend initial evaluation with mammography for patients older than age 40 and initial evaluation with ultrasound for patients younger than age 30. Equal rating is given to mammography and ultrasound for patients between 30 and 39 years of age. It should also be noted that ultrasound is often performed after mammography to work up an indeterminate finding, unless the mammogram is clearly benign (BI-RADS 2).
Although there are no established guidelines, it is generally suggested that radiologists recommend diagnostic mammogram and targeted ultrasound for evaluation of incidental breast abnormalities , for women older than the age of 40. Ultrasound should be recommended for women younger than age 40, and mammography can be performed at the discretion of the breast imager. In addition, a study found that radiologist recommendation for a specific imaging examination (rather than “per clinician”) was associated with a 40% increase in compliance for subsequent diagnostic imaging.
Imaging findings of breast abnormalities
Malignant Breast Tumors
Primary breast cancer
Invasive ductal carcinoma
Invasive ductal carcinoma (IDC) is the most common subtype, accounting for up to 90% of all invasive breast cancers. If visible on CT/MR imaging, typical findings include a spiculated mass with early and/or peripheral enhancement, although imaging appearance can vary, and a circumscribed process does not exclude malignancy ( Fig. 3 ). The microcalcifications and architectural distortion of associated breast cancer detected on mammography are generally not appreciated on CT. ,

Invasive lobular carcinoma
Approximately 10% to 15% of invasive breast cancers are invasive lobular carcinomas. This malignancy is more likely to be bilateral and multifocal compared with IDC. As the tumor diffusely infiltrates the breast parenchyma, a discrete mass is often absent. Subtle architectural distortion on mammography is unlikely to be appreciated on CT. CT and MR imaging may show asymmetric soft tissue and nonmass enhancement ( Fig. 4 ). ,

Inflammatory breast carcinoma
Inflammatory breast carcinoma is an aggressive malignancy with poor prognosis. It produces the classic “peau d’orange” appearance of the breast on physical examination owing to dermal lymphatic invasion. The breast demonstrates erythema, warmth, induration, and possibly nipple retraction. Clinically, inflammatory carcinoma may resemble mastitis/abscess, but unlike infection, will not completely respond to antibiotic therapy. On imaging, findings of breast edema may be seen, including skin and trabecular thickening, as well as diffusely increased density. Skin thickening is often the most obvious CT finding ( Fig. 5 ), and a discrete mass may or may not be visualized. Axillary lymphadenopathy is common , , and may be identified on CT.

Mucinous carcinoma
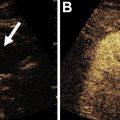
Mucinous (colloid) carcinoma is a rare type of well-differentiated adenocarcinoma, representing less than 2% of all invasive breast carcinomas, and usually has a good prognosis. Because of the large extracellular mucin composition, these tumors demonstrate hyperintensity on T2-weighted MR images ( Fig. 6 ) and may mimic a simple cyst or benign fibroadenoma because classic features of mucinous carcinoma also include a well-circumscribed margin and oval shape. Most mucinous tumors show gradual and progressive enhancement. The imaging features of mucinous carcinoma make it difficult to distinguish from benign processes, particularly on a noncontrast CT or MR image. When seen incidentally, caution must be taken not to dismiss these as inconsequential.

Papillary carcinoma
Papillary carcinoma is a rare cause of primary breast cancer, accounting for 1% to 2% of breast carcinomas. They are typically circumscribed masses with round, oval, or lobulated shape ( Fig. 7 ). Spiculation is rare. These tumors can be entirely solid or have cystic components. Almost half of papillary carcinomas arise in the retroareolar region and are usually found in postmenopausal women.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree