Hepatic incidental findings often are seen on cross-sectional imaging examinations of the chest, spine, pelvis, or other nondedicated hepatic imaging. Radiologists are tasked with appropriately triaging, which requires further evaluation, even in the setting of an otherwise limited evaluation. This article reviews common benign entities encountered on ultrasound, computed tomography, or magnetic resonance imaging, along with their characteristic imaging features. Imaging features that are suspicious for malignancy or suggest the need for further evaluation also are discussed. Two algorithms are proposed to guide radiologists in their recommendations based on patient risk factors, focal hepatic abnormality size, and available imaging features.
Key points
- •
Hepatic incidental findings often are seen on ultrasound, computed tomography, and MR imaging examinations; however, not all such findings require additional evaluation, which otherwise can be relatively costly and result in patient anxiety.
- •
A focal hepatic finding is more likely to require further evaluation in high-risk patients, including those patients with underlying liver disease or known malignancy.
- •
Simple cysts identified on ultrasound are unlikely to require further evaluation due to a high likelihood of benignity.
- •
Focal hepatic findings less than 1 cm in low-risk patients are unlikely to require further evaluation.
Introduction
Focal hepatic findings frequently are discovered incidentally on cross-sectional imaging performed for reasons other than for evaluation of the liver. Because these examinations often are not optimized for characterization of such hepatic findings, careful consideration should be given to whether these incidental liver findings (ie, incidentalomas) require further characterization. The role of the radiologist is to recognize and attempt to characterize these findings and, if required, to suggest appropriate follow-up. It is important to identify clinically actionable findings correctly, while making appropriate use of health care resources. The Incidental Findings Committee of the American College of Radiology (ACR) published their recommendations in 2010, with updates in 2017, that provide guidance on the management of liver incidentalomas detected by computed tomography (CT).
In the general population, a vast majority of incidental liver findings are benign entities: most commonly cysts, hemangiomas, and perfusion alterations. More than 5% of patients have liver metastases at the time of diagnosis of an extrahepatic malignancy, most commonly breast and colorectal cancer; therefore, a radiologist’s recognition of an incidental possible malignant hepatic nodule or mass may be the first step toward the diagnosis of an extrahepatic malignancy. Primary hepatic malignancies also may be detected incidentally but occur much less commonly than metastases.
The general approach for evaluating an incidental focal hepatic finding is to (1) consider whether technical factors allow for adequate interpretation; (2) determine the presence of features supporting benignity and/or malignancy; (3) compare to any prior imaging, including across modalities; and (4) interpret the risk of malignancy in the context of patient-specific factors, including age, gender, any history of malignancy or concurrent imaging/clinical findings suggesting malignancy, and the presence or absence of chronic liver disease.
The liver often is included, at least partially, on CT and MR imaging examinations of the abdomen, thorax, thoracolumbar spine, pelvis, and breast as well as on ultrasound examinations, including renal ultrasound. As such, incidental focal liver findings may be detected under circumstances that do not provide sufficient information to make a confident specific diagnosis. For ultrasound examinations, factors that influence the adequacy of the examination for characterization of focal liver findings include the transducer, frequency, focal zone, depth, and gain; in some cases, the finding may be more fully interrogated by the sonographer and in other cases recognized only retrospectively. For CT examinations, the resolution, reconstruction method, and phase of contrast (if any) are important considerations. Slice thickness may limit evaluation of small focal findings. MR examinations have similar considerations as CT examinations; however, the liver may be included only in a few sequences or only localizer sequences, and, for spine MR imaging, the liver may be obscured by the suppression band. Additionally, all imaging modalities have potential artifacts that may obscure all or part of the suspected liver finding, particularly when the focus of the examination was not the liver.
This article describes the multimodality imaging features of various focal liver findings and proposes an algorithmic approach for management of such incidental liver findings on ultrasound, CT, and MR examinations, which are inadequate for complete characterization of the liver. The authors’ recommended approach is to evaluate first whether there are any imaging features that are suspicious for malignancy and then to assess for the presence of features that suggest benignity. These imaging features include morphology, location, multiplicity, echogenicity/attenuation/signal, and growth ( Table 1 ). Additionally, the liver should be evaluated for secondary findings, including the presence of mass effect, perfusion alterations, biliary obstruction, capsular retraction, or underlying chronic liver disease, in particular, cirrhosis or steatosis.
| Morphology | Size Shape Margin Internal architecture |
| Location | Central vs peripheral Segment vs lobe vs diffuse Peribiliary vs periportal |
| Multiplicity | Single Multiple |
| Growth | Stable vs enlarging vs shrinking |
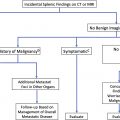
The imaging features of focal hepatic findings can overlap: atypical manifestations of benign processes can simulate malignancy, and some malignant tumors can resemble benign processes. This is true for dedicated liver imaging, and thus is particularly salient for imaging examinations that were not optimized for liver evaluation. It is crucial to understand patient-specific risk factors when evaluating a focal liver abnormality, because an atypical appearance of a benign process is far more common in patients who are at low risk of malignancy. For instance, focal liver findings less than 1 cm in size almost always are benign in low-risk patients, whereas in patients with known malignancy, approximately 10% demonstrate progressive growth and are presumed to represent metastases. Additionally, patients with most forms of cirrhosis or chronic hepatitis B infections should be evaluated based on the Liver Imaging Reporting and Data System (LI-RADS) criteria due to the markedly increased risk of primary liver malignancy. For simplicity, patients can be stratified into low-risk and high-risk categories, as proposed by the ACR in 2017, and as shown in Box 1 . In practice, the ordering provider also should consider a patient’s wider clinical context when considering the recommendations of the interpreting radiologist.
Low-risk patients a
No known malignancy
No hepatic dysfunction
No hepatic risk factors b
High-risk patients
Known malignancy with a propensity to metastasize to the liver
Cirrhosis
Presence of hepatic risk factors b
Cystic incidental findings
When an incidental finding is primarily cystic, attention should be given to the size, distribution, complexity, margins, relationship to the biliary tract, and enhancement patterns, to assess the risk of malignancy. Additional imaging may be needed if these features are not well evaluated or appear atypical, especially in high-risk patients. Both benign and malignant cystic processes can have mass effect, which may manifest as biliary obstruction or perfusion alteration. The most common cystic liver processes are discussed later. Uncommon cystic findings not discussed further here include very unusual findings, such as hepatic lymphangioma and mesenchymal hamartoma; those secondary to trauma, such as seroma/liquefied hematoma; and biloma as well as infectious or inflammatory cysts.
Definitely Benign: Simple Hepatic Cyst
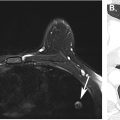
Hepatic cysts are extremely common and can be found in 2% to 18% of the general adult population, with a slight female predilection. True simple cysts are developmental and are composed of a thin wall lined with cuboidal epithelium, which do not communicate with the biliary tract. A vast majority of hepatic cysts are asymptomatic. Hepatic cysts are round or ovoid foci, ranging from several millimeters to multiple centimeters in size, but most are less than 3 cm. All have well-defined margins. Most cysts are unilocular and can have up to 2 thin and nonenhancing septations. Hepatic cysts may be solitary or multiple. On ultrasound, cysts appear as anechoic structures with thin or imperceptible walls and a clearly defined posterior wall. Increased through-transmission should be seen except with small cysts. On CT, cysts are homogeneous, fluid attenuation structures (<20 Hounsfield units [HU] when large enough to measure accurately) with sharp margins and no internal or mural enhancement. On MR imaging, they are homogeneous with sharp margins, very high signal on T2-weighted imaging (T2WI), similar to urine, bile, and cerebrospinal fluid, and low signal on T1-weighted imaging (T1WI) ( Fig. 1 ). They exhibit no enhancement and have no restricted diffusion.

Atypical manifestations
True hepatic cysts sometimes can contain hemorrhage or other debris, resulting in mild complexity or layering components, in which cases the cyst no longer is considered simple. Wall calcifications can develop as sequelae of hemorrhage or infection. Hemorrhagic or highly proteinaceous cysts can have increased signal on T1WI and decreased signal on T2WI but should demonstrate no enhancement with CT or MR imaging (or ultrasound) contrast media.
Suspicious features
Wall or septal thickening, nodularity, and enhancement are suspicious features warranting further evaluation.
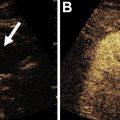
Definitely Benign: Biliary Hamartomas
Also known as von Meyenburg complexes, biliary hamartomas are benign ductal plate malformations composed of disorganized dilated bile ducts within a fibrous stroma that result from failure of embryonic bile ducts to involute. In most cases, there is no communication with the biliary tract. The prevalence is approximately 3% to 6% at autopsy and 1.5% by imaging. In rare cases, malignant degeneration to cholangiocarcinoma has been described. Biliary hamartomas typically present as numerous small rounded or irregular structures throughout the liver, with well-defined margins and a predilection for the subcapsular region. Biliary hamartomas typically are 0.5 cm to 1.5 cm and relatively uniform in size. Many hamartomas are less than 5 mm in size and, therefore, can be difficult to detect by ultrasound and CT but usually are well seen on MR with T2WI due to the high internal signal intensity ( Fig. 2 ). On ultrasound, visualized foci can appear hypoechoic, hyperechoic, or mixed, depending on the size and composition. Foci below ultrasound resolution may appear as a region of heterogeneous parenchymal echotexture. Comet-tail artifact can be seen with hyperechoic foci. On CT, hamartomas typically are seen as homogeneous fluid attenuation (<20 HU) structures with sharp and sometimes irregular margins. On MR imaging, they present as well-defined cysts with high signal on T2WI, low signal on T1WI, and no diffusion restriction. Predominantly solid foci, when present, are isointense to liver parenchyma on T1WI, and have intermediate signal on T2WI. On postcontrast images, larger foci may have a subtly enhancing rim from adjacent compressed hepatic parenchyma.

Atypical manifestations
Most biliary hamartomas are predominantly cystic, although sometimes a nodular area or rim of the solid fibrous component is visible and can show mild enhancement. The sonographic and CT appearance can resemble metastatic disease or hepatic abscesses in some cases. Alternative or concurrent diagnoses should be considered when there is marked variation in size or size greater than 3 cm.
Excluding or suspicious features
Prominent enhancement, interval growth, restricted diffusion, and calcifications warrant consideration of alternative, possibly malignant, diagnoses.
Definitely Benign: Peribiliary Cysts
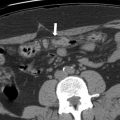
Peribiliary cysts develop from peribiliary glands, are lined by a single layer of epithelium, and do not communicate with the biliary tract. A recent classification framework has been proposed: type I hepatic peribiliary cysts are numerous and develop in the presence of chronic liver disease; type II extrahepatic cysts have a predilection for women without chronic liver disease or portal hypertension, often are solitary, and often present with biliary obstruction due to mass effect; and type III are mixed hepatic and extrahepatic. Peribiliary cysts typically present as multiple, less than 1 cm cystic structures seen on both sides of the portal vein, often most pronounced at the hepatic hilum and central portal triads, which has been described as a string-of-beads pattern ( Fig. 3 ). The typical distribution of noncommunicating cystic structures is key to diagnosis of hepatic peribiliary cysts in the appropriate clinical setting. Involvement may be segmental or diffuse. Increased size or number of hepatic peribiliary cysts is correlated with worsening chronic liver disease. On ultrasound, they appear as small cysts, which are most pronounced along the central intrahepatic portal veins. On CT, peribiliary cysts present as multiple nonenhancing, well-defined, low-attenuation structures along the sides of portal veins. In cases of confluent cysts, where individual foci are not resolvable, involvement of both sides of the portal vein can help distinguish it from intrahepatic biliary dilation but can resemble periportal edema. On MR imaging, they appear as well-defined cysts with high signal on T2WI, low signal on T1WI, and no diffusion restriction, enhancement, or communication with the biliary system.

Atypical manifestations
Confident diagnosis can be challenging when the number of peribiliary cysts is small and their distribution is unclear or when the number is too high and the bile ducts are obscured.
Excluding or suspicious features
Thickened or nodular walls, septations, or atypical distribution suggest other diagnoses.
Definitely Benign: Polycystic Liver Disease
Polycystic liver disease (PCLD) is an autosomal dominant condition resulting in diffuse hepatic cystic disease. PCLD is present in 75% to 90% of patients with autosomal dominant polycystic kidney disease, and isolated PCLD has a prevalence of less than 0.01%. Two types of cysts can be seen: intrahepatic cysts that likely arise from biliary hamartomas and peribiliary cysts. Cyst formation continues over time, and cysts often start to become large enough to be symptomatic at approximately the fifth decade. Treatment options include cyst aspiration, sclerosis, fenestration, enucleation, and liver transplantation, depending on symptom burden, liver function, and other clinical factors. The sonographic, CT, and MR imaging appearance of individual cysts is similar to simple hepatic cysts and peribiliary cysts, except in the setting of complications, such as hemorrhage or infection. Numerous cysts of varying sizes usually are present, often but not always with diffuse hepatic involvement ( Fig. 4 ). The cysts slowly increase in size with age, and at least 10 enlarging cysts must be present for the diagnosis of PCLD. No enhancement of the cyst walls or contents should be present.

Definitely Benign: Choledochal Malformation (Caroli Disease)
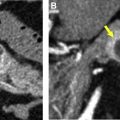
Choledochal malformations are a rare spectrum of developmental conditions affecting the biliary ductal plate with an autosomal recessive inheritance. Caroli disease results from abnormal cavernous ectasia of the large bile ducts, whereas Caroli syndrome affects all levels of the biliary tract, including the small ducts which can result in congenital hepatic fibrosis. Patients with this condition are at increased risk of cholangitis, strictures, choledocholithiasis, cirrhosis, and malignancies, including cholangiocarcinoma and papillary adenocarcinomas. There also is an association with multiple cystic conditions of the kidneys. Caroli disease manifests as saccular and fusiform biliary dilation from persistent ectatic embryonic bile ducts within the ductal plate, which communicate with the biliary tract. Segmental intrahepatic involvement is more common than diffuse disease with predilection for the left lobe. Extrahepatic involvement can be present. Periductal fibrosis of the portal triad can manifest as the central dot sign, although this fibrovascular bundle can be eccentrically located or not visualized. The size of the dilated ducts varies but typically is less than 3 cm in diameter. On ultrasound, Caroli disease presents as intrahepatic biliary dilation in a typical distribution. If a central dot sign is visualized, Doppler examination can demonstrate its fibrovascular nature. On CT and MR imaging, homogeneous fluid attenuation/signal saccular or fusiform biliary dilation with sharp margins is present. A central dot sign is characteristic ( Fig. 5 ). Communication with the biliary tract often is seen best with MR cholangiopancreatography. No restricted diffusion is present. On postcontrast images, the only enhancing component should be the fibrovascular bundle, which follows the enhancement pattern of the hepatic arteries and portal veins. Hepatobiliary phase contrast can demonstrate communication with the biliary tract, which can be helpful with the diagnosis in uncertain cases.

Atypical manifestations
The presence of saccular intrahepatic biliary dilation is a key distinguishing feature of Caroli disease from alternative diagnoses, such as primary sclerosing cholangitis and recurrent pyogenic cholangitis.
Excluding or suspicious features
Signs of malignancy include presence of solid masses or strictures with shoulders or irregular margins. Because patients with Caroli disease have an increased risk for malignancy, these patients need to have follow-up with liver specialists, even in the absence of imaging findings specific for malignancy.
Indeterminate: Ciliated Hepatic Foregut Duplication Cyst
Ciliated hepatic foregut duplication cyst is a rare congenital cyst composed of ciliated pseudostratified columnar epithelium. Most cases are asymptomatic; however, cases of malignant transformation to squamous cell carcinoma have very uncommonly been described. On imaging, a unilocular cyst typically is seen in an anterior subcapsular location in segment 4, or less commonly segments 5 or 8. There is a predilection for men. On ultrasound, the duplication cysts appear as an anechoic or hypoechoic cystic focus with sharp margins and no internal vascularity. On CT, a nonenhancing low to isoattenuation cyst is present in a typical location with sharp margins. Attenuation may be higher than simple fluid due to mucinous or proteinaceous contents ( Fig. 6 ). On MR imaging, this process presents with high signal on T2WI and variable signal on T1WI, depending on the cyst contents.