Infection
Within this chapter, the manifestations of how pulmonary vessels can be a vector in the spread of infection to the lungs or be secondarily affected by infection are explored. Pulmonary vessels can spread infection to the lungs via septic emboli; alternatively, pulmonary vessels can be affected by infection in adjacent lung parenchyma acquired from the airways. Classic examples of acute bacterial infection, recurrent bacterial infection, septic embolism, and of mycobacterial, fungal, viral, and parasitic infections are used to illustrate the range of interplay between infections and pulmonary vessels.
 Acute Bacterial Infection
Acute Bacterial Infection
 Lobar consolidation can occur in acute bacterial pneumonia. On contrast material–enhanced computed tomography (CT), the contour of the vessels within areas of uncomplicated consolidation usually appears normal (Fig. 8.1).
Lobar consolidation can occur in acute bacterial pneumonia. On contrast material–enhanced computed tomography (CT), the contour of the vessels within areas of uncomplicated consolidation usually appears normal (Fig. 8.1).
 Local inflammation from lung infection leads to an increase in the production of tissue factor and the inhibition of fibrinolysis. In this procoagulant environment, focal in situ thrombosis can occasionally occur (see Fig. 5.5 in Chapter 5).
Local inflammation from lung infection leads to an increase in the production of tissue factor and the inhibition of fibrinolysis. In this procoagulant environment, focal in situ thrombosis can occasionally occur (see Fig. 5.5 in Chapter 5).
 Consolidation causes a focal increase in pulmonary vascular resistance, which can slow the transit of blood and contrast material (see Fig. 4.30 in Chapter 4). Unopacified blood can mimic pulmonary embolism or in situ thrombosis.
Consolidation causes a focal increase in pulmonary vascular resistance, which can slow the transit of blood and contrast material (see Fig. 4.30 in Chapter 4). Unopacified blood can mimic pulmonary embolism or in situ thrombosis.
 Recurrent Bacterial Infection
Recurrent Bacterial Infection
 A pulmonary structural abnormality, such as the bronchiectasis seen in cystic fibrosis, can lead to recurrent bacterial infections.
A pulmonary structural abnormality, such as the bronchiectasis seen in cystic fibrosis, can lead to recurrent bacterial infections.
 Recurrent infections in patients with cystic fibrosis can cause lung and vessel wall necrosis, characterized by hemorrhagic pneumonia, as well as bronchial artery and pulmonary artery pseudoaneurysm (Fig. 8.2).
Recurrent infections in patients with cystic fibrosis can cause lung and vessel wall necrosis, characterized by hemorrhagic pneumonia, as well as bronchial artery and pulmonary artery pseudoaneurysm (Fig. 8.2).
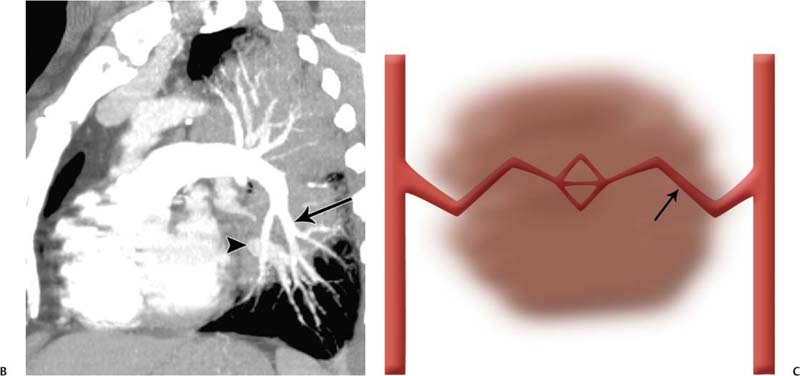
Fig. 8.1 (A–C) Acute streptococcal lobar pneumonia in a 54-year-old man. (A) Frontal chest radiograph demonstrates extensive consolidation with air bronchograms in the left lung. Acute streptococcal lobar pneumonia in a 54-year-old man. (B) Contrast material–enhanced CT maximum-intensity projection in a sagittal oblique plane demonstrates normal contours of the pulmonary arteries (arrow) and veins (arrowhead). (C) Illustration of pneumonia (represented by the brown circle). Coursing through the consolidated lung are vessels with normal contours and diameters (arrow).
 Massive hemoptysis in patients with cystic fibrosis is associated with Staphylococcus aureus infection and diabetes mellitus.
Massive hemoptysis in patients with cystic fibrosis is associated with Staphylococcus aureus infection and diabetes mellitus.
 Septic Emboli
Septic Emboli
 Septic emboli are seen in patients with infective endocarditis or periodontal disease. They are also associated with infected venous catheters or pacemaker leads.
Septic emboli are seen in patients with infective endocarditis or periodontal disease. They are also associated with infected venous catheters or pacemaker leads.

Fig. 8.2 (A,B) Pseudoaneurysm in a 25-year-old man with cystic fibrosis. (A) Spot film of a pulmonary angiogram demonstrates a pseudoaneurysm in the left upper lobe. Pseudoaneurysm in a 25-year-old man with cystic fibrosis. (B) Spot film demonstrates successful coiling of the pseudoaneurysm.
 The infecting organism varies with the cause. In intravenous (I.V.) drug abusers, S. aureus is the most common infective agent.
The infecting organism varies with the cause. In intravenous (I.V.) drug abusers, S. aureus is the most common infective agent.
 The radiologic appearances of septic emboli include nodules and wedge-shaped subpleural opacities with or without cavitation (Fig. 8.3).
The radiologic appearances of septic emboli include nodules and wedge-shaped subpleural opacities with or without cavitation (Fig. 8.3).
 Mycobacterial Infection
Mycobacterial Infection
 Tuberculous and nontuberculous mycobacteria often enter the lungs via the airways.
Tuberculous and nontuberculous mycobacteria often enter the lungs via the airways.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree