Infection and Inflammation
Disk Space Infection
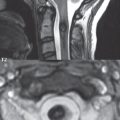
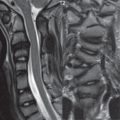
Disk space infection can be hematogenous in origin, or a complication of spine surgery. In the latter, the clinical presentation is usually several weeks following surgery, with delays in diagnosis common. Focal pain is a prominent clinical feature, but may be absent. In hematogenous seeding, it is stated that the disk serves as the initial site of infection in children, as it is richly vascularized, whereas in adults the initial site of infection is the subchondral bone or adjacent soft tissue. On CT, only late changes are noted, including disk space narrowing, cortical endplate destruction and irregularity, and an accompanying paraspinal soft tissue mass. On MR, the most common presentation of a disk space infection is that of a narrowed irregular disk ( Fig. 3.116 ), with focal high signal intensity on the T2-weighted scan (infected fluid pockets), enhancement of the disk space (other than the fluid), and a horizontal band of edema within the vertebral body both above and below (osteomyelitis), paralleling the infected disk space. The edema within the adjacent vertebral bodies will display enhancement on post-contrast scans obtained with fat saturation ( Fig. 3.117 ).


In early disease, the extent of edema within the adjacent vertebral bodies may be mild (or absent with discitis only), and in severe disease both the vertebral body above and below can be involved in their entirety. Although often less evident than on CT, the vertebral endplates will appear indistinct on MR in a disk space infection with accompanying osteomyelitis. A paraspinal soft tissue mass is also commonly present, of varying size, with enhancement post-contrast ( Fig. 3.118 ).

Often CT-guided biopsy is performed in order to have material for bacterial culture, prior to starting antibiotic treatment. Once treatment with intravenous antibiotics is initiated, the changes on MR (reflecting recovery) lag behind that of the clinical course. Other causes of paraspinal infection, without accompanying discitis and osteomyelitis, include hematogenous seeding (e.g., with a psoas abscess) and following surgery, with infection in the operative bed posteriorly.
Tuberculous Spondylitis
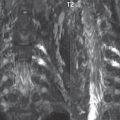
Tuberculous spondylitis follows a more indolent clinical course than pyogenic infection. In the United States this disease is seen primarily in immigrants (from Southeast Asia and South America) and in immunocompromised patients. The disease is primarily one of adults, and occurs due to hematogenous seeding. Differentiating features on imaging from pyogenic infection include inoculum in the anterior vertebral bodies, relative sparing of the disk space due to absence of proteolytic enzymes (early in the disease process) ( Fig. 3.119 ), involvement of multiple contiguous vertebral bodies (three or more levels in half of patients), and a large associated paraspinal mass. Although skip lesions are reported, these are uncommon (< 5%). Spread of disease occurs under the anterior longitudinal ligament. In long standing disease there will be extensive bone destruction.

Epidural Abscess
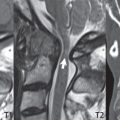
In recent years, epidural abscesses in the spine have become more frequent, with a subdural abscess, though, very uncommon. Infection can occur by hematogenous spread, direct extension (e.g., anteriorly from a disk space infection with osteomyelitis), or penetrating trauma. There may be associated meningitis and myelitis. MR is the modality of choice for detection and delineation, with CT of little value. Thickened inflamed (enhancing) soft tissue (phlegmon) is seen initially, progressing to a frank abscess (with fluid centrally). Contrast enhancement on MR can thus be homogeneous, or rimlike with central low signal intensity (pus). There can be canal compromise and cord compression, due to inflammation, granulation tissue, and any associated fluid collection ( Fig. 3.120 ). Lesions usually extend over several levels, and are often very extensive ( Fig. 3.121 ).


Both sagittal and axial imaging are important, the former for definition of extent of disease, and the latter for improved assessment of the thecal sac and cord compression. Diffusion weighted scans (an abscess will demonstrate restricted diffusion), relatively recently available with reasonable image quality for spine MR imaging, are an important complementary imaging sequence ( Fig. 3.122 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree