ANKYLOSING SPONDYLITIS (SERONEGATIVE SPONDYLOARTHROPATHY)
KEYFACTS
 This disease occurs predominantly in young men and is associated with histocompatibility antigen B27.
This disease occurs predominantly in young men and is associated with histocompatibility antigen B27.
 Ankylosing spondylitis is found in 1.4% of the population (particularly white Europeans or individuals of European descent).
Ankylosing spondylitis is found in 1.4% of the population (particularly white Europeans or individuals of European descent).
 Sacroiliitis is often the first manifestation followed by ankylosis of the lumbar and thoracic spine and ligamentous laxity (atlantoaxial subluxation), fractures, and epidural hematoma.
Sacroiliitis is often the first manifestation followed by ankylosis of the lumbar and thoracic spine and ligamentous laxity (atlantoaxial subluxation), fractures, and epidural hematoma.
 Complications: fractures (“banana” type), spontaneous epidural hematoma, erosive arachnoiditis with cauda equine syndrome, spinal cord infarctions, destructive noninfectious process (amyloidosis).
Complications: fractures (“banana” type), spontaneous epidural hematoma, erosive arachnoiditis with cauda equine syndrome, spinal cord infarctions, destructive noninfectious process (amyloidosis).
 Main differential diagnosis: DISH, juvenile rheumatoid arthritis, infectious sacroiliitis, retinoid-induced changes.
Main differential diagnosis: DISH, juvenile rheumatoid arthritis, infectious sacroiliitis, retinoid-induced changes.

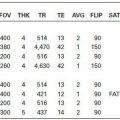
FIGURE 24-1. Lateral cervical spine radiograph shows fusion of vertebral bodies by anterior syn-desmophytes. The facet joints are also diffusely fused.

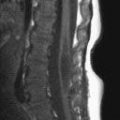
FIGURE 24-2. Mldsaglttal T2, In the same patient, shows vertebral body fusion and partia disc reabsorption.

FIGURE 24-3. Midsagittal T1, in a different patient, shows fusion of lumbar vertebra, disc obliteration, and widening of the canal.

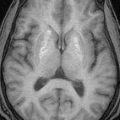
FIGURE 24-4. Axial T2, in the same patient, shows erosive changes in bone and nerve root clumping secondary to arachnoiditis.

FIGURE 24-5. Midsagittal CT reformation, in a different patient, shows fracture through the C6-7 disc.
FIGURE 24-6. Midsagittal CT reformation, in a different patient, shows severely displaced C5 involving both of its disc spaces.
SUGGESTED READING
Wang Y-F, Teng MM-H, Chang CY, Wu HT, Wang ST. Imaging manifestations of spinal fractures in ankylosing spondylitis. Am J Neuroradiol 2005;26:2067–2076.
 SPONDYUTIS AND DISCITIS, PYOGENIC
SPONDYUTIS AND DISCITIS, PYOGENIC
KEYFACTS
 Most adult spinal infections are caused by Staphylococcus aureus (60%, even in patients with AIDS), Enterobacter spp. (30%), Escherichia coli, Pseudomonas, and KLebsietta organisms.
Most adult spinal infections are caused by Staphylococcus aureus (60%, even in patients with AIDS), Enterobacter spp. (30%), Escherichia coli, Pseudomonas, and KLebsietta organisms.
 Most cases of discitis and osteomyelitis arise from hematogenous dissemination (e.g., drug users and immunodepressed patients), ascending route (genitourinary tract manipulations), and direct inoculation (traumatic injuries and postsurgical).
Most cases of discitis and osteomyelitis arise from hematogenous dissemination (e.g., drug users and immunodepressed patients), ascending route (genitourinary tract manipulations), and direct inoculation (traumatic injuries and postsurgical).
 In adults, the infection begins in the vertebral end-plates, while in children, the infection begins in the disc.
In adults, the infection begins in the vertebral end-plates, while in children, the infection begins in the disc.
 Discitis and osteomyelitis are usually seen in men between the sixth and seventh decades of life; the presenting symptoms are nonspecific (e.g., fever, pain, and elevated erythrocyte sedimentation rate).
Discitis and osteomyelitis are usually seen in men between the sixth and seventh decades of life; the presenting symptoms are nonspecific (e.g., fever, pain, and elevated erythrocyte sedimentation rate).
 Plain films are not sensitive and remain normal 7 to 10 days after onset of symptoms; magnetic resonance imaging (MBI) is the most reliable modality.
Plain films are not sensitive and remain normal 7 to 10 days after onset of symptoms; magnetic resonance imaging (MBI) is the most reliable modality.
 One-level involvement: 60% to 70%; involvement of multiple adjacent levels: 20%; multiple scattered level involvement: 10%.
One-level involvement: 60% to 70%; involvement of multiple adjacent levels: 20%; multiple scattered level involvement: 10%.
 Main differential diagnosis: degenerative changes, Schmorl node, trauma, hemodialysis (amyloid) arthropathy, tuberculosis, brucellosis, fungus.
Main differential diagnosis: degenerative changes, Schmorl node, trauma, hemodialysis (amyloid) arthropathy, tuberculosis, brucellosis, fungus.

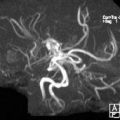
FIGURE 24-7. Sagittal T2 shows bright L1-L2 disc with erosion of end-plates and edema in bone marrow.

FIGURE 24-8. Corresponding postcontrast T1 shows disc enhancement and phlegmon in epidural space compressing the cauda equina.
FIGURE 24-9. Axial postcontrast T1, in the same patient, shows extensive patchy disc enhancement, thick and enhancing epidural space, and extension of inflammatory process to the perispinal region including the psoas muscles.

FIGURE 24-10. Corresponding axial CT shows to better advantage the bone destruction.

FIGURE 24-11. Midsagittal T2, in a different patient, shows two levels of discitis and osteomyelitis (arrows).

FIGURE 24-12. Corresponding fat-suppressed T2 shows to better advantage the extents of both infections.

FIGURE 24-13. Midsagittal CT reformation, in a different patient, shows discitis and adjacent bone involvement at the C5-C6 levels.

FIGURE 24-14. Midsagittal T2, in a different patient, shows edema of disc and adjacent vertebra.
SUGGESTED READING
Mahboubi S, Morris MC. Imaging of spinal infections in children. Radiol Clin North America 2001;39:215–222.
 EPIDURAL AND SUBDURAL ABSCESSES AND PHLEGMON
EPIDURAL AND SUBDURAL ABSCESSES AND PHLEGMON
KEYFACTS
 Infections in the epidural/subdural spaces occur secondary to extension of adjacent disci-tis or osteomyelitis (80%) or directly from hematogenous spread (common sources include the genitourinary tract, skin, and lungs).
Infections in the epidural/subdural spaces occur secondary to extension of adjacent disci-tis or osteomyelitis (80%) or directly from hematogenous spread (common sources include the genitourinary tract, skin, and lungs).
 Staphylococcus aureus is the most common responsible organism.
Staphylococcus aureus is the most common responsible organism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree