Fig. 8.1
Fungal sinusitis in leukemic patient. (a) Postcontrast CT shows sinusitis in both ethmoid and sphenoid sinuses extending to the right medial orbit with subperiosteal abscess formation. (b, c) Fat-suppressed T1-weighted axial (b) and coronal (c) images after gadolinium administration show severe inflammatory changes in the nasal cavity and sinuses with right orbital and intracranial (arrow) extension. This patient was diagnosed of having acute myelocytic leukemia and invasive aspergillosis
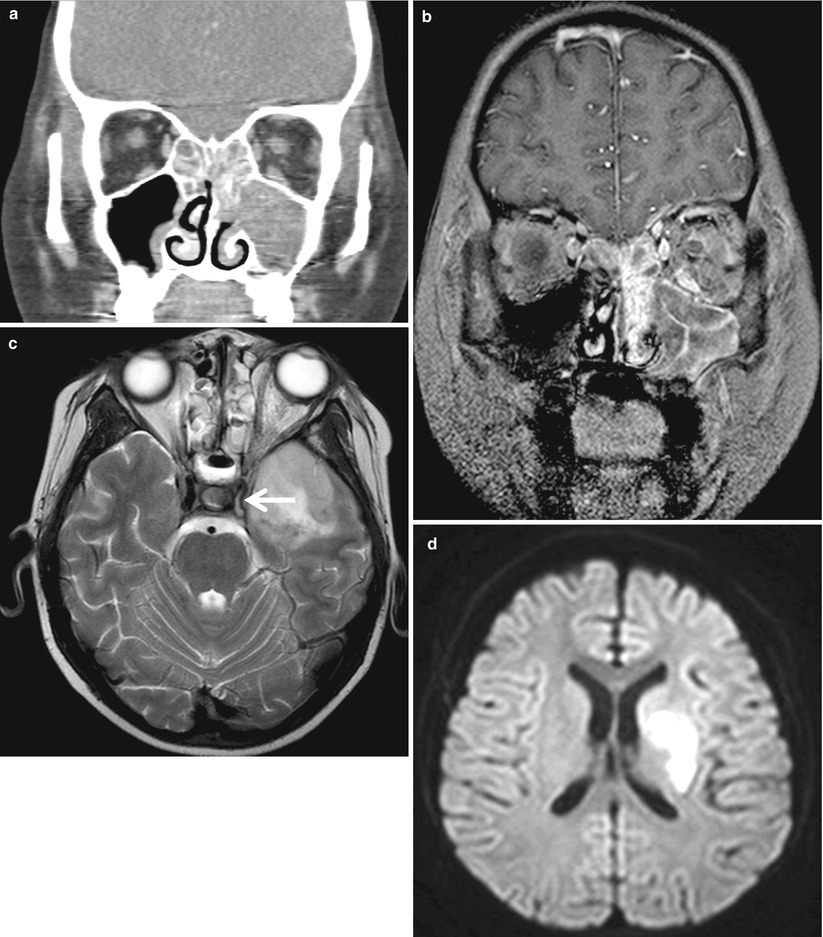
Fig. 8.2
Mucormycosis in leukemic patient. (a) Postcontrast coronal CT image shows total opacification in the left maxillary and both ethmoid sinuses. The medial wall of the left maxillary sinus is eroded, but no sinus expansion or calcification is noted. (b) Postcontrast fat-suppressed T1-weighted coronal image shows extensive sinus inflammation involving the bony structures. Meningeal enhancement is noted in the left inferior frontal region, and left inferior rectus muscle is enhanced representing intraorbital extension. (c, d) T2-weighted axial image (c) shows brain parenchymal involvement in the left temporal lobe. Note the lack of signal void in the left internal carotid artery (arrow in c) and resultant ischemic infarction in the left basal ganglia on diffusion-weighted image (d)
8.5.2 Frontal Sinusitis with Meningitis
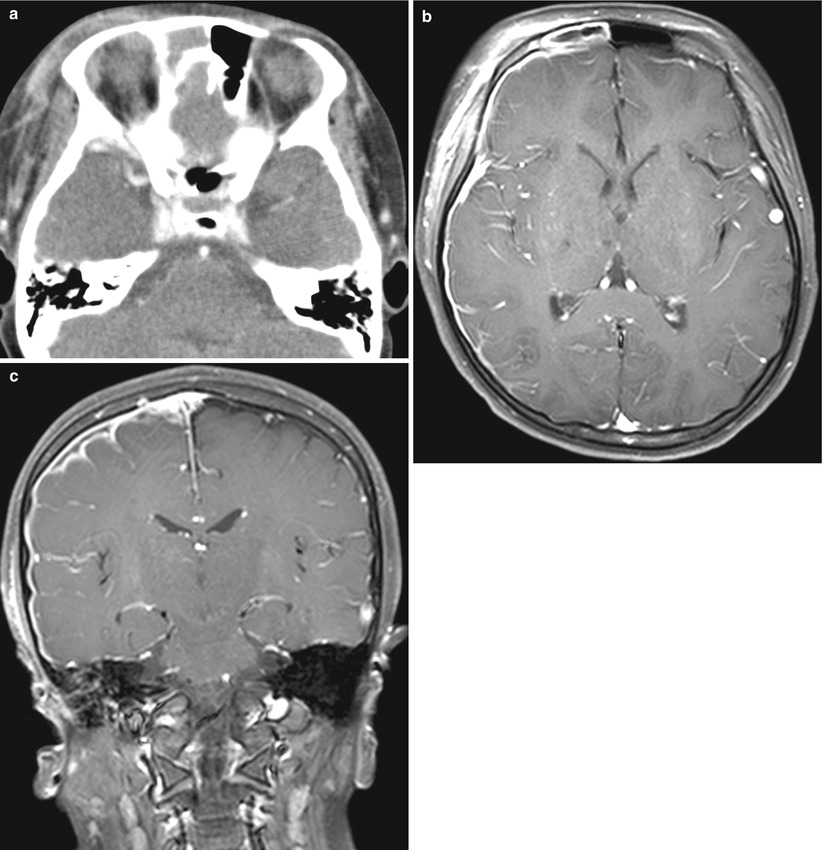
Fig. 8.3
Frontal sinusitis with meningitis in immunocompetent host. (a) Postcontrast axial scan shows right frontal sinus opacification and severe right periorbital soft tissue swelling. (b, c) Postcontrast fat-suppressed T1-weighted axial (b) and coronal (c) images show right frontal sinusitis with surrounding inflammatory changes and diffuse meningeal enhancement in keeping with meningitis
8.5.3 Otomastoiditis with Meningitis
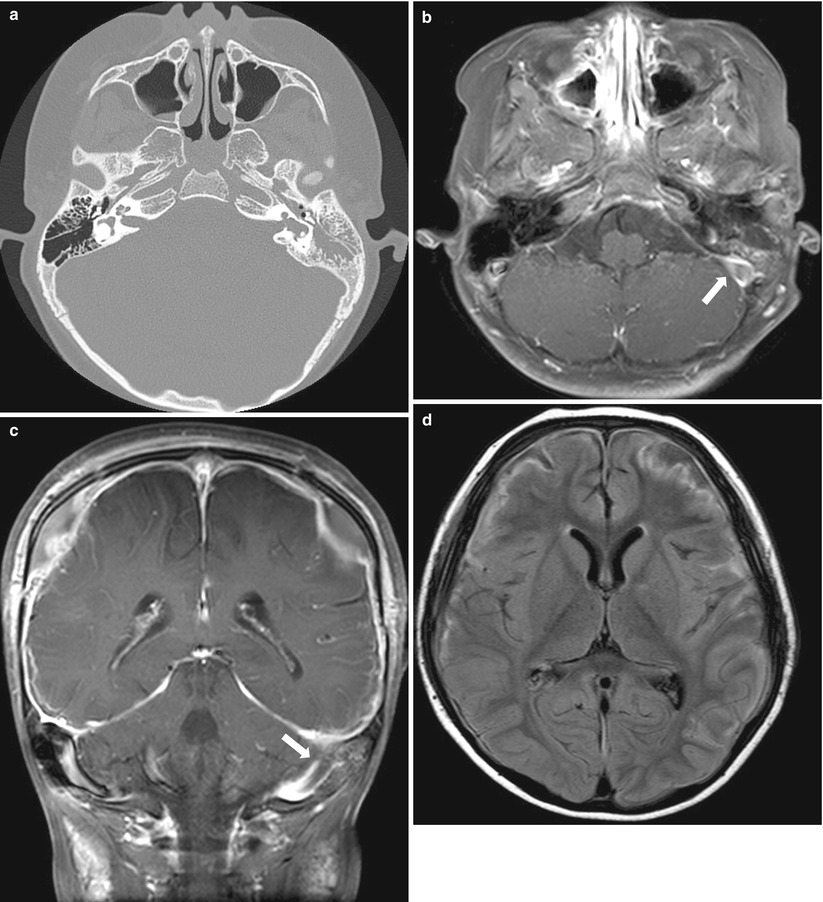
Fig. 8.4
Otomastoiditis with sinus thrombosis and recurrent pneumococcal meningitis. (a) Temporal bone CT shows abnormal soft tissue opacification in the left middle ear cavity and mastoid antrum/air cells. There is underlying congenital cochlear and vesicular dysplasia. Diffuse sclerosis is noted in the mastoid area. (b–d) MR postcontrast fat-suppressed T1-weighted axial (b) and coronal (c) images show abnormal enhancement in the mastoid region and nonenhancing thrombosis in the left sigmoid sinus (arrows in b and c). Axial FLAIR image (d) reveals abnormal high signal intensity along the cortical gyri, extraaxial fluid collections, and diffuse meningeal enhancement, representing meningoencephalitis
8.5.4 Retropharyngeal Abscess
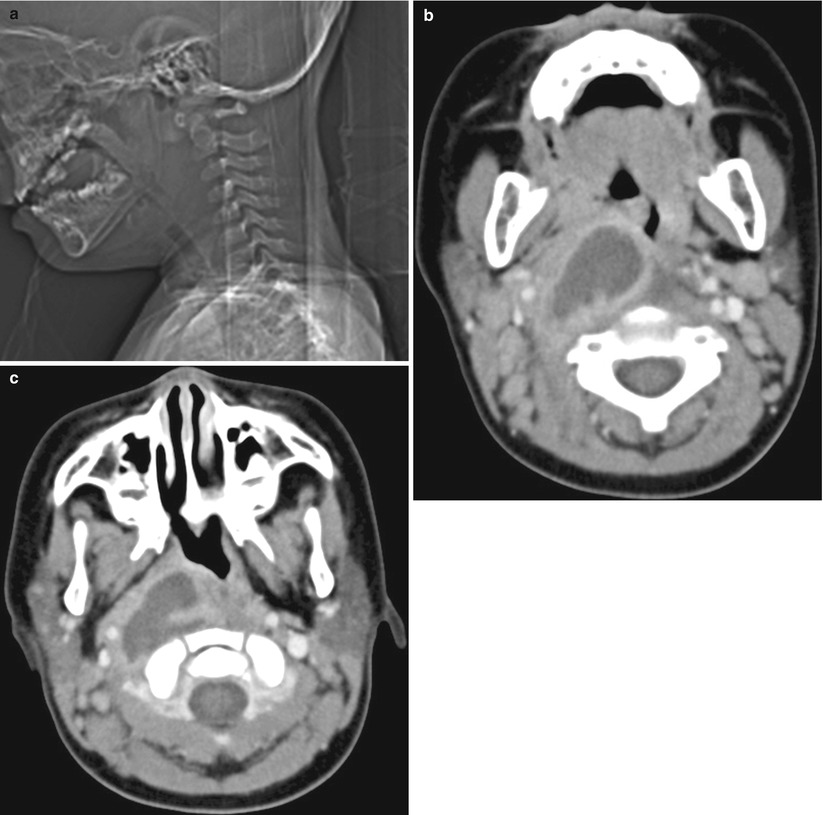
Fig. 8.5
Retropharyngeal abscess in a 3-year-old girl. (a) CT scout image shows widening of retropharyngeal prevertebral soft tissue space with oropharyngeal and hypopharyngeal airway obliteration. (b, c) Postcontrast CT scans at the mandible body level show a thick rim-enhancing cavitary lesion in the right retropharyngeal space, which compresses the oropharyngeal airway to the opposite side. Pus was aspirated
8.5.5 Cervical Reactive Lymph Node Hyperplasia
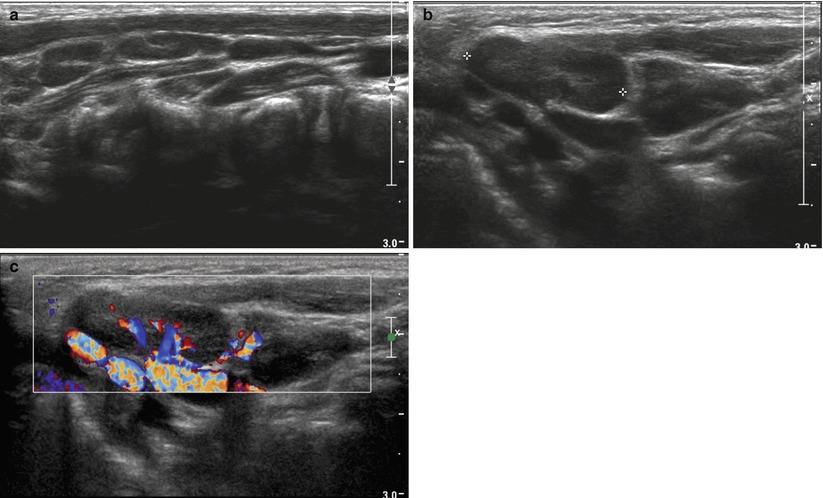
Fig. 8.6
Reactive lymph node hyperplasia in a 3-year-old boy who presented with mild fever and palpable nodules. (a, b) Ultrasound images through the right upper neck show multiple ovoid or elongated hypoechoic lesions with central linear echogenicity representing central hilar structures, which is a characteristic finding of benign lymphadenopathy. (c) Color Doppler study reveals prominent but preserved central vascularity, which is also one of the findings of benign inflammatory lymph nodes
8.5.6 Kikuchi Disease
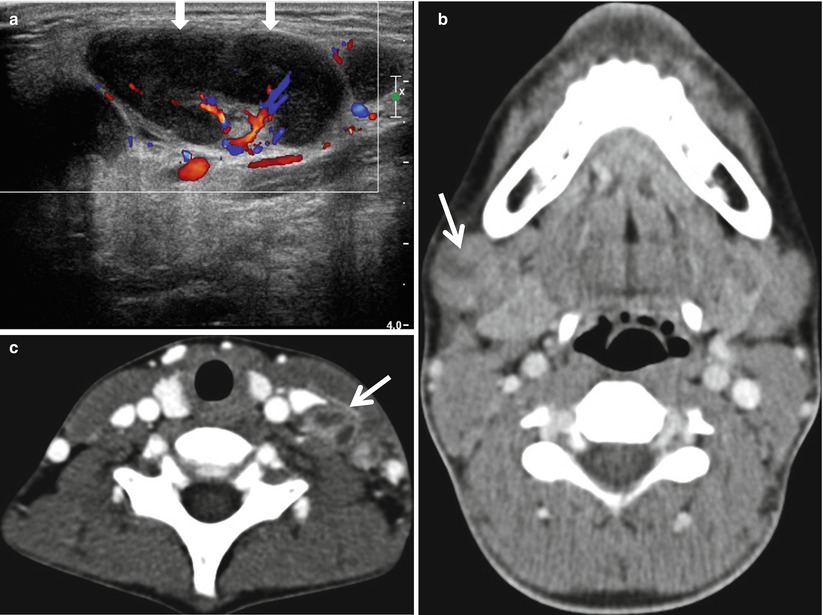
Fig. 8.7
Kikuchi disease in a 13-year-old boy. (a) Color Doppler ultrasound of the right submandibular region shows a large enlarged lymph node (arrows) with profound hypoechogenicity and increased central vascularity. (b, c) Postcontrast CT through submandibular gland (b) and thyroid gland (c) show enlarged lymph nodes with internal low density suggesting necrotic areas (arrows in b and c). Excisional biopsy of the cervical node revealed necrotizing lymphadenitis, consistent with Kikuchi lymphadenitis. No organism was identified on AFB and GMS staining
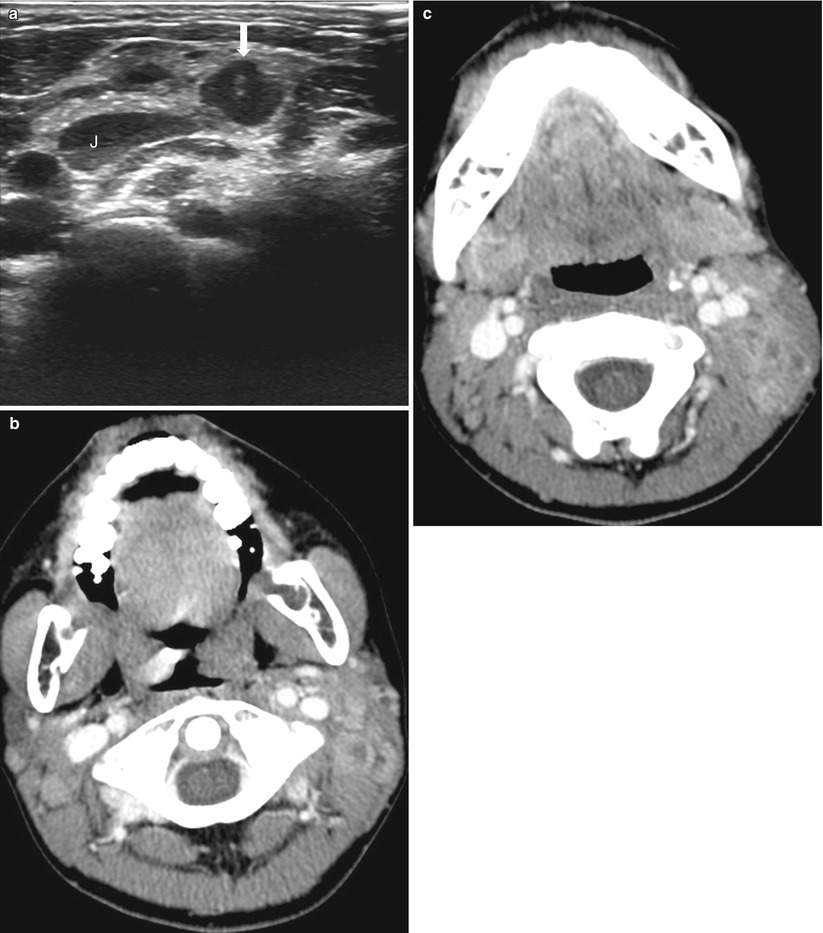
Fig. 8.8
Kikuchi disease in another 13-year-old boy. (a) Ultrasound of the left neck shows a lobulating contoured hypoechoic lesion (arrow) representing an enlarged lymph node just lateral to the internal jugular vein (J). (b, c) Postcontrast CT of the neck shows conglomerated lymph nodes in the left posterior cervical space with rim enhancement suggesting internal necrosis. Biopsy confirmed Kikuchi disease. There is reactive lymph node hyperplasia in the right posterior neck as well
8.5.7 Kawasaki Disease (Mucocutaneous Lymph Node Syndrome)
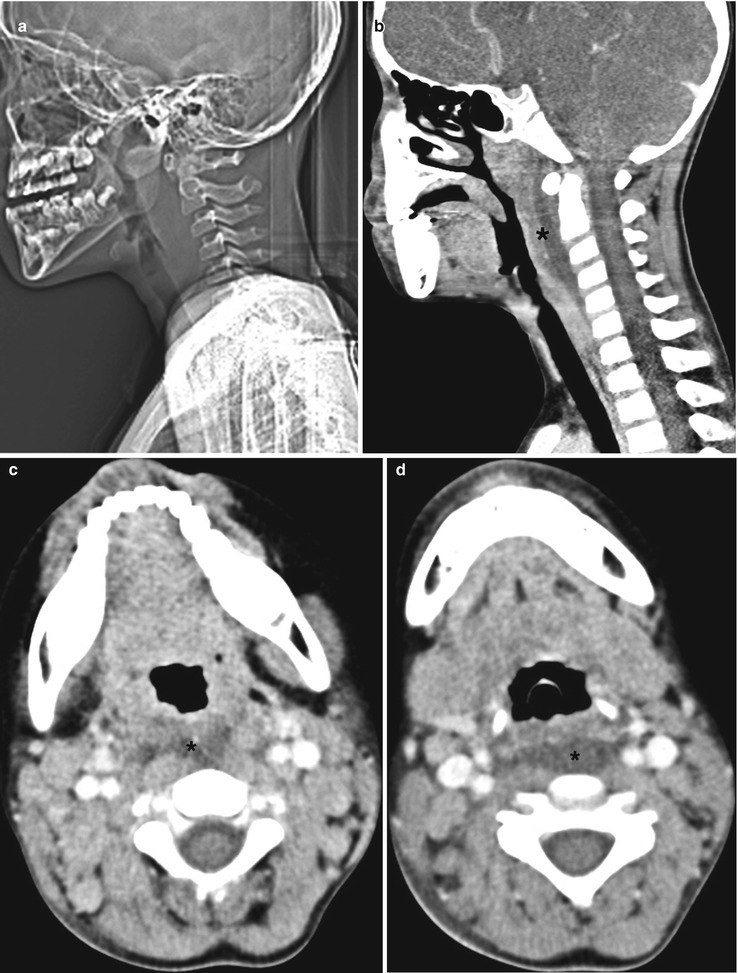
Fig. 8.9
Mucocutaneous lymph node syndrome in a 5-year-old boy. He had a history of prolonged fever, cervical adenopathy, skin rashes, strawberry tongue, and conjunctival injection, which fulfilled the diagnostic criteria for Kawasaki disease. (a, b) CT scout image (a) and sagittal reconstructed image (b) show retropharyngeal soft tissue space widening with low attenuating collection (* in b) in the prevertebral region. (c, d) Axial postcontrast CT images show multiple enlarged lymph nodes along the bilateral jugular and spinal accessory chains. There is low attenuating edematous fluid collection in the retropharyngeal space (* in c and d)
8.5.8 Infectious Mononucleosis
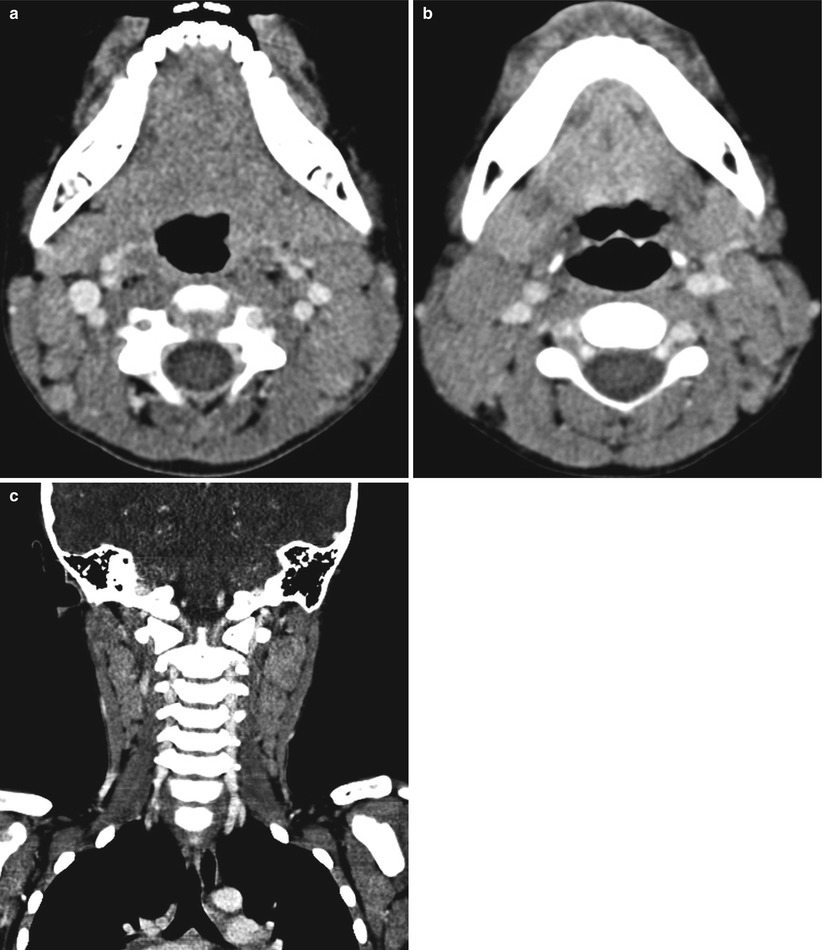
Fig. 8.10




Infectious mononucleosis in a 7-year-old boy with hepatosplenomegaly. His blood test showed atypical lymphocytosis and positive result for Epstein-Barr virus (EBV) viral capsid antigen (VCA) IgM. (a–c) Postcontrast axial (a and b) and coronal (c) images show bilateral cervical lymphadenopathy, which is homogeneously enhanced
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree