, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
14.1 Spondyloarthropathy
14.1.1 Ankylosing Spondylitis
14.1.2 Psoriatic Arthritis
14.2 SAPHO Syndrome
14.3 Rheumatoid Arthritis
14.4.1 Ankylosing Spondylitis
14.4.2 Psoriatic Arthritis
14.4.3 SAPHO Syndrome
14.4.4 Rheumatoid Arthritis
Abstract
Noninfectious inflammatory arthritis involving the spine includes spondyloarthropathies, SAPHO syndrome, and rheumatoid arthritis. In this chapter, the spinal manifestations of ankylosing spondylitis, psoriatic arthritis, SAPHO syndrome, and rheumatoid arthritis will be discussed.
Noninfectious inflammatory arthritis involving the spine includes spondyloarthropathies, SAPHO syndrome, and rheumatoid arthritis. In this chapter, the spinal manifestations of ankylosing spondylitis, psoriatic arthritis, SAPHO syndrome, and rheumatoid arthritis will be discussed.
14.1 Spondyloarthropathy
Spondyloarthropathy (previously known as seronegative spondyloarthropathy) is a spectrum of chronic inflammatory joint disorders which manifest as generalized enthesopathy. Ankylosing spondylitis (AS) and psoriatic arthritis (PA) are the most prevalent. Other less frequent spondyloarthropathies include Reiter’s syndrome, enteropathic arthropathies (Crohn’s disease or ulcerative colitis), and undifferentiated spondyloarthropathy. Generally, spondyloarthropathies have several common features. The spine and sacroiliac joint can be affected, which causes back pain and stiffness. The age of onset ranges from 20 to 40 years. There is a genetic predisposition and an association with the human leukocyte antigen (HLA) B27. Results of serological tests for rheumatoid factors are almost always negative. Spondyloarthropathy involves the cartilaginous joints, entheses, and synovial joints.
14.1.1 Ankylosing Spondylitis
Ankylosing spondylitis (AS) predominantly affects the spine and sacroiliac joints that can lead to severe, chronic pain and discomfort. In the advanced stage, the inflammation and bone formation of the spine results in painful stiffness of the entire spine, loss of the lumbar lordosis, and severe thoracic kyphosis (Levine et al. 2004). HLA-B27 is positively expressed in up to 95 % of patients with ankylosing spondylitis, although 5 % of patients are HLA-B27 negative. Ankylosing spondylitis tends to progress cephalad from the SI joints to the lumbar spine and eventually to the cervical spine. Characteristically, ankylosing spondylitis presents as an insidious onset of low back pain and morning stiffness persisting for more than 3 months. Pain on the sacroiliac regions can be prominent in the early phases of the disease and may disappear after ankylosis of the sacroiliac joints.
The radiographic findings reflect the underlying pathological processes, namely, inflammation, bony repair, and ossification of the spine. The inflammation reveals as subchondral bone erosions, while bony repair and ligamentous ossification presents as subchondral sclerosis and osseous ankylosis. According to the modified New York criteria, a definite diagnosis of ankylosing spondylitis requires the presence of obvious sacroiliitis by plain radiography as well as typical clinical findings (low back pain lasting for 3 months, decreased spinal mobility, and decreased chest expansion) (van der Linden et al. 1984). The criteria, however, can’t diagnose the early stages of ankylosing spondylitis due to the obligation of evident sacroiliitis by plain radiography.
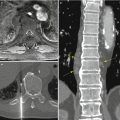
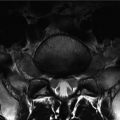
Sacroiliac Joint
Sacroiliitis is the earliest radiographic finding of ankylosing spondylitis. Initial change is blurring of the subchondral cortex on the iliac side of the sacroiliac joints. The erosions usually develop earlier on the iliac side due to thinner iliac cartilage. After then, both sides of the sacroiliac joints are involved generally bilaterally and symmetrically (Bennett et al. 2004). Haziness of the subchondral bone on the radiography is an important finding of sacroiliitis that is not observed in degenerative joint disease. This finding is followed by the erosive changes of the joint and mild subchondral sclerosis. The erosions become larger with widening of the joint space (pseudo-widening), and the subchondral sclerosis (reactive bone proliferation) becomes more prominent. The destruction of cartilage progresses with narrowing of the joint space. The SI joints come to be fused with ossification of the capsuloligamentous structures. In advanced stage, the joint shows complete ankylosis with decreased periarticular sclerosis. The modified New York criteria grades the sacroiliitis as follows: grade 0 indicates normal findings; grade 1, suspicious changes; grade 2, minimum abnormality, defined as small localized areas with erosion or sclerosis without change in the joint width; grade 3, obvious abnormality with widening of the joint space; and grade 4, total ankylosis. Based on the modified New York clinical criteria, grades 0 or 1 are not sufficient for the diagnosis of definite ankylosing spondylitis.
CT is more sensitive than plain radiography in detecting subtle cortical erosions of the sacroiliac joints. MR imaging can detect the sacroiliitis earliest and evaluate the disease activity. Postcontrast T1 fat-saturated images improve the delineation of activity signs.
Bilateral and symmetrical sacroiliac joint abnormalities in ankylosing spondylitis must be differentiated from hyperparathyroidism and osteitis condensans ilii. In hyperparathyroidism, subchondral bone resorption in the ilium and subsequent joint space widening can be seen. In osteitis condensans ilii, a triangular segment of bony sclerosis is noted in the inferior aspect of the ilium. The joint surface is not affected, and the joint space is maintained. Osteitis condensans ilii results from chronic stress on the sacroiliac joints and occurs almost exclusively in women.
Spine
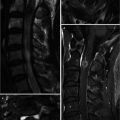
Spinal changes in ankylosing spondylitis can be seen in the diskovertebral junction, facet joints, costovertebral joints, posterior ligamentous attachments, and atlantoaxial joints. Ankylosing spondylitis predominantly involves the diskovertebral junction, including osteitis, erosions, syndesmophytes, and osteoporosis with diskal ballooning.
Osteitis causes cortical erosions along the anterior corners of the diskovertebral junction, typically seen at the thoracolumbar junction (Romanus lesions). These corner erosions and bony proliferation along the anterior aspect of the vertebral bodies result in loss of the normal concavity of the anterior vertebral surfaces and squaring of the vertebral bodies. Reactive subcortical scleroses frequently occur at the anterior corner of vertebral bodies (shiny corner sign). Romanus lesions show inflammatory and edematous changes at the anterior corners of the vertebral bodies on MRI (Jevtic et al. 2000). Fatty marrow change at vertebral corners on MR images is suggestive of chronic stage of the disease. Ossification of anterior and lateral paraspinal ligaments and the outer annulus of the disk results in thin vertical syndesmophytes. In later phase, ankylosis with diffuse syndesmophytes leads to the undulating vertebral contour (bamboo spine).
Ankylosing spondylitis may manifest as destructive diskovertebral lesions (Andersson lesions). Two types of Andersson lesions have been described. The type-A Andersson lesion is an inflammatory change in the central subchondral portions of the diskovertebral junction and reveals as Schmorl’s node, irregularity of vertebral endplate, and disk space narrowing. The type-B Andersson lesion is a pseudoarthrosis following a diskovertebral fracture in the frangible ankylosed spine. The type-B Andersson lesion is usually located at the thoracolumbar or cervicothoracic junction, around skip area of ankylosed segments.
The facet joints may exhibit cortical erosions, sclerosis, capsular calcifications, and fusion. The ankylosis of the facet joints is the main cause of the rigidity of the spine. Ossification of the facet joint capsules makes two vertical radiodense lines (the tram-track sign or trolley sign) on anteroposterior (AP) radiograph. Ossification of the posterior interspinous and supraspinous ligaments of the lumbar spine is seen as a single central radiodense line (the dagger sign) on AP radiographs.
Osteoporosis and spinal rigidity of advanced ankylosing spondylitis can cause spinal fractures (Wang et al. 2005). Fractures in ankylosing spondylitis are likely to be transverse and may spread through the vertebral body or intervertebral disk. The adjacent anterior and posterior paraspinal ligaments are frequently disrupted, and spinal cord compression or contusion may occur.
Severe osteoporosis may result in smooth biconcave endplate depressions of the vertebral body (fish vertebrae) and biconvex disk (diskal ballooning). Dural ectasia and associated widening of the spinal canal may develop particularly in the lumbar region.
14.1.2 Psoriatic Arthritis
Psoriatic arthritis may involve both the appendicular and the axial skeleton. Skin disease commonly develops before joint disease by months or years. HLA-B27 antigen is expressed in 25–60 % of patients with psoriatic arthritis. The hands and feet are the commonly affected sites in psoriatic arthritis. The findings in axial skeleton of psoriatic arthritis are similar to those of ankylosing spondylitis except for several differences. Unilateral sacroiliitis, asymmetry of syndesmophytes, and development of parasyndesmophytes may distinguish psoriatic arthritis from ankylosing spondylitis (Harvie et al. 1976).
Approximately 20 % in patients with psoriasis have sacroiliac joint changes. The radiographic findings resemble ankylosing spondylitis, but ankylosis of sacroiliac joints is infrequent in psoriatic arthritis.
In the spine, prominent paravertebral ossification and large asymmetric bony bridging can occur along the diskovertebral margins mainly on the thoracolumbar junction in psoriatic arthritis (Bennett et al. 2004). These are different features from the syndesmophytes of ankylosing spondylitis. Osteitis and squaring of the vertebral bodies are uncommon in psoriatic arthritis.
14.2 SAPHO Syndrome
The SAPHO (synovitis, acne, pustulosis, palmoplantaris, hyperostosis, and osteitis) syndrome is a variety of inflammatory bone disorders that may be associated with skin changes. The earliest and most common articular manifestations are swelling and hyperostosis at the sternomanubrial region. Bone scan can easily detect the increased uptake in both sternoclavicular joints and the sternomanubrial junction. Spinal involvement may manifest as painful stiffness and chronic low back pain. The features of the spine involvement in the SAPHO syndrome are mixed osteolytic and sclerotic changes, which are osteophytes, syndesmophytes, squaring of the vertebral bodies, and erosions of the anterior corners usually in two or more vertebral bodies including the intervertebral space. Spinal involvement can be misdiagnosed as chronic pyogenic spondylitis.
14.3 Rheumatoid Arthritis
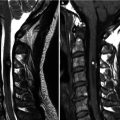
Rheumatoid arthritis (RA) is a common autoimmune disease that causes symmetric and erosive synovitis of peripheral joints. Rheumatoid arthritis has a predilection for cervical region at the spine involvement. The characteristic findings in rheumatoid arthritis are atlantoaxial subluxation, odontoid and apophyseal joint erosions, subaxial subluxation, intervertebral disk space narrowing, subchondral erosion and sclerosis, and spinous process destruction.
The most common finding in cervical spine is anterior atlantoaxial subluxation which is abnormal widening between the anterior arch of the atlas and the odontoid process (atlantodental interval, ADI > 2.5 mm in adults). Anterior atlantoaxial subluxation is produced by laxity of the transverse ligament. The distance between the posterior surface of the odontoid and the anterior margin of the posterior ring of the atlas (posterior atlantodental interval, PADI), however, directly measures the spinal canal and is more important for the evaluation of atlantoaxial subluxation. The PADI of less than 14 mm is thought to be an indication for surgical stabilization (Wasserman et al. 2011). The subluxation of the cervical spine and pannus formation in rheumatoid arthritis may compress the spinal cord or brainstem. MRI can demonstrate cord compression due to bone and periodontoid pannus.
With progression of instability, the odontoid process migrates superiorly within the ring of the atlas. With continued cranial settling, the anterior atlantodental interval may paradoxically decrease. The cervicomedullary angle assesses superior migration of the odontoid. The cervicomedullary angle is the angle between a line drawn along the anterior aspects of the cervical cord and another line along the medulla on midsagittal MRI. A normal angle is between 135° and 175°. Values less than 135° are significant for vertical settling and correlate with myelopathy (Bundschuh et al. 1988).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree