4 Inflammatory Diseases
Brain Abscess, Bacterial
Frequency: a common computed tomography (CT) diagnosis.
Suggestive morphologic findings: ring-enhancing lesion with smooth margins, often located near the frontal sinus or petrous temporal bone.
Procedure: antibiotic therapy, surgery if required.
Other studies: magnetic resonance imaging (MRI) can detect contrast enhancement with higher sensitivity. It is especially useful for detecting or excluding accompanying meningeal and ependymal reactions. Also better than CT for detection of complicating dural sinus thrombosis.
Checklist for scan interpretation:
 Number and location of enhancing lesions?
Number and location of enhancing lesions?
 Proximity to frontal sinus or petrous bone?
Proximity to frontal sinus or petrous bone?
 Inflammatory changes in frontal sinus or petrous bone (bone window)?
Inflammatory changes in frontal sinus or petrous bone (bone window)?
 Meningeal enhancement?
Meningeal enhancement?
 Mass effect (midline shift, ventricular compression, etc.)?
Mass effect (midline shift, ventricular compression, etc.)?
 Pathogenesis
Pathogenesis
Bacterial brain abscesses can develop in a variety of clinical settings. Many brain abscesses result from an infection of the frontal sinus or petrous bone that has extended intracranially (Fig. 4.1). In both cases, the normally air-filled portions of these bones become filled with fluid, providing a clue to the etiology of the intraparenchymal changes.
Multiple brain abscesses may develop as a complication of sepsis (Fig. 4.2) or endocarditis (Fig. 4.3). In the latter case, infected thrombi are shed from the diseased valves and disseminate to the brain by the hematogenous route. The blood currents tend to carry the septic emboli through the internal carotid artery and into the middle cerebral arteries. Once septic emboli have been seeded into the territory of the middle cerebral artery (MCA), a brain abscess begins to form. This occurs more or less independently of the specific etiology. The initial stage is a focal cerebritis, which soon develops central necrosis and is surrounded by perifocal edema. With time, the lesion forms a capsule and “ripens” into an established brain abscess.
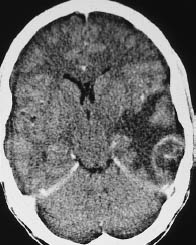
Fig.4.1 Otogenic brain abscess. Postcontrast CT shows a digitate pattern of hypodensity in the left temporal lobe, representing perifocal edema. The abscess itself appears as a ring-enhancing structure bordering the calvarium above the petrous bone.

Fig. 4.2 Septic brain embolism. Postcontrast CT shows conspicuous enhancing lesions in the right occipital and left frontoparietal areas, and a less prominent lesion in the left occipital area. The gyral changes show the ring-enhancing pattern typical of brain abscess.
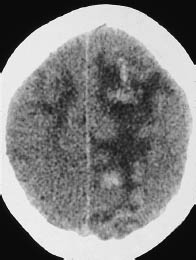
Fig. 4.3 Valvular endocarditis. Noncontrast CT in a patient with clinically confirmed valvular endocarditis shows bilateral string-of-beads hypodensities with central hemorrhages, mainly on the right side. The hyperdense areas on the plain scan did not enhance after contrast administration.
The bacterial inflammatory process can have various central nervous system (CNS) manifestations. The brain abscess may be accompanied by localized or more extensive meningeal inflammation (Fig. 4.4), subdural empyema formation, ventriculitis (Fig. 4.5), or dural sinus thrombosis. Bacterial contamination from a penetrating head injury can also result in a brain abscess (Fig. 4.6).
 Frequency
Frequency
The incidence of brain abscess is increased in patients with pulmonary disease (especially pulmonary arteriovenous fistulae or bronchiectasis), patients with endocarditis, and immunosuppressed patients. Males predominate by about a 2:1 ratio.
 Clinical Manifestations
Clinical Manifestations
While purulent forms of meningitis typically present with nuchal rigidity, headache, and hypersensitivity to light and sound, the clinical picture of brain abscess is dominated by focal neurologic symptoms. These may be accompanied by signs and symptoms of meningeal irritation.
 CT Morphology
CT Morphology
The typical CT appearance of brain abscess is that of a ring-enhancing lesion with central necrosis and perifocal edema (see Fig. 4.1). The ring is usually thin and uniform, without scalloping. As noted above, abscesses due to sinusitis are located either in the frontal lobe or in the middle or posterior cranial fossa in close proximity to the petrous bone. Brain abscesses secondary to endocarditis tend to be small, multiple, and located at the gray-white matter junction in the territory of the MCA.
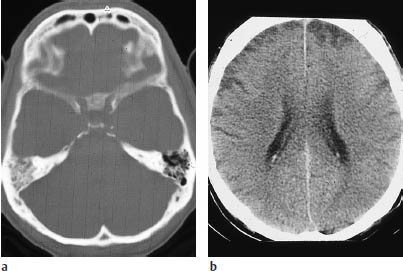
Fig. 4.4a, b Otogenic meningitis.
a The bone-window scan shows opacification of the right mastoid due to inflammatory disease.
b Plain CT in a patient with clinically confirmed meningitis shows bilateral cortical hypodensities that represent secondary infarcts due to vasculitis. The meningitis itself is not demonstrable on CT scans.
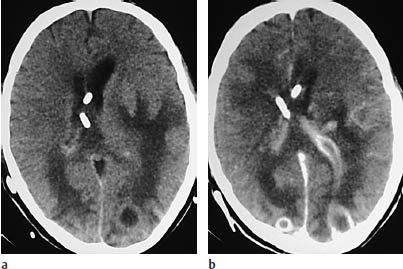
Fig. 4.5a, b Brain abscess with ependymitis.
a Noncontrast CT shows ventricular enlargement and bilateral occipital hypodensities, including a rounded hypodensity on the left side.
b A scan after intravenous contrast administration shows rimenhancing lesions in the left and right occipital areas. The left occipital abscess appears to have ruptured into the ventricular system. Note the enhancing ventricular wall and the additional enhancing foci to the left of the ventricle.
The early cerebritis stage may not enhance after contrast administration. These patients require serial examinations at close intervals. If the initial examination is delayed, it can be difficult to distinguish brain abscess from other lesions that show a ring pattern of contrast enhancement. Metastases, glioblastoma, and other etiologies should be considered. CT may direct attention to complications that require surgical intervention, such as extensive mass effect. As stated earlier, it is important to recognize subdural fluid collections with accompanying meningeal enhancement that would signify a subdural empyema. Dural sinus thrombosis is not uncommon. A deep abscess may rupture into the ventricular system, giving rise to ventriculitis, with contrast enhancement of the ventricular wall (Fig. 4.5).
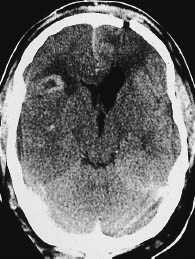
Fig.4.6 Abscess secondary to head trauma. This scan demonstrates a gaping fracture site in the left frontal calvarium. To the right of the frontal horn there is a ring-enhancing lesion, representing an abscess.
Among the various diseases that can produce a ring-shaped enhancement pattern, the features of brain abscess are often the most characteristic. Apart from the typical location of sinugenic abscesses, the ring itself tends to have distinctive features: it is usually thin, circular, and of uniform diameter. By contrast, glioblastoma usually has a scalloped rim, while small tumors tend to have an enhancing rim of varying thickness.
Tuberculosis
Frequency: once very rare, but the incidence has been increasing in recent years.
Suggestive diagnostic findings: basal meningitis.
Procedure: cerebrospinal fluid (CSF) examination.
Other studies: MRI is much more sensitive than CT for detecting meningitis (the most common pattern of CNS involvement).
Checklist for scan interpretation:
 Hydrocephalus?
Hydrocephalus?
 Meningeal enhancement? Enhancement in the basal cisterns?
Meningeal enhancement? Enhancement in the basal cisterns?
 Enhancement of the ventricular wall?
Enhancement of the ventricular wall?
 Enhancing lesions in the brain parenchyma?
Enhancing lesions in the brain parenchyma?
 Evidence of ischemic infarcts?
Evidence of ischemic infarcts?
 Pathogenesis
Pathogenesis
Cerebral or meningeal involvement by tuberculosis is almost always a result of hematogenous spread. The causative organism in nearly all cases is Mycobacterium tuberculosis. Most cases start as a pulmonary infection that spreads swiftly to other organs by the hematogenous or lymphogenous route.
The most common CNS manifestation of the disease is meningitis (Fig. 4.7) or meningoencephalitis.
Other manifestations of intracranial infection are abscess formation and the development of multiple tuberculomas. Involvement of the cranium itself is extremely rare.
Involvement of the meninges, ependyma, and choroid plexus is characterized histologically by typical inflammatory reactions and, in severe cases, by caseating necrosis. Cranial nerve involvement is very common, and even the optic nerve may be affected. When meningitis develops, the associated vasculitis can result in areas of infarction. A frequent complication is hydrocephalus, with its associated clinical manifestations.
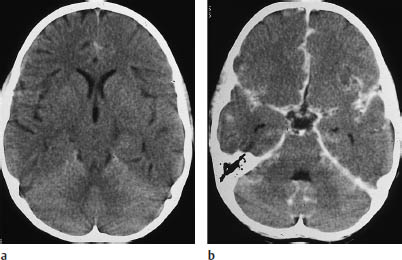
Fig.4.7a, b Meningitis.
a Noncontrast CT scan in a 10-year-old child shows no significant abnormalities.
b Scan after contrast administration shows ubiquitous enhancement of the meninges, particularly in the tentorium and sylvian fissure on the left side and within the interhemispheric fissure. Changes over the hemispheres are less clearly defined due to the proximity of the calvarium.
The incidence of tuberculosis has been rising, due in part to the increasing number of immunosuppressed patients. It is likely, therefore, that the incidence of CNS involvement by tuberculosis will also continue to increase.
 Clinical Manifestations
Clinical Manifestations
Headache and nuchal rigidity are seen initially. Cranial nerve involvement is frequent, and is manifested by corresponding deficits. Consciousness changes range from confusion to neuropsychiatric disorders.
Focal neurologic deficits may result from vasculitis-induced infarction or intracerebral tuberculomas. Hydrocephalus is a frequent complication caused by involvement of the basal meninges and manifested by headache, nausea, vomiting, and impaired consciousness.
Children are commonly affected.
Untreated, the disease has a fatal outcome. If treatment is initiated in time, the patient may recover, although cranial nerve deficits and focal neurologic symptoms may persist. Even with adequate treatment, however, some patients may develop an organic brain syndrome or epileptic seizures.
CSF examination is diagnostic, showing a low glucose concentration, elevated protein, and a threefold to fourfold increase in cellularity. Lumbar spinal puncture should be withheld if obstructive hydrocephalus is present.
 CT Morphology
CT Morphology
Hydrocephalus is a frequent complication in many patients and must be described. If basal meningitis is present, it is often manifested on CT by contrast enhancement in the basal cisterns (Fig. 4.8).
Brain infarction due to vasculitis, seen also in other forms of meningitis, can have various CT manifestations. The infarcts may be unilateral or bilateral, symmetrical or asymmetrical, and may involve the cortex and white matter in various combinations. Perforating arteries may be affected by vasculitis.
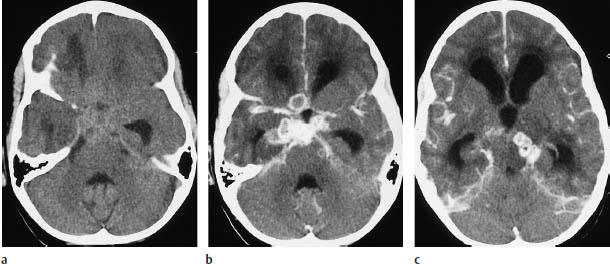
Fig.4.8a–c Tuberculous meningitis.
a Even plain CT in this 7-year-old child shows obliteration of the basal cisterns, with ill-defined hyperdensity.
b Scan after contrast administration shows the basal enhancement and ring-enhancing abscesses (mainly to the right of the midline) that are typical of tuberculous meningitis.
c Another abscess is compressing the brain stem from the left side. Hydrocephalus is also present.
 Differential Diagnosis
Differential Diagnosis
Meningeal enhancement on postcontrast CT, even when basal and occurring in a pediatric patient, is seen in various types of meningitis and is not pathognomonic for the tuberculous form. The same is true of ventriculitis. When nodular or ring enhancement is seen with tuberculomas, it is necessary to consider the entire spectrum of differential diagnoses for ring-enhancing lesions. There is no morphologic characteristic that is specific for tuberculosis.
Brain infarcts due to vasculitis may be seen in all forms of meningitis. It is important to recognize the infarcts and relate them causally to meningitis, which is not always associated with meningeal enhancement.
Sarcoidosis
Frequency: cerebral involvement is rare.
Suggestive morphologic findings: enhancing tissue in the basal cisterns, optic chiasm, and pituitary stalk.
Procedure: watch for lesion regression in response to cortisone therapy.
Other studies: MRI is more accurate for the sagittal and coronal localization of lesions.
Checklist for scan interpretation:
 Involvement of the hypothalamus or pituitary?
Involvement of the hypothalamus or pituitary?
 Hydrocephalus?
Hydrocephalus?
 Pathogenesis
Pathogenesis
Sarcoidosis may have an infectious etiology, but this is unproved. Pulmonary involvement is most common. CNS involvement is rare, with an incidence rate in single figures.
 Frequency
Frequency
Approximately 3% of patients with sarcoidosis show isolated CNS involvement with no apparent involvement of other organ systems.
 Clinical Manifestations
Clinical Manifestations
A great many patients with sarcoidosis also have diabetes insipidus. CNS involvement, including cervical cord disease, is very often misinterpreted as a tumor and is not correctly diagnosed until surgery. It is important to consider sarcoidosis in the differential diagnosis: the basal location of the lesions, together with involvement of the optic chiasm, should raise the possibility of sarcoidosis.
 CT Morphology
CT Morphology
CT after contrast administration shows enhancing, smoothly marginated tissue in the basal cisterns, which may extend into the brain parenchyma along small penetrating vessels. On the whole, the enhancing areas are clearly demarcated from the surrounding brain (non-caseating granulomas).
Unenhanced CT findings may be limited to nonvisualization of the basal CSF spaces.
The second major granulomatous disease, tuberculosis, may show features similar to those of sarcoidosis, but its clinical presentation is more dramatic. Low-grade primary brain tumors may also cause obstruction of the basal CSF spaces, in which case coronal MRI—e.g., using fluid-attenuated inversion recovery (FLAIR) sequences—can define the mass as originating in the brain parenchyma.
Herpes Simplex Encephalitis
Frequency: rare.
Suggestive morphologic findings: decreased density, followed in later stages by contrast enhancement and possible hemorrhagic imbibition in the mesial temporal lobe.
Procedure: immediate treatment.
Other studies: MRI is more sensitive than CT, especially for early detection, and is the imaging modality of choice. Single-photon emission computed tomography (SPECT) with 99mTc hexamethyl propyleneamine-oxime (HM-PAO) shows increased regional cerebral blood flow in the temporal region.
Checklist for scan interpretation:
 Decreased density in the sylvian fissure?
Decreased density in the sylvian fissure?
 Hemorrhages in that area?
Hemorrhages in that area?
 Give urgent recommendation for MRI.
Give urgent recommendation for MRI.
 Pathogenesis
Pathogenesis
Herpes simplex infections of the CNS are caused by two major types of organism: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2).
HSV-1, which persists in the gasserian ganglion and causes orofacial herpes, is responsible for encephalitis in adults.
HSV-2 causes genital herpes, and incites a diffuse encephalitis in neonates when transmitted from the infected maternal genitalia at birth. This diffuse encephalitis contrasts with the predominantly temporal-lobe encephalitis caused by HSV-1.
 Frequency
Frequency
Herpes encephalitis has an estimated annual incidence of one in 750000 to one in 100000. Males and females are affected equally.
 Clinical Manifestations
Clinical Manifestations
The HSV-1 organism resides in the oropharynx of approximately 95% of the adult population. HSV-1 encephalitis typically affects immunocompetent patients. HSV-2 encephalitis in newborns has an estimated incidence of one in 5000 to one in 10000 births. HSV-2 neonatal encephalitis has a poor prognosis, both in terms of survival and in the persistence of serious sequelae. Impaired consciousness is the clinical hallmark of herpes encephalitis in the acute stage. Often this is preceded by a prodromal stage, with lethargy, fever, and sore neck. Epileptic seizures are not uncommon. While the disease is usually fatal when untreated, the mortality rate with virostatic therapy has fallen to less than one-third. Today the diffuse neonatal form of encephalitis is seen increasingly in patients with acquired immune deficiency syndrome (AIDS), and early trial administration of virostatic drugs is replacing the former practice of brain biopsy.
 CT Morphology
CT Morphology
MRI has become the imaging modality of choice for herpes simplex encephalitis owing to its higher sensitivity. CT is used only as an initial imaging procedure in cases that have not yet been definitively diagnosed.
Both plain and postcontrast CT scans generally show no abnormalities during the first two days after the infection is acquired. Starting on about the third day, CT shows increasing hypodensity in the temporal lobe region (Fig. 1.19). After intravenous contrast administration, the lesions may show a diffuse, striate, or gyral/meningeal pattern of enhancement. The region may show swelling, with a mass effect on the ventricular system. Increased density due to hemorrhage has also been described. If the patient survives the herpes encephalitis, the primarily affected brain areas generally show extensive atrophic changes due to volume loss.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





