Infectious Inflammatory Diseases
Noninfectious Inflammatory Diseases
M. Loeffler
J. Wessling
Definition and Classification
Inflammation is defined as “a protective response in the living organism. […] It consists of a complex reaction of blood vessels, blood plasma constituents, and blood cells as well as cellular and structural components of the connective tissue that is elicited by local tissue injury” (Riede 1993). The purpose of inflammation is to inactivate or eliminate the causative injurious agent and repair the tissue injury. The causative agents of inflammation may be mechanical (foreign body, pressure, trauma), physical (ionizing radiation, UV light, heat, cold), chemical (lyes, acids, heavy metals), bacterial (toxins, allergens, immune complexes), or organic (microorganisms, helminths, insects). They also include abnormal metabolic products, dysfunctional enzymes, and malignant tumors. Diseases in which inflammation is the leading clinical problem have a profound economic impact. A survey by the German Ministry of Health found that inflammatory diseases were responsible for 22% of total healthcare costs (Federal Bureau of Statistics [Statistisches Bundesamt] 2004).
There is no uniform scheme for the classification of inflammation. Clinicians in various disciplines tend to view inflammations of specific organ systems in isolation while at the same time distinguishing between local and generalized inflammations. This is problematic for the pathologist, however, who recognizes that every inflammation, even if local, has a systemic component. For practical reasons and for convenience, therefore, the classification scheme used in this chapter will distinguish between infectious and noninfectious inflammations and between known and occult inflammatory foci (Table 3.1).
Tracers for Inflammation Imaging
FDG. The pathophysiology of inflammatory processes is accessible to FDG PET imaging. This is because inflammatory processes consume energy, causing metabolic markers such as [18F]DG to accumulate in macrophages and granulocytes. PET imaging localizes this accumulation in granulocytes, revealing the site of the inflammation. On the other hand, malignant tumors and other primarily noninflammatory diseases may also show increased glucose metabolism and frequently have an inflammatory component. As a result, the uptake of FDG is by no means specific for inflammation. Repeating the PET acquisition at a later time may be helpful in these cases: relative glucose uptake at sites of inflammation (measured as the standard uptake value, SUV) will diminish over time, whereas glucose uptake in malignancies will increase (Sahlmann et al. 2004).
Table 3.1 Clinical differentiation of various inflammatory conditions
| Occult sites of inflammation | |
| Fever of unknown origin (FUO) | |
| Known site of inflammation | |
| Infectious | Noninfectious |
|
|
99mTc leukocyte scans are effective for the early imaging of inflammation, but delayed scans acquired 24 hours PI show poor count rates due to the short tracer half-life. Moreover, enteric excretion by 4 hours PI may mask sites of abdominal inflammation.
111In leukocyte scintigraphy has relatively unfavorable imaging properties because only low activities can be administered due to the long half-life of the tracer.
Monoclonal anti-granulocyte antibodies (mAb) initially accumulate at sites where vascular permeability is increased due to inflammation and are therefore relatively sensitive but nonspecific. As murine antibodies, MAbs also have an affinity for anti-mouse antibodies. Only fractionated MAbs are exempt from this reaction.
The above tracers differ in their imaging characteristics. Given the limitations imposed by excretory path-ways, differences in specificity, or sensitivities limited to infectious granulocytic inflammations, selection of the proper imaging agent should depend on the type of inflammation being investigated.
Infectious Inflammatory Diseases
Fever of Unknown Origin
Definition. Fever of unknown origin (FUO) is present when the body temperature remains elevated above 38.3°C for more than 3 weeks and an inflammatory focus cannot be detected by conventional means (Petersdorf and Beeson 1961).
Etiology. FUO may be caused by infection, a noninfectious inflammatory condition (especially granulomatous inflammations, autoimmune diseases, and connective tissue diseases), or neoplasia. The prevalence of underlying diseases varies with patient age. Older patients are more likely to have vasculitis, tuberculosis, or neoplasms. The most common etiology in younger patients is infectious disease. Also, a conventional search for an inflammatory focus is more likely to be unrewarding in children (40% of cases) than in seniors (8%; Durak 1997).
CT. CT is an established modality that is used very early in patients with FUO. It is particularly effective for detecting pulmonary infiltrates, enlarged lymph nodes, abscesses, and granulomas.
Scintigraphy. Scintigraphic studies are usually performed only in cases where conventional tests have been equivocal or unrewarding. At the same time, the success of different scintigraphic methods depends on the type of inflammation, and so the clinical assessment of the underlying cause will direct the selection of an appropriate tracer (e.g., increased likelihood of infectious foci after surgery; focal symptoms). Labeled white blood cells (WBCs) can be used for infection imaging and are particularly useful in the diagnosis of postoperative inflammation. While a large percentage of noninfectious inflammations are not reliably detected by conventional scintigraphy, a negative scan would suggest a noninfectious etiology owing to its relatively high negative predictive value for an infectious cause.
FDG PET. Comparative studies using a narrower definition of FUO (no prior surgery) found that FDG PET was superior to other conventional scintigraphic techniques. In a study of 118 patients with FUO, FDG PET contributed to the diagnosis in 36% of the cases (Jaruskova et al. 2006). Only eight of the 51 positive findings were false-positive. The origin of the fever could not be ascertained in 67 patients. In another study of 16 patients, FDG PET had a sensitivity of 85% in detecting the cause of FUO (Lorenzen et al. 2001). FDG PET was false-positive in one patient and was predictably negative in two patients with rheumatic fever (Lorenzen et al. 2001).
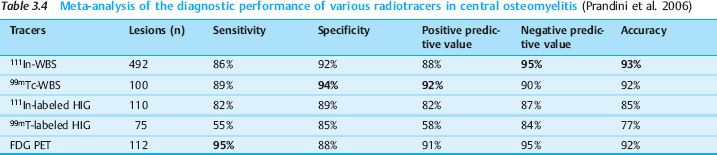
In another study of 35 patients, PET had a reported sensitivity of 93% and a specificity of 90% (Bleeker-Rovers et al. 2004). Table 3.2 reviews the diagnostic performance of various tracers based on a meta-analysis of patients with FUO (Cascini et al. 2006; Dumarey et al. 2006). Comparison of the data shows some degree of variation in the inclusion criteria. Compared with the complex procedure of leukocyte scintigraphy, FDG PET has higher sensitivity, lower specificity, and comparable accuracy. Because high sensitivity is a priority in the clinical setting, FDG PET is therefore to be preferred over leukocyte scans. Ferda and coworkers reported a sensitivity of 97% (43/44) and a “specificity” of 75% (3/4) for FDG PET-CT (Ferda et al. 2009). Another prospective study in 48 patients showed that PET-CT identified the underlying cause of inflammation in 46% of patients and contributed to the diagnosis or exclusion of disease in 90% of patients (Keidar et al. 2008).
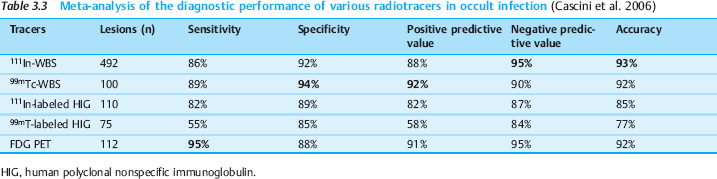
In patients evaluated specifically for postinterventional inflammation, imaging with labeled WBCs acquires a higher sensitivity owing to the greater likelihood of an infectious cause. Nevertheless, the above meta-analysis indicates that FDG PET is still more sensitive for this indication while providing the same accuracy. In an analysis of 55 studies, FDG PET achieved a sensitivity of 100% and a specificity of 89% (Bleeker-Rovers et al. 2004). Just as in FUO, then, FDG PET is also useful in the investigation of occult infections (Fig. 3.1). In a larger study it was demonstrated that FDG PET-CT is a valuable diagnostic tool for the evaluation of children with FUO and unexplained signs of inflammation. The combination of PET with CT was superior, since the site of inflammation can be localized more accurately. In 69 children 45% of the scans were helpful (Jasper et al. 2009). The results are summarized in Table 3.3.
Osteomyelitis
Bone infection primarily localized to the medullary cavity is a systemic disease with organ manifestations. Also known as hematogenous osteomyelitis, this condition is distinguished from secondary osteomyelitis in which local local bone inflammation develops as a result of trauma or surgery. While children are more likely to develop the acute form of osteomyelitis without a definite portal of entry for infection (most likely nasopharyngeal), chronic osteomyelitis is more common in elderly patients. The diagnosis is generally based on multimodal tests that may include conventional radiographs, ultrasonography, CT and, increasingly, MRI. Nuclear medicine imaging is most commonly used for evaluating acute cases. Data on the performance of nuclear medicine techniques are limited by the frequent failure in the literature to distinguish between chronic and acute osteomyelitis. In studies on FDG PET, however, reported sensitivities and specificities do not show significant differences between the acute and chronic forms.
Acute osteomyelitis. The radiographic changes of acute osteomyelitis often take time to develop, and initial X-ray films may be negative. MRI, labeled WBCs, or FDG PET can generally detect acute osteomyelitis at an early stage (Gold et al. 1991; Mahnken et al. 2000). The sensitivity of FDG PET for this application is as high as 100% (Sugawara et al. 1998). FDG PET can be particularly useful in cases where postoperative changes (especially metal implants) hamper the detection of inflammatory changes by CT or MRI (Bessette et al. 1993).
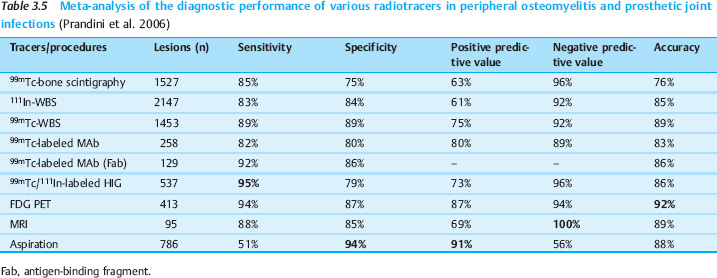
While WBS is roughly equivalent to FDG PET when used at peripheral sites (sensitivity up to 83%), central inflammatory foci are often missed due to the physiologic uptake of labeled WBCs by the bone marrow (Sugawara et al. 1998). Perfusion also has a greater impact on WBC scans than on FDG PET scans. Especially in cases of spinal inflammation, the inflammatory foci often appear as nonspecific cold spots on WBC scans due to a pressure-induced decrease in perfusion.
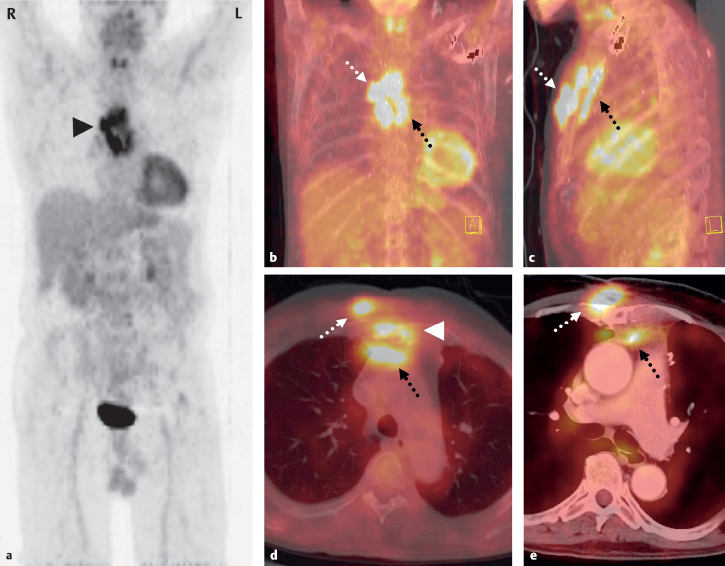
Fig. 3.1 a-e Sternal osteomyelitis and soft-tissue abscesses in a 71-year-old man 2 years after aortocoronary venous bypass. A small fistula remained following surgical repair of an inflammatory soft-tissue defect in the lower part of the sternum. Due to the protracted but marked physical deterioration of the patient, a complete sternectomy was proposed. The preoperative workup included PET-CT to evaluate lesion extent. PET MIP (a frontal) and PET-CT MIP (b frontal, c lateral) show florid inflammatory foci anterior (dotted white arrows) and posterior to the sternum (dotted black arrows). The foci are also visible in axial scans (d PET-CT with bone-window CT, e PET-CT with soft-tissue window CT), but the sternum itself shows only very limited involvement (d, arrow-head). As a result, the sternum was simply explored and inflammatory tissue was removed by local excision. The soft-tissue abscesses were also confirmed intraoperatively and evacuated. Operative treatment was followed by marked clinical improvement.
For this reason, FDG PET is superior to WBS for detecting central involvement. Table 3.4 summarizes the results of a meta-analysis on the diagnostic value of nuclear medicine techniques for imaging central osteomyelitis (Prandini et al. 2006). The accuracy of 92%–93% was equivalent to that of WBS. On current data, FDG PET is preferred over leukocyte scans because it has comparable performance, tracer synthesis is easier, and examination time is shorter. No data have yet been published on the PET-CT imaging of central osteomyelitis.
Chronic osteomyelitis. Chronic osteomyelitis often develops over a prolonged period. It may take months or even years for acute or subacute osteomyelitis to reach a chronic stage. Primary chronic hematogenous forms of osteomyelitis may also occur (e.g., Brodie abscess, chronic recurrent multifocal osteomyelitis). The clinical picture is often remarkable for the paucity of symptoms (Petersdorf and Beeson 1961).
Reparative processes are the dominant radiographic finding in chronic osteomyelitis. The main goal of imaging in these cases is to detect or exclude new inflammatory foci and sequestra. A negative FDG PET scan reliably excludes chronic osteomyelitis (sensitivity 100%, negative predictive value 100%, specificity 62%–88%). However, with a positive predictive value of 75%–92%, not every area of increased FDG uptake indicates inflammation (Zhuang et al. 2000; Schmitz et al. 2000; Schmitz et al. 2001). Previous surgery is a very common source of falsepositive activity. When the surgical history is known and examiners are not blinded as in studies, however, PET should achieve a higher specificity in routine clinical settings.
FDG PET is reported to have a high sensitivity (100%), superior to that of bone scintigraphy, and a relatively high specificity of 92%. Another advantage of FDG PET is its ability to distinguish between primary bone inflammation and perifocal soft-tissue infection (Guhlmann et al. 1998a, 1998b; Kälicke et al. 2000). Initial reports show that a decline of inflammatory activity in response to antibiotic therapy correlates well with a decrease in FDG uptake. Case numbers and follow-ups are still too small, however, to make a definitive assessment of the clinical importance of FDG PET for evaluating the response of chronic osteomyelitis to therapy (Schmitz et al. 2000; Kälicke et al. 2000).
Prosthetic Joint Infections
Infection of a prosthetic joint is a special form of chronic osteomyelitis. Because the bacterial flora on the surface of the prosthesis are not accessible to effective antibiotic therapy, an urgent indication exists for explantation of the prosthesis. Conventional limb radiographs can detect zones of periprosthetic resorption and gas inclusions. Sectional imaging modalities, particularly CT, can further advance the diagnosis. Today, the limitations formerly imposed by metal-induced beam-hardening artifacts have been largely eliminated by special postprocessing algorithms.
Metal artifacts have very little impact on nuclear medicine imaging. Metal implants absorb only a negligible portion of the emissions and cause an insignificant amount of scatter. FDG PET images should, however, be reconstructed without attenuation correction to avoid correction artifacts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 FDG PET has high sensitivity but low specificity in the detection of inflammation.
FDG PET has high sensitivity but low specificity in the detection of inflammation. Scintigraphy has a high negative predictive value for infectious inflammation.
Scintigraphy has a high negative predictive value for infectious inflammation. FDG PET is superior to conventional scintigraphy in patients with FUO.
FDG PET is superior to conventional scintigraphy in patients with FUO. FDG PET is preferred over WBS in FUO because of its high sensitivity.
FDG PET is preferred over WBS in FUO because of its high sensitivity.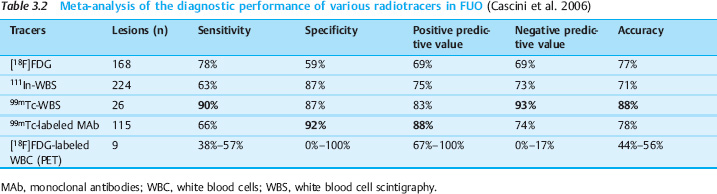
 Initial radiographs may be negative in acute osteomyelitis.
Initial radiographs may be negative in acute osteomyelitis. FDG PET is superior to WBS for the imaging of central osteomyelitis.
FDG PET is superior to WBS for the imaging of central osteomyelitis.