Inflammatory Joint Diseases
Michel Court-Payen
Marcin Szkudlarek
Ian Beggs
INTRODUCTION
Ultrasound is increasingly used as a diagnostic modality in joint imaging by radiologists and rheumatologists. Several factors explain this development. Technical advances have improved image quality, simplified equipment, reduced cost, and improved diagnostic capability. New, highly effective treatments have become available that control joint inflammation and prevent or retard long-term joint damage, but early diagnosis of pre-destructive soft tissue changes is critical and best achieved by magnetic resonance imaging (MRI) or ultrasound. With the exception of pre-erosions (subcortical bone edema) and assessment of articular cartilage, MRI and ultrasound are equally effective in the diagnosis of inflammatory arthropathy.1 Ultrasound is more operatordependent than MRI and cannot always access all parts of a joint (e.g., between metacarpal heads). However, ultrasound has better spatial resolution than MRI in superficial areas, can be used to scan multiple joints and sites quickly, and readily distinguishes effusion from synovitis without needing intravenous contrast. Ultrasound is now viable as a diagnostic tool for office-based practice and for this reason has been adopted by many rheumatologists in their routine practice.
In this chapter we will present the ultrasound technique and criteria for examining patients with arthropathies, and discuss initial diagnosis and follow-up. We will discuss the ultrasound findings in conditions that target the synovial membrane (e.g., rheumatoid arthritis, juvenile idiopathic arthritis, and crystal arthropathies); inflammatory arthropathies that target both entheses and synovial membrane (spondyloarthopathies); and other arthropathies (osteoarthritis, pigmented villonodular synovitis, synovial osteochondromatosis, amyloid, septic arthritis, and hemophiliac arthropathy). Finally, we will describe ultrasound-guided interventions.
Although the cost of ultrasound equipment has reduced considerably in real terms, high-quality equipment remains essential. High-frequency (>10 MHz) linear array transducers are essential, although larger joints may need curvilinear transducers and lower frequencies. Small footprint transducers are useful for the small joints of the hands and feet. A standoff is not required, but copious jelly helps. Beam steering and compound imaging are also useful. Joints should be relaxed when examined, and transducer pressure should be light or fluid may be displaced and missed or vascularity effaced.
Tip:
Use light transducer pressure or fluid or hyperemia may be missed.
New developments are being assessed for possible roles in joint disease: 3D imaging (possible quantification of the volume of inflamed synovium, regional vessels, or erosions); intravenous contrast agents (improved visualization of vascularity); elastography (compressibility of soft tissues); and fusion imaging (direct correlation of ultrasound to computed tomography [CT] and/or MRI). As yet, no practical applications for these techniques have been established in routine rheumatological practices.
Standardization of technique and diagnoses has been facilitated by the adoption of a number of consensus definitions2:
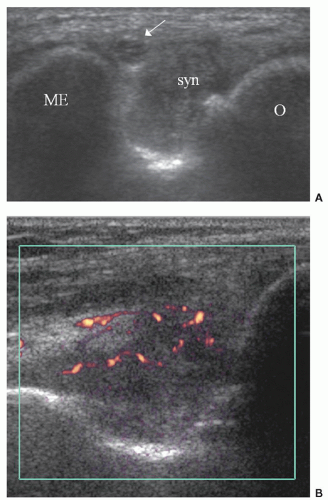
Synovial fluid: Intra-articular material that is displaceable and compressible and does not exhibit Doppler signal. It is usually anechoic (Fig. 10.1) or hypoechoic but may be hyperechoic.
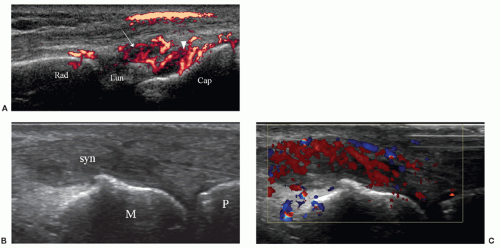
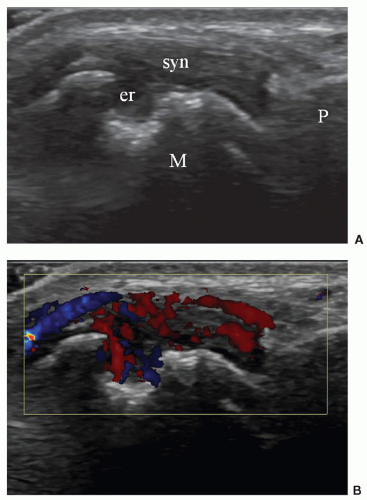
Synovial hypertrophy: Abnormal intra-articular tissue that is not displaceable and is poorly compressible. It may/may not exhibit Doppler signal and is usually hypoechoic (Figs. 10.2 and 10.3).
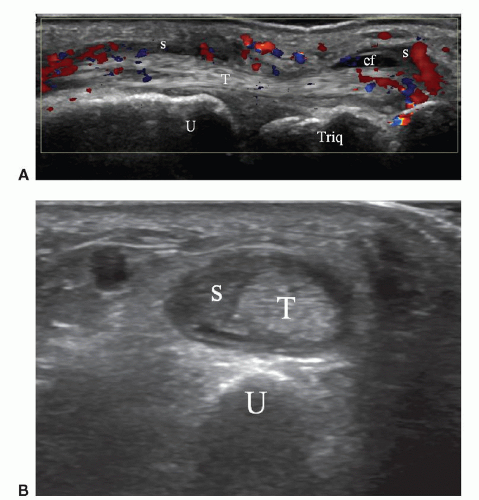
Tenosynovitis: Thickened tissue (+/− fluid) within a tendon sheath seen in two perpendicular planes. It may/may not exhibit Doppler signal and is usually hypoechoic (Figs. 10.4 and 10.5).
Bone erosion: An intra-articular discontinuity in the bone surface that is visible in two perpendicular planes (Fig. 10.6).
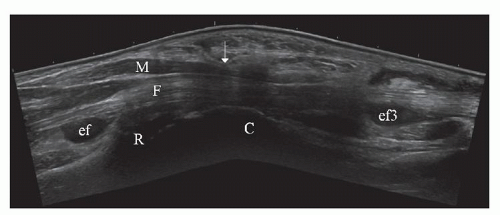
Enthesopathy: Abnormally hypoechoic and/or thickened tendon or ligament at its bony attachment with loss
of the normal fibrillar pattern seen in two perpendicular planes. Echogenic foci due to calcification, Doppler signal, and bony changes (due to enthesophytes, erosions, or irregularity) may be present.
of the normal fibrillar pattern seen in two perpendicular planes. Echogenic foci due to calcification, Doppler signal, and bony changes (due to enthesophytes, erosions, or irregularity) may be present.
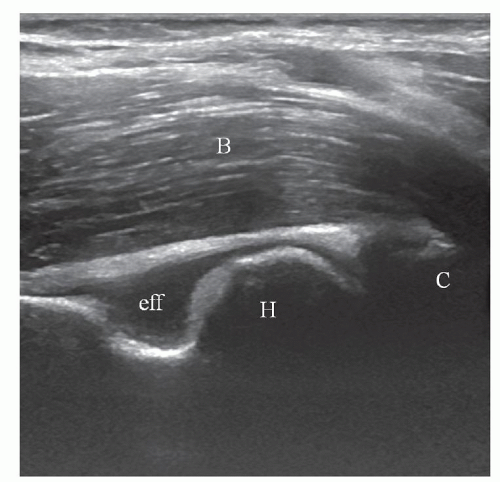 Figure 10.1. Longitudinal scan of anterior elbow. Anechoic effusion (eff) in anterior recess. B, brachialis muscle; C, coronoid process of ulna; H, humerus. |
In clinical practice, the diagnosis of “active arthritis” (or clinical synovitis) is based primarily on clinical evaluation, but it is often difficult to determine whether
joint pain, swelling, and/or limitation of mobility are caused by synovitis, tenosynovitis, enthesitis, or periarticular edema. Ultrasound has become a valuable adjunct in rheumatology. Ultrasound examination of joints demonstrates with high accuracy most of the anatomical structures involved: synovial recesses, articular/periarticular bone contours, ligaments, tendons, and tendon sheaths (including the bony insertions or entheses of ligaments and tendons), and bursae. Ultrasound can demonstrate inflammatory changes (hyperemia, synovial thickening, or effusion in joint recesses, bursae, or tendon sheaths) and destructive changes (bone erosions, joint destruction or ankylosis, cartilage loss, and tendon tears).
joint pain, swelling, and/or limitation of mobility are caused by synovitis, tenosynovitis, enthesitis, or periarticular edema. Ultrasound has become a valuable adjunct in rheumatology. Ultrasound examination of joints demonstrates with high accuracy most of the anatomical structures involved: synovial recesses, articular/periarticular bone contours, ligaments, tendons, and tendon sheaths (including the bony insertions or entheses of ligaments and tendons), and bursae. Ultrasound can demonstrate inflammatory changes (hyperemia, synovial thickening, or effusion in joint recesses, bursae, or tendon sheaths) and destructive changes (bone erosions, joint destruction or ankylosis, cartilage loss, and tendon tears).
Most of the early studies that described the ultrasound findings in inflammatory arthropathy were performed on patients with rheumatoid arthritis (RA), but these findings are not specific and can be found in most types of joint diseases.
EXAMINATION TECHNIQUE
In general, joints are best examined with long-axis scans to show the joint recesses. Tendon sheaths are best studied in short axis when the transducer can be moved proximally and distally, employing an “elevator” technique. Bursae and Baker cysts are shown in two planes. Typical sites of synovitis include the ulnar aspect of the
wrist, the metacarpophalangeal joints (MCPJs) especially the dorsal margins, and the suprapatellar recess of the knee.
wrist, the metacarpophalangeal joints (MCPJs) especially the dorsal margins, and the suprapatellar recess of the knee.
Hand and Wrist
The hand/wrist is the area most frequently examined for inflammatory arthropathy. Ultrasound anatomy and technique have been described in Chapter 5 and will not be repeated in detail here, but a systematic approach to the examination is essential. The thumb and interphalangeal joints are not usually included unless there is a specific indication. By moving the transducer slowly, the entire examination can be performed as a combined grayscale and Doppler procedure.
Start by examining the dorsal aspects of the second to fifth MCPJs with the hand pronated, fingers extended, and the transducer placed longitudinally (Fig. 10.7). Flexion at the wrist or MCPJs reduces the conspicuity of both grayscale and Doppler evidence of synovitis.3 With grayscale and Doppler gain and focal zone suitably adjusted, examine each joint in turn by moving the transducer slowly backward and forward from medial to lateral. At the second and fifth MCPJs, respectively, continue the movement to examine the radial and ulnar aspects of the joints.
Tip:
The wrist and MCPJs should be extended when examined to optimize conspicuity of synovitis.
Now place the transducer transversely on Lister tubercle to examine the second to fifth extensor compartments before internally and externally rotating the wrist to examine the sixth and first extensor compartments, respectively. In each position, an “elevator” technique is employed by moving the transducer to and fro, proximally and distally. The transducer is then rotated through 90 degrees on the dorsal aspect of the carpals and again moved backward and forward, from radial to ulnar, to examine the wrist and midcarpal joints. The hand is then supinated and the transducer placed transversely across the carpal tunnel and moved proximally and distally looking for evidence of flexor tenosynovitis. Finally, the volar aspects of the second to fifth MCPJs are examined in similar fashion to the dorsal aspects.
Foot and Ankle
A similar approach to the hand/wrist is used. The dorsal and plantar aspects of the metatarsophalangeal (MTP) joints and the dorsal midfoot are examined with the transducer placed longitudinally. The medial, peroneal, and anterior tendons at the ankle are examined transversely using a proximal and distal elevator technique, and the anteromedial and lateral gutters are also examined transversely.
Other Joints
Although long-axis scans of joints are usually preferred, short-axis scans can be useful, for example, in looking for fluid or synovitis in the medial and lateral pouches of the suprapatellar recess of the knee.
ULTRASOUND FINDINGS IN INFLAMMATORY JOINT DISEASES
Synovitis
Detection of synovitis is important because synovitis precedes bone erosions. Ultrasound is better than clinical examination and radiographs, and comparable to MRI in detecting synovitis.1 Synovial hypertrophy and joint fluid are both frequently present (Fig. 10.8). Normal synovium is so thin it is not seen with ultrasound. Synovial hypertrophy produces solid, noncompressible, thickened hypoechoic tissue in joints and tendon sheaths.2,4,5 The echogenicity of the thickened synovium is inversely proportional to its water content: the more fluid that is present, the less echogenic the synovium. A semiquantitative grading system (normal/mild/moderate/large) for synovial hypertrophy may be employed.6 Joint or tendon sheath fluid is usually anechoic or hypoechoic, and compressible. A complex or echogenic appearance is due to proteinaceous fluid, crystals, or debris. Even in large and easily palpable joints such as the knee, ultrasound is more sensitive in detecting fluid than clinical examination or radiographs.7,8 Volumes as small as 1 mL
and interobserver agreement of 79% can be found in small joints of the hands and feet.8
and interobserver agreement of 79% can be found in small joints of the hands and feet.8
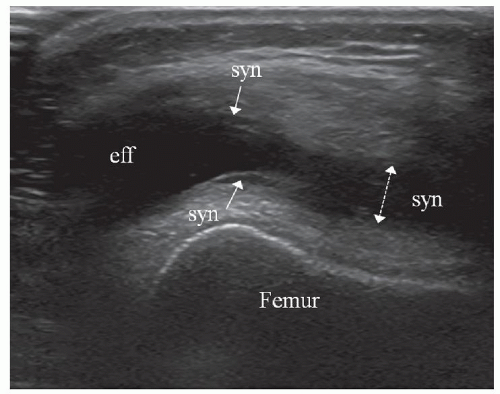 Figure 10.8. Transverse scan of suprapatellar recess of knee. Transducer pressure on right of image displaces fluid to left and distinguishes effusion (eff) from synovial hypertrophy (syn). |
In patients with doubtful hypoechoic or anechoic areas in superficial joints, compression with the transducer9 distinguishes between synovial hypertrophy (poorly compressible, non-displaceable) and effusion (compressible, displaceable) (Fig. 10.8). This does not work for deep joints like the hip.
Tip:
Joint fluid is compressible and displaceable. Synovial thickening is poorly compressible and non-displaceable.
Synovial hypertrophy occurs in both acute (inflammation) and chronic (fibrosis) stages of inflammatory joint disease, and it is not possible to distinguish between them using grayscale ultrasound. Doppler techniques (color or power Doppler) are therefore widely employed for diagnosis and follow-up of arthritic joints.
Tip:
Use Doppler to distinguish between active and chronic (inactive) synovitis.
Doppler techniques detect tissue hyperemia, which is associated with disease activity (Figs. 10.2 and 10.3). Some authors use power Doppler. Depending on the sensitivity of the ultrasound equipment, others prefer color Doppler. Synovial hyperemia on Doppler ultrasound correlates well with contrast enhancement on MRI10,11 and microvascular density on histology.12 Synovial tissue may be seen extending into erosions (Fig. 10.6), sometimes with vascular signal,13 probably related to erosion activity (Fig. 10.6). Fluid does not show Doppler signal and this helps to distinguish active synovitis from fluid. Light transducer pressure is essential as even moderate pressure may efface vessels and flow.
Intravenous injection of ultrasound contrast has been used to increase the sensitivity of Doppler examinations.10,14,15 However, the sensitivity of current generation ultrasound machines has improved dramatically, even without contrast enhancement, and with high-end units it is now possible to display physiological joint flow.16 The use of intravenous ultrasound contrast increases the cost and time of the examination, and is invasive. Contrast is not used in routine clinical practice although it has been shown to improve the diagnosis of sacroiliitis.17
Doppler findings5 can be reported in three different ways: qualitative assessment, semiquantitative grading, and quantitative assessment. Qualitative assessment is a simple report of the presence or absence of synovial flow. Semiquantitative scoring is the most often used technique in daily practice10,13 and employs a grading scale depending on the severity of findings.1 Quantitative assessment18,19 is time-consuming but is more precise and is used for trials. It is performed by calculating the number of pixels showing power Doppler signal or by calculating the resistive index from spectral Doppler measurements. Future ultrasound systems may provide automatic measurements.
Bony Changes
Ultrasound of articular and periarticular bone surfaces can display erosions (Fig. 10.3), which are important signs in aggressive arthritis such as RA. Erosions are not disease-specific and can occur in other types of inflammatory joint disease. Small bone defects resembling erosions can be found in healthy controls.20 Erosions typically occur in the bare area of a joint (i.e., the intracapsular cortex that is not covered by hyaline cartilage) and are seen as focal cortical defects identified in two perpendicular planes. Active erosions may show Doppler signal (Fig. 10.6).
Tip:
Erosions usually occur at the bare area of a joint.
Ultrasound is more sensitive than radiographs and comparable to MRI in detecting erosions in fingers21,22 or toes.1 The specificity of ultrasound is lower than that of CT, probably because small cortical defects occur as normal findings. Some studies have found ultrasound to be less sensitive in detecting erosions than MRI,23 possibly because of inaccessibility (e.g., on the lateral and medial margins of metacarpal and metatarsal heads or at the wrist joint).1,22 A drawback of ultrasound is that it cannot detect bone marrow edema, which has been
shown to be an important prognostic factor on MRI. Bone erosions in early undifferentiated arthritis increase the risk of developing persistent arthritis.23
shown to be an important prognostic factor on MRI. Bone erosions in early undifferentiated arthritis increase the risk of developing persistent arthritis.23
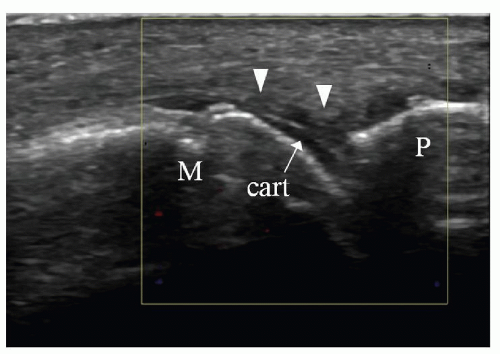
Cartilage Changes
Normal hyaline or articular cartilage forms a hypoechoic layer that covers the bright surface of the subchondral bone plate. Its thickness can be measured by ultrasound.9 The superficial surface of normal cartilage is seen as a smooth, thin echogenic line. In inflammatory and degenerative joint diseases, nonspecific destructive cartilaginous changes can be detected with diffuse or focal thinning (Fig. 10.9), irregularity of the surface, or defects.
Tenosynovitis
In tenosynovitis, hypoechoic or anechoic fluid and/or synovial proliferation are seen around the tendon in the tendon sheath. Synovial hypertrophy may be nodular and show abnormal Doppler signal. Tendinopathy (with or without tenosynovitis) is defined by intratendinous changes: hypoechoic thickening best demonstrated on transverse scans, and disorganization of the fibrillar tendon structure best seen on longitudinal scans. Paratendinitis is an inflammatory thickening of the para-tendon, which can be pronounced in some arthritides (RA, crystal or infectious arthritides, and juvenile idiopathic arthritis). Tendon tears are defined by areas of interruption of tendon fibers and may be partial (transverse or longitudinal with tendon split) or complete (transverse tears). In aggressive inflammatory joint diseases such as RA, synovial tissue can enter tendon erosions, similarly to bony erosions.
Enthesitis
Enthesopathy refers to a pathological condition at the bony attachment of tendons, ligaments, capsule, or fascia, and can be mechanical or secondary to an inflammatory process (enthesitis). Enthesitis is characteristic of sero-negative spondyloarthropathies such as ankylosing spondylitis and psoriasis. Signs of inflammation in the spondyloarthropathies are more frequent at insertion sites than in the synovial membrane of joints or tendon sheaths. This is the opposite of RA24 and is useful when considering the differential diagnosis, although a specific diagnosis cannot be achieved with ultrasound alone.
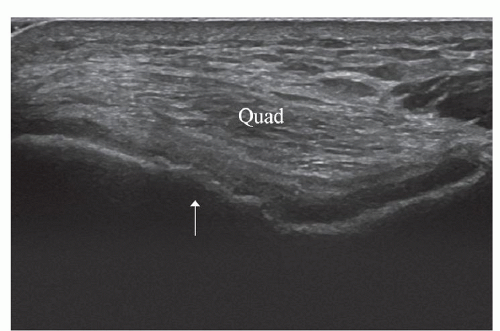 Figure 10.9. Transverse scan of femoral trochlea with knee in full flexion. Cartilage thinning and irregular hyperostosis are present on lateral aspect of trochlea (arrow). Quad, Quadriceps tendon. |
Tip:
Enthesitis is characteristic but not pathognomonic of seronegative spondyloarthropathy.
The presence of inflammation at insertion sites is difficult to assess clinically. Radiographs show bony changes (enthesophytes, bony irregularity, and erosions) and tendon calcification at a late stage, often only after many years of symptoms.25 Ultrasound and MRI can demonstrate the early soft tissue signs of inflammation. Ultrasound shows the soft tissue part of insertion sites in greater detail than MRI, especially at small structures, and is a helpful adjunct to clinical examination. Ultrasound shows focal hypoechoic thickening of the tendon insertion in two orthogonal planes, sometimes with hyperemia, calcifications, or bony changes.2 Adjacent bursae may also be inflamed (e.g., enthesitis of the Achilles tendon and retrocalcaneal bursitis). As ultrasound can show only the surface of bone at an enthesis, local bone edema is not detectable, and this is a disadvantage compared with water-sensitive MRI sequences (STIR, fat-suppressed T2-weighted) or fat-suppressed contrast-enhanced T1-weighted sequences.26 However, only large calcifications or spurs can be seen on MRI, whereas ultrasound shows even small enthesophytes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree