Soft Tissue Masses
Jon A. Jacobson
David P. Fessell
INTRODUCTION
Ultrasound is routinely used to evaluate palpable soft tissue masses.1 Ultrasound differentiates cystic from solid masses, which often require biopsy to exclude malignancy,2 and can identify superficial soft tissue tumor margins and local tumor spread.3 Limitations primarily relate to evaluation of deep soft tissue structures, bone, and masses that calcify or ossify, casting acoustic shadows that obscure deeper structures.
Advantages of ultrasound include direct correlation of symptoms and physical examination with imaging. Palpation during ultrasound imaging, “sonopalpation,” is the ultrasound correlate of physical examination. Additional history gained during the ultrasound examination often adds insight to narrow the differential diagnosis. Ultrasound is less expensive and more accessible than magnetic resonance imaging (MRI). Color and power Doppler may help distinguish between cystic and solid masses and characterize malignant masses and lymph nodes. Ultrasound can guide percutaneous biopsy, particularly useful with masses near neurovascular structures or the pleura where real-time imaging during biopsy is necessary.
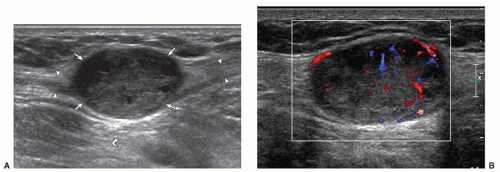
While ultrasound is primarily used to discriminate between cystic and solid masses, there are often features that can limit the differential diagnosis. The first critical distinction is to determine whether the mass originates from a synovial space (joint, bursa, or tendon sheath), as such masses are likely benign and related to a synovial process. A mass that originates in other soft tissues could be benign or malignant. Most malignant masses are predominantly hypoechoic, usually with low-level echoes or heterogeneity, and well defined as they have pseudocapsules. As a malignant mass enlarges, especially if high grade, it becomes more heterogeneous with hypoechoic areas of internal necrosis and increased flow on color and power Doppler imaging. Tumors with a significant myxoid component (myxoid liposarcoma, intramuscular myxoma) can be predominantly hypoechoic and have the appearance of a heterogeneous cyst. Many solid masses demonstrate increased through-transmission, simulating complex cysts.4 The presence of an echogenic and shadowing focus requires radiography to evaluate for calcification or ossification. Ultrasound is accurate in the diagnosis of sarcoma and melanoma local recurrence.5,6,7
Color Doppler imaging has been used to characterize masses and tumor vascularity.8 Aggressive tumors tend to have more flow on color and power Doppler imaging than benign tumors. However, hypervascular benign tumors such as peripheral nerve sheath tumors do occur.9,10 Extreme vascularity of a hypoechoic soft tissue mass in the absence of necrosis is characteristic of lymphoma. Increased flow is also characteristic of vascular malformations and vascular tumors. Because of the overlap between lesions on Doppler, including spectral Doppler, ultrasound cannot reliably differentiate between benign and malignant masses.11 Ultrasound contrast agents have been used to characterize the vascularity of soft tissue tumors,12 but no role has been established for contrast agents.
In evaluating a soft tissue mass of the extremity, a differential diagnosis can be organized based on location of the mass and age of the patient,13,14 and a short list of probable etiologies can be generated. This information is helpful when characterizing the mass with imaging, as imaging features are often in part explained by the histology of the tumor. The World Health Organization (WHO) classifies tumors by their histologic differentiation.15,16 The ultrasound description of masses in the subsequent text will in part follow this classification scheme.
ULTRASOUND TECHNIQUE
Diagnostic
Examination technique is important when performing ultrasound of a soft tissue mass. Hold the transducer at its footprint, and anchor the probe to the patient with the side of the hand or fingers. This will stabilize the transducer, allow fine movements, and help to assess how much pressure is being placed with the transducer. Excessive pressure may obscure the margins of a soft tissue mass or compress a fluid component. Ideally, a variety of probe pressures should be used. Floating the transducer on a thick layer of gel helps to demonstrate soft tissue swelling or a very superficial mass. The application of
pressure can show if a mass is pliable (such as a lipoma) and differentiates a fluid component (which is compressible) from an area of heterogeneous soft tissue. When assessing vascularity with color or power Doppler imaging, the application of pressure via the transducer may also obscure flow.
pressure can show if a mass is pliable (such as a lipoma) and differentiates a fluid component (which is compressible) from an area of heterogeneous soft tissue. When assessing vascularity with color or power Doppler imaging, the application of pressure via the transducer may also obscure flow.
Tip:
Use pressure to distinguish fluid (which is compressible and can be displaced) from solid tissue.
Avoid heavy pressure when performing Doppler examinations, or vascularity may be effaced or reduced.
Interventional
While a complete review of interventional techniques as they relate to soft tissue masses is beyond the scope of this chapter, several general points deserve emphasis. Ultrasound is ideal for guiding soft tissue biopsy or aspiration, especially when the mass is small and superficial17,18 or adjacent to a vital structure, such as an artery, where real-time imaging during the biopsy is important.19 While there are various techniques to guide needles with ultrasound, the in-plane approach with the needle parallel to the transducer is most accurate and shows the full length of the needle and its trajectory in real time. Needle visualization is improved when the sound beam is perpendicular to the needle to eliminate anisotropy. Typically three to five samples are obtained from various regions of the mass including the center and periphery, typically with a 16G or 18G needle. Fine needle aspiration generally does not provide diagnostic material, but may be helpful when performing a biopsy of a necrotic tumor, where soft tissue cores may not yield solid tissue, when the soft mass is small or in a critical location such as a pleural mass, or when recurrent or metastatic tumor is suspected. Discussion with the surgical oncologist prior to the biopsy is essential with regard to the approach and needle path as surgery often occurs along the biopsy needle path, which is also resected. Many centers perform local MRI staging prior to biopsy.
Tip:
Do not biopsy a soft tissue mass without first discussing the needle approach with the surgical oncologist.
Confirmation of a malignant tumor typically initiates staging with thoracic computed tomography (CT) and possibly an isotope bone scan to identify potential metastases. Positron emission tomography (PET) scanning is generally restricted to a few rare tumors such as alveolar rhabdomyosarcoma that metastasize to unusual sites. Staging and histology help to determine whether and what type of surgery and adjuvant radiation or chemotherapy are employed.
SOFT TISSUE MASSES
Lipomatous Tumors
Lipoma
Lipomas are benign fatty tumors. They are common, have a prevalence of 2.1%, and account for nearly half of all soft tissue masses.20 Frequent locations include the shoulder region and back.20 Lipomas are often present for many years with little or no growth. Malignant transformation is nonexistent with no metastatic potential.20 A lipoma may become clinically apparent when a patient loses weight and the surrounding fat decreases. Most lipomas occur in the subcutaneous fat and are <5 cm in diameter.20 Intramuscular or intermuscular lipomas, referred to as deep lipomas, are less common.20 Lipomas are multiple in 5% to 15% of cases, typically in males.20
In general, a lipoma is a discrete and homogeneous fatty mass that has similar imaging features to adjacent subcutaneous fat (Fig. 9.1). Superficial lipomas are usually encapsulated, while deep lipomas may have microscopic invasion of adjacent muscle tissue.20 Other than fatty elements, a lipoma may contain thin fibrous septations.
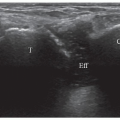
Ultrasound evaluation largely depends on the location of the lipoma. Superficial lipomas are typically oval or oblong, well defined, compressible, and show no flow on color or power Doppler imaging (Fig. 9.2). Echotexture varies from hypoechoic to hyperechoic relative to the surrounding subcutaneous fat. Pure fat is essentially free of echoes.21 Echogenicity is related to the fibrous component that increases the echogenic interfaces (Figs. 9.3 and 9.4).22 A blood vessel coursing through a lipoma should not be interpreted as neovascularity. Any unusual features on imaging, history, or physical examination warrant MR imaging. Otherwise, ultrasound may be considered as a follow-up if symptoms change.
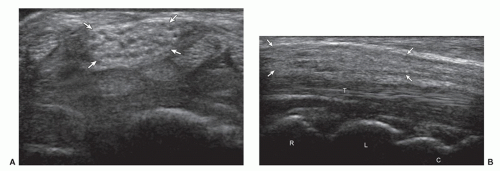
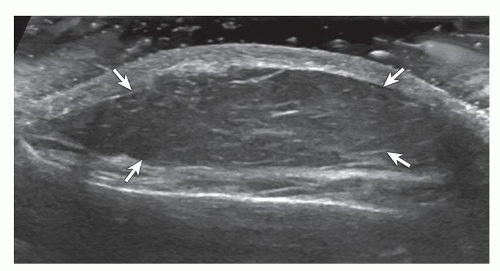 Figure 9.1. Lipoma. Ultrasound image shows oval hypoechoic subcutaneous lipoma (arrows) with internal linear hyperechoic fibrous tissue. |
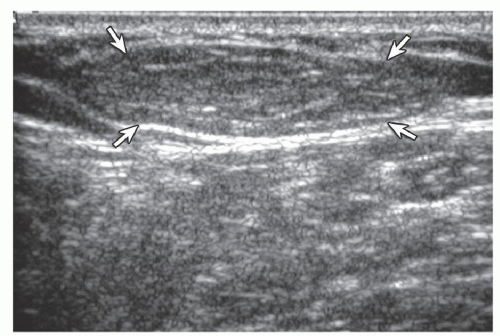 Figure 9.2. Lipoma. Ultrasound image shows oval hyperechoic subcutaneous lipoma (arrows) with internal linear hyperechoic fibrous tissue. |
Tip:
Superficial lipomas are typically elliptical, well defined, pliable, and avascular.
Lipoma echotexture varies from hypoechoic to hyperechoic relative to subcutaneous fat, but is homogeneous.
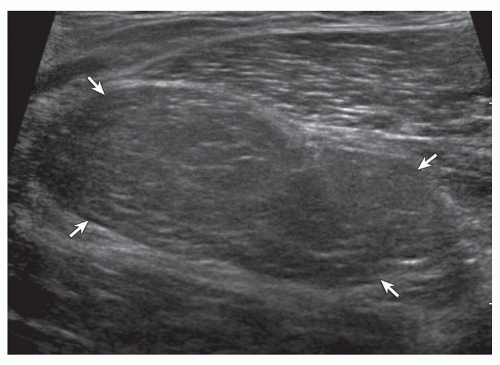
The ultrasound features of deeper lipomas are more variable and diagnosis less accurate.23 This is related to lower resolution of deeper structures, the inability of ultrasound to identify internal septations in well-differentiated liposarcomas, and the higher prevalence of liposarcomas in deeper soft tissues.24 Intramuscular lipomas are often ill-defined and insinuate into the adjacent muscle fibers. Echogenicity is variable, often isoechoic to hyperechoic, relative to the surrounding muscle (Fig. 9.5). When a deep lipoma is identified on ultrasound, MRI should be recommended to confirm that there are no suspicious features.
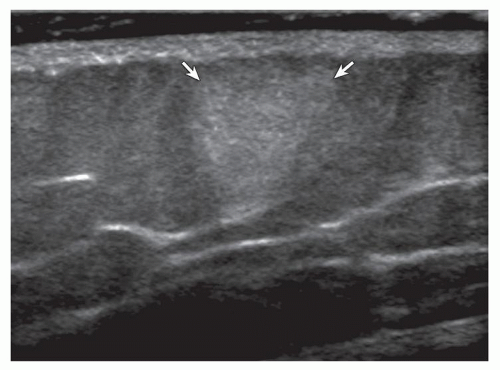 Figure 9.3. Lipoma. Ultrasound image shows round hyperechoic subcutaneous lipoma (arrows) (pathologically proven). |
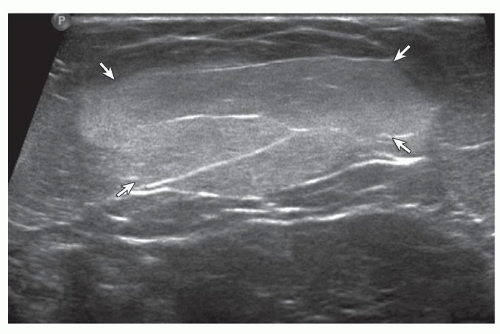 Figure 9.4. Lipoma. Ultrasound image shows oval hyperechoic subcutaneous lipoma (arrows) with internal linear hyperechoic fibrous tissue (pathologically proven). |
Other benign lesions can be considered in the differential diagnosis of superficial lipomas. If a presumed subcutaneous lipoma is hyperechoic and tender, angiolipoma and fat necrosis should be considered (see later discussion).25,26 Most malignant processes tend to be hypoechoic. Dermatofibrosarcoma protuberans may be hyperechoic,27 but does not have the other ultrasound features of a superficial lipoma.
Other Benign Lipomatous Masses
Several less common benign lipomatous masses deserve brief comment.20 Diffuse lipomatosis is diffuse infiltration of an anatomic region with mature fat, usually presenting by the age of 2 years when involving the extremity. Lipomatosis of nerve (also termed fibrolipomatous hamartoma) is fibrofatty infiltration of a peripheral nerve, typically the median nerve at the wrist and associated with
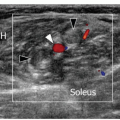
macrodystrophia in 67% of cases.20 Ultrasound shows hyperechoic fibrofatty tissue separating the individual hypoechoic nerve fascicles in the enlarged nerve (Fig. 9.6). Angiolipoma presents as a small (<2 cm), possibly painful circumscribed mass in the subcutaneous tissues. It is typically hyperechoic, and there may be increased vascularity (Fig. 9.7).25 Hibernoma is a benign tumor composed of brown fat (Fig. 9.8). Although somewhat similar in appearance to a lipoma, the increased echogenicity and possible internal vascularity typically raise concern for other pathologies such as well-differentiated liposarcoma.28
macrodystrophia in 67% of cases.20 Ultrasound shows hyperechoic fibrofatty tissue separating the individual hypoechoic nerve fascicles in the enlarged nerve (Fig. 9.6). Angiolipoma presents as a small (<2 cm), possibly painful circumscribed mass in the subcutaneous tissues. It is typically hyperechoic, and there may be increased vascularity (Fig. 9.7).25 Hibernoma is a benign tumor composed of brown fat (Fig. 9.8). Although somewhat similar in appearance to a lipoma, the increased echogenicity and possible internal vascularity typically raise concern for other pathologies such as well-differentiated liposarcoma.28
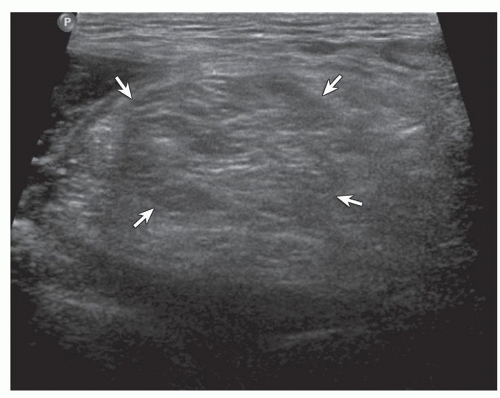 Figure 9.5. Lipoma: intramuscular. Ultrasound image shows isoechoic intramuscular lipoma (arrows) with internal linear hyperechoic fibrous tissue (pathologically proven). |
Liposarcoma
Liposarcoma is a malignant fat-containing tumor, which has several subtypes and can vary in tumor grade. Liposarcoma is the second most common soft tissue sarcoma, accounting for up to 35% of soft tissue sarcomas.24 The subtypes of liposarcoma include well-differentiated, dedifferentiated, myxoid, pleomorphic, and mixed liposarcomas.24 At one end of the spectrum is a well-differentiated, low-grade liposarcoma (previously termed atypical lipoma), while at the other end is a poorly differentiated, high-grade pleomorphic liposarcoma. The imaging appearances of liposarcomas relate to their subtypes and grades of malignancy.
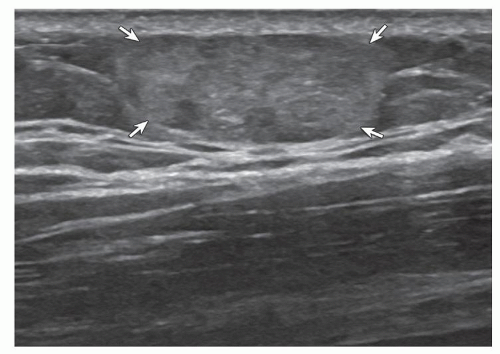 Figure 9.7. Angiolipoma. Ultrasound image shows well-defined hyperechoic angiolipoma (arrows) within the subcutaneous tissues (pathologically proven). |
The ultrasound appearances of liposarcomas tend to fall into three categories. The first is the well-differentiated liposarcoma, the most common type of liposarcoma, most frequently located in the deep tissues when involving an extremity.24 A well-differentiated liposarcoma is predominantly composed of fat (>75%), but may also be characterized by thick septations and/or nodules. At CT or MR imaging, thick septations (>2 mm) or nodules in a fatty tumor, especially if enhancing, indicate well-differentiated low-grade liposarcoma until proven otherwise.24,29 Although such features may be identified, the septations or nodules are often not well seen at ultrasound, and therefore a well-differentiated liposarcoma may be misdiag-nosed as a lipoma (Fig. 9.9). Given the higher prevalence of liposarcomas in deeper soft tissues and the difficulty in providing an accurate diagnosis with ultrasound, any fatty tumor deeper than the subcutaneous tissues warrants MR. Well-differentiated liposarcomas calcify or ossify in 10% to 32% of cases.24
Tip:
Any fatty tumor deeper than the subcutaneous tissues may be a liposarcoma and warrants MRI evaluation.
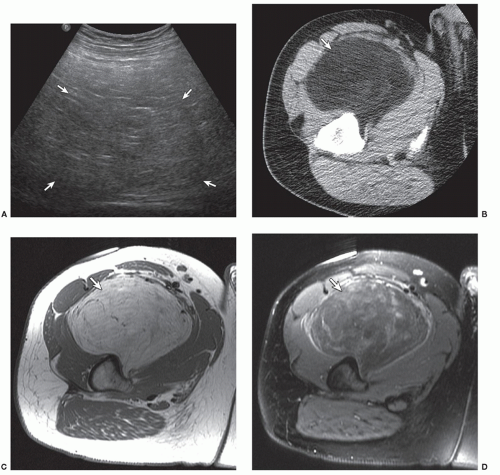
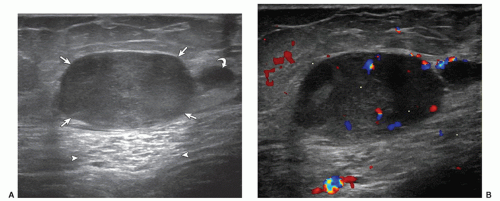
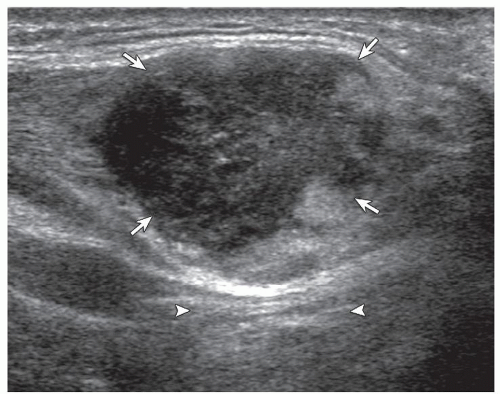
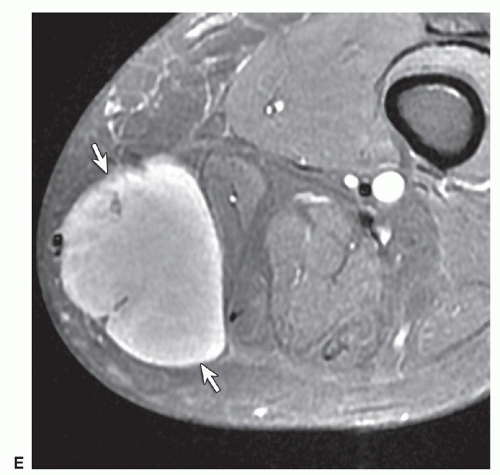
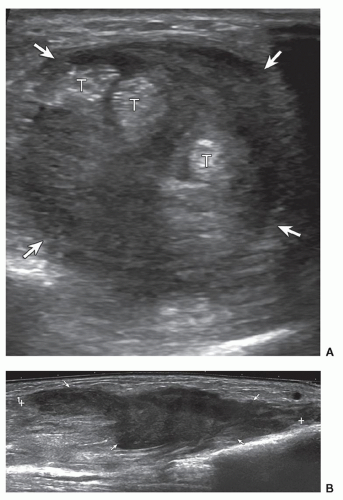
The second ultrasound appearance relates to the myxoid subtype, which is the second most common type of liposarcoma.24 Myxoid liposarcomas are heterogeneous and contain myxoid, round cell, and fat components,
although fat may comprise <10% of the tumor volume.24 The ultrasound appearances depend on the amount of each component. If a myxoid component is predominant, the mass may appear hypoechoic and potentially simulate a complex cyst (Fig. 9.10). To avoid misdiagnosis of a myxoid liposarcoma as a complex cyst, any “cyst-appearing” mass, which does not correspond to a bursa, especially when large, can be biopsied for confirmation.
although fat may comprise <10% of the tumor volume.24 The ultrasound appearances depend on the amount of each component. If a myxoid component is predominant, the mass may appear hypoechoic and potentially simulate a complex cyst (Fig. 9.10). To avoid misdiagnosis of a myxoid liposarcoma as a complex cyst, any “cyst-appearing” mass, which does not correspond to a bursa, especially when large, can be biopsied for confirmation.
Tip:
Consider biopsy of any round “cyst-appearing” mass that does not correspond to a bursa, especially if large, for confirmation of the diagnosis.
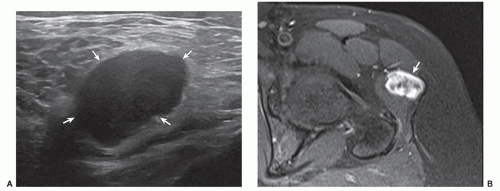
A myxoid liposarcoma (Fig. 9.11) should not be mistaken for a ganglion cyst, which is usually multilocular
and not typically large, or a Baker’s cyst, which has a neck between the medial head of the gastrocnemius muscle and the semimembranosus tendon. Myxoid liposarcoma may appear more heterogeneous if increased round cell components are present and therefore appear more nonspecific at ultrasound.
and not typically large, or a Baker’s cyst, which has a neck between the medial head of the gastrocnemius muscle and the semimembranosus tendon. Myxoid liposarcoma may appear more heterogeneous if increased round cell components are present and therefore appear more nonspecific at ultrasound.
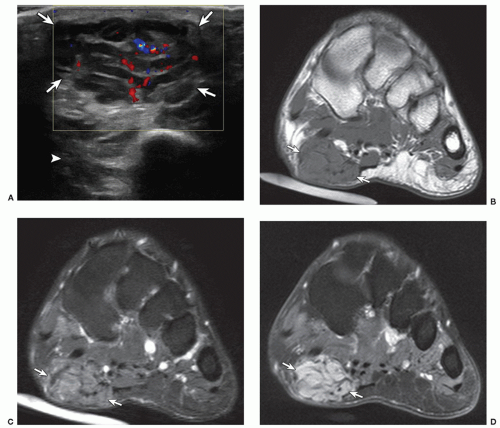
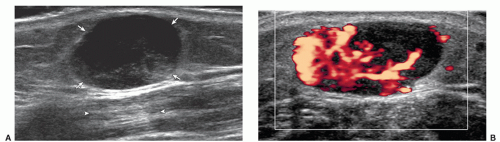
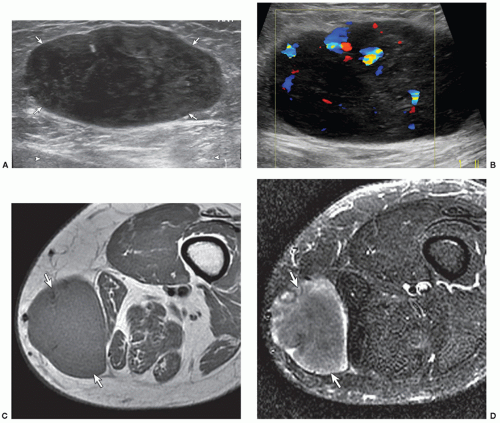
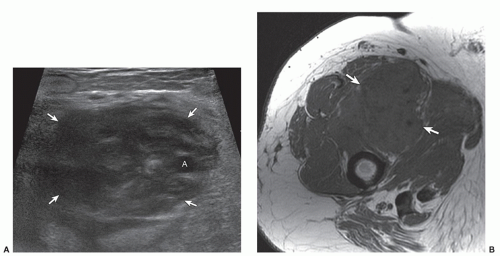
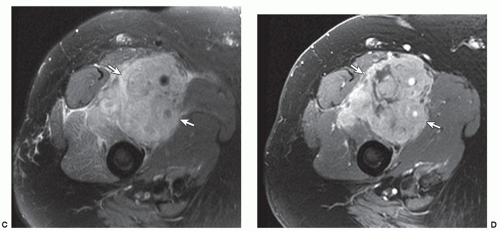
The third ultrasound appearance of liposarcoma occurs with high-grade or poorly differentiated tumors, and includes dedifferentiated, myxoid (if containing a round cell component), pleomorphic, and mixed subtypes. In this situation, the appearance is nonspecific and similar to any high-grade sarcoma. Although predominantly hypoechoic, there are often heterogeneous anechoic areas due to necrosis, heterogeneity, and increased flow on color and power Doppler imaging (Fig. 9.12).
Fibrous Tumors
Soft tissue fibrous proliferation may be categorized as fibromatoses (which includes superficial and deep fibromatoses), benign fibrous proliferations (which includes nodular fasciitis and elastofibroma), fibrosarcomas, and fibrous proliferations of infancy and childhood.30
Superficial Fibromatosis
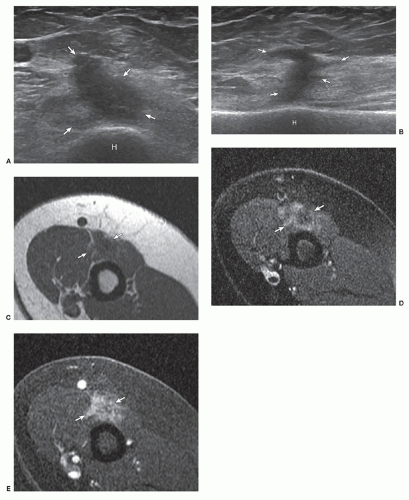
Superficial fibromatosis includes plantar and palmar fibromas.30 They are benign but, although having no malignant potential, may behave aggressively. Palmar fibromatosis (or Dupuytren disease) is the most common superficial fibromatosis. It occurs typically in men over the age of 30 and is bilateral in approximately 50% of cases.30 Palmar fibromatosis involves the volar hand and appears as hypoechoic fusiform masses or nodules along the palmar fascia, often associated with flexion deformity of the digits (Fig. 9.13).31 Plantar fibromatosis (Ledderhose disease) appears as single or multiple discrete fusiform hypoechoic nodules or thickenings along the plantar fascia of the foot (Fig. 9.14). Increased flow on color and power Doppler imaging may be present (Fig. 9.15).32 Plantar fibromatosis more commonly involves men, is associated with palmar fibromatosis in up to 65% of cases,
and is bilateral in 20% to 50% of cases.30 The presence of multiple plantar aponeurosis nodules, unilateral or bilateral, is diagnostic of plantar fibromatosis.
and is bilateral in 20% to 50% of cases.30 The presence of multiple plantar aponeurosis nodules, unilateral or bilateral, is diagnostic of plantar fibromatosis.
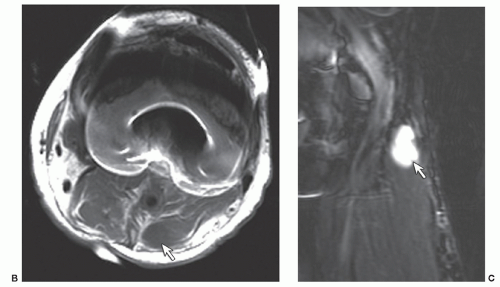 Figure 9.11. (continued) Axial T1-weighted (B) and sagittal fluid-sensitive (C) MR images show a fluid signal lobular mass (arrow). Note artifact related to total knee arthroplasty. |
Tip:
Multiple nodules on the plantar fascia are diagnostic of plantar fibromatosis.
Deep Fibromatoses
Deep fibromatoses or desmoid tumors (also termed aggressive fibromatosis) are benign fibrous proliferations at musculoaponeurotic sites, most common in adults between the ages of 25 and 35,33 and multiple in 15% of cases.30 Common locations include the shoulder, chest wall, back, thigh, and knee.30 Similar to superficial fibromatoses, desmoid tumors do not metastasize but may be locally aggressive. Desmoid tumors can be intra-abdominal, within the abdominal wall, or extra-abdominal.34 They are typically hypoechoic with possible acoustic shadowing, and flow on color and power Doppler imaging (Fig. 9.16).31 Extra-abdominal desmoids are characterized by an aggressive and infiltrative pattern. A characteristic ultrasound feature is an ill-defined border where it extends through fascial planes, creating a “fascial tail.”33 Patients who have desmoids are at risk of having familial adenomatous polyposis (FAP) and should be screened for FAP.
Nodular Fasciitis
Nodular fasciitis is a benign proliferation of fibroblasts and myofibroblasts, most common between the ages of 20 and 40 years.30 Two notable features include its propensity to involve the volar aspect of the forearm, and its rapid growth,30 which often leads to a mistaken diagnosis of soft tissue sarcoma. Ultrasound shows a well-defined soft tissue mass that may be isoechoic to the surrounding tissues or heterogeneous with mixed hypoechoic and isoechoic areas (Fig. 9.17).35 Increased through-transmission has also been described, similar to other soft tissue masses.35
Tip:
A rapidly growing mass in the volar forearm suggests nodular fasciitis.
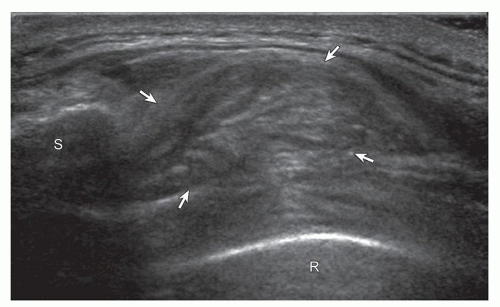
Elastofibroma Dorsi
Elastofibroma dorsi is a benign fibroelastic pseudotumor, believed to result from friction between the scapula and chest wall,36 that almost exclusively occurs at the inferior margin of the scapula, deep to the serratus anterior, rhomboid major and latissimus dorsi muscles. It is usually seen in elderly women, often asymptomatic and bilateral in up to 66% of patients.36 Elastofibroma contains alternating fatty and fibrous tissue layers, which produce a characteristic heterogeneous and striated appearance with numerous linear and curvilinear hypoechoic fat and hyperechoic fibrous tissue interfaces (Fig. 9.18).36 Dynamic imaging is helpful as the mass may be obscured by the scapula in neutral position.37 Placing the ipsilateral hand on the opposite shoulder may throw the scapula off the mass.
Tip:
A soft tissue mass at the lower pole of the scapula suggests an elastofibroma, and demonstration of a striated appearance confirms the diagnosis and avoids biopsy.
Fibrosarcoma
Fibrosarcoma is a malignant tumor of low-to-intermediate grade that is most common in the adult population aged 40 to 70 years.38 Ultrasound shows a nonspecific mass, possibly heterogeneous with calcifications.1 Myxofibrosarcoma most commonly involves the subcutaneous tissues of the extremities and has a propensity to spread along fascial and vascular planes; recurrent tumor is associated with higher grade and distant metastases (Fig. 9.19).39
Malignant fibrous histiocytoma or undifferentiated pleomorphic sarcoma is the most common soft tissue sarcoma. It has a peak incidence in the fifth decade of life, is more common in men, and is the most common radiation-induced soft tissue sarcoma.38 Most (70%) are intramuscular, usually in the extremities, but 5% to 10% are subcutaneous.38 Ultrasound demonstrates a nonspecific heterogeneous soft tissue mass with mixed hypoechoic and echogenic regions and increased vascularity (Fig. 9.20).1 Anechoic regions are due to tumor necrosis. In 2002, the WHO reorganized the classification of soft tissue sarcomas, and the term malignant fibrous histiocytoma has been replaced by undifferentiated pleomorphic sarcoma.38
Dermatofibrosarcoma Protuberans
Dermatofibrosarcoma protuberans (DFSP) is one of the more common malignant soft tissue tumors and accounts for 6% of soft tissue sarcomas.38 It frequently involves males in the third to fifth decades of life and presents as a growing palpable soft tissue nodule.38 A phase of rapid tumor growth has been described after a quiescent phase of months to years.40 Because DFSP is dermal and clinically apparent, it is frequently not imaged prior to biopsy or attempted removal. Ultrasound shows a superficial hypoechoic or mixed echogenicity dermal mass with variable flow on color and power Doppler imaging (Fig. 9.21).27,40 A hyperechoic appearance may be seen due to interfaces between fibrous tissue and tumor cells (Fig. 9.22),27 and this appearance is associated with irregular margins due to tumor infiltration, unlike other superficial hyperechoic masses such as lipoma, which are well defined.
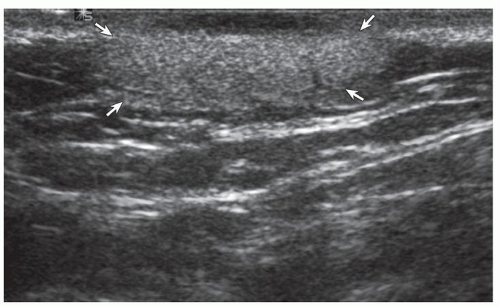 Figure 9.22. Dermatofibrosarcoma protuberans. Ultrasound image shows a hyperechoic mass (arrows) (pathologically proven). |
Smooth Muscle Tumors
Tumors that have a predominant smooth muscle differentiation include benign leiomyomas and malignant leiomyosarcomas. Although leiomyomas are uncommon outside the uterus and gastrointestinal tract, they may be found in the extremities and take one of three forms: cutaneous leiomyoma (most common, located in the dermis), angioleiomyoma (located in the subcutaneous tissues), and leiomyoma of deep tissues.41 Extra-uterine leiomyosarcoma represents the malignant form, and can be divided into four subtypes: cutaneous, subcutaneous, deep soft tissue, and vascular.42 At ultrasound, a leiomyoma appears as a nonspecific hypoechoic or slightly heterogeneous mass (Fig. 9.23), whereas a leiomyosarcoma
will more likely show heterogeneity (Fig. 9.24), increased vascularity, and possible necrosis.
will more likely show heterogeneity (Fig. 9.24), increased vascularity, and possible necrosis.
Lymphoid Tumors
Lymphoma
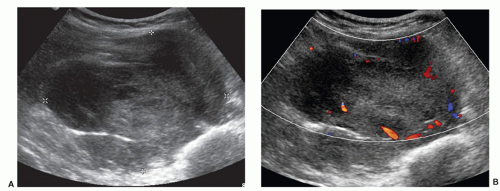
Lymphoid neoplasms may be categorized as Hodgkin, non-Hodgkin, and plasma cell neoplasms, of which 80% to 85% originate from B cells.43 The typical presentation is of localized or generalized lymph node enlargement.44 Extra-nodal involvement, especially involving the soft tissues of the extremities, is rare.44
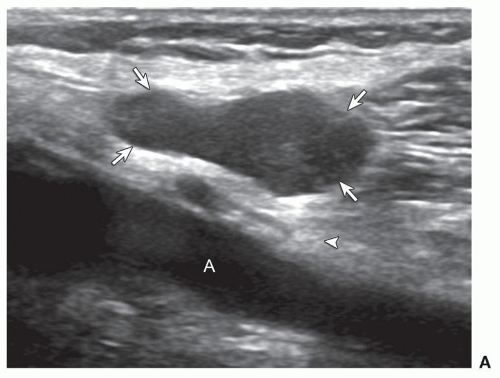
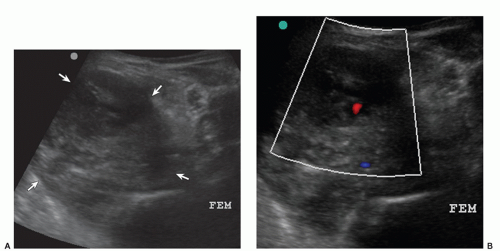
Lymph node involvement in lymphoma has an appearance that it is consistent with malignant infiltration but is otherwise nonspecific, including enlargement, a round rather than oval shape, thickening of the node cortex, and narrowing or obliteration of the echogenic hilum. Malignant nodes often have a peripheral or mixed rather than hilar vascular pattern on color and power Doppler imaging (Fig. 9.25)45 but a hilar pattern is commonly seen in lymphoma and may also be seen with reactive lymph nodes.46 Although lymph node measurements may be used as guidelines for tumor involvement, it is more critical to assess the morphology of a lymph node than rely on measurements.47
Extra-nodal lymphoma of soft tissues most commonly appears as a hypoechoic mass with infiltrative margins and significantly increased vascularity on color and power Doppler imaging.44 In spite of often large size, necrosis is typically absent.44 Another characteristic feature is its ability to extend through the soft tissues while preserving the surrounding soft tissues.43 The characteristic sonographic features of extreme hypervascularity, lack of necrosis, and infiltrative pattern may suggest the diagnosis. Another presentation is of heterogeneous muscle infiltration with preservation of the muscle architecture and plump muscle bundles (Fig. 9.26).44 Osseous invasion produces discontinuity or destruction of the normally smooth and echogenic bone cortex. Peripheral nerve involvement has also been described.48 Lymphoma rarely appears as an ill-defined hyperechoic subcutaneous soft tissue mass as seen with subcutaneous T-cell lymphoma.49
Tip:
A hypervascular soft tissue mass with preserved architecture suggests lymphoma.
Neural Tumors
Peripheral Nerve Sheath Tumors
Schwannoma (or neurilemmoma) and neurofibroma represent two forms of benign peripheral nerve sheath
tumors, and commonly present between the ages of 20 and 30 years.50 Schwannoma tends to be solitary, but can be multiple (termed schwannomatosis) and can be associated with neurofibromatosis type I.50 The characteristic histologic features of a schwannoma are the presence of Antoni A and B regions.50 Neurofibromas have three different forms: localized, plexiform, and diffuse.50 Localized neurofibromas are usually <5 cm in size and painless. Plexiform neurofibromas appear as multiple swellings diffusely involving a nerve trunk or as diffuse enlargement of a nerve. Diffuse neurofibromas cause thickening of the subcutaneous and dermal tissues and envelop tendons, nerves, and vessels. Although all forms of neurofibromas can be associated with neurofibromatosis I, plexiform neurofibromas are considered pathognomonic.50 Other hallmarks of neurofibromatosis I include cutaneous neurofibromas (frequently multiple), skin lesions (café au lait spots), skeletal deformities, and mental deficiency.50 Histologically, in contrast to schwannoma, Antoni A and B regions are not identified. Neurofibromatosis II primarily affects the central nervous system.
tumors, and commonly present between the ages of 20 and 30 years.50 Schwannoma tends to be solitary, but can be multiple (termed schwannomatosis) and can be associated with neurofibromatosis type I.50 The characteristic histologic features of a schwannoma are the presence of Antoni A and B regions.50 Neurofibromas have three different forms: localized, plexiform, and diffuse.50 Localized neurofibromas are usually <5 cm in size and painless. Plexiform neurofibromas appear as multiple swellings diffusely involving a nerve trunk or as diffuse enlargement of a nerve. Diffuse neurofibromas cause thickening of the subcutaneous and dermal tissues and envelop tendons, nerves, and vessels. Although all forms of neurofibromas can be associated with neurofibromatosis I, plexiform neurofibromas are considered pathognomonic.50 Other hallmarks of neurofibromatosis I include cutaneous neurofibromas (frequently multiple), skin lesions (café au lait spots), skeletal deformities, and mental deficiency.50 Histologically, in contrast to schwannoma, Antoni A and B regions are not identified. Neurofibromatosis II primarily affects the central nervous system.
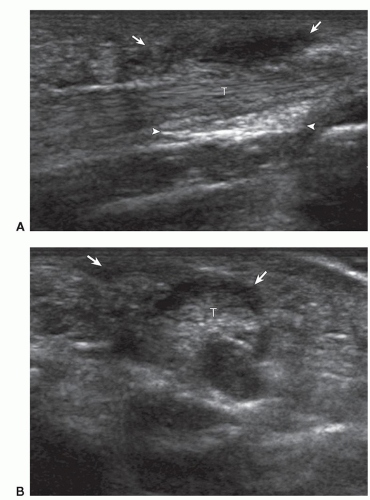
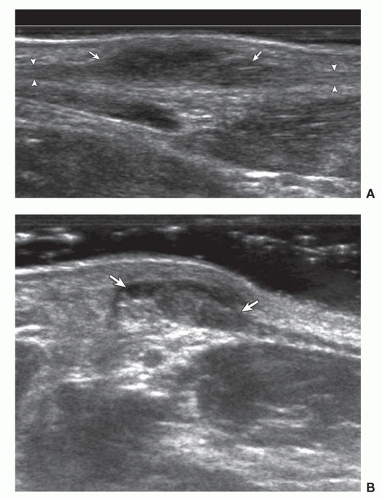
At ultrasound, solitary schwannoma (Fig. 9.27) and neurofibroma (Fig. 9.28) look similar, appearing as well-defined hypoechoic fusiform masses with internal low-level and homogeneous echoes.51,52 The finding of a peripheral nerve entering and exiting the mass is key to the diagnosis. Often hyperechoic fat is identified around the entering/exiting nerve producing an echogenic, triangular “cap” at the edge of the mass, termed the “split-fat sign.”
Tip:
The split-fat sign and a nerve entering/exiting a soft tissue mass are characteristic of a nerve tumor.
If the entering or exiting nerve is eccentric to the mass, schwannoma may be suggested, whereas in neurofibroma the nerve tends to be central,52 but these findings are not invariable.
Tip:
Ultrasound cannot reliably distinguish between schwannoma and neurofibroma.
Increased through-transmission deep to a nerve sheath tumor is common51 and should not lead to a mistaken diagnosis of a complex cyst. Blood flow within neural tumors is typical and is absent in complex cysts. Schwannomas may be heterogeneous due to cyst formation (Fig. 9.29),52 the so-called “ancient schwannomas.” A target appearance has been described due to an echogenic
fibrocollagenous center and surrounding hypoechoic myxoid area, most notably with benign neurofibromas.53 Plexiform neurofibromas appear as multiple lobular, predominantly hypoechoic masses with possible target appearances involving a large nerve trunk.53 Diffuse neurofibroma appears as hyperechoic dermal and subcutaneous tissue thickening with intervening hypoechoic tubular or nodular areas.54 As they are frequently extensive, plexiform and diffuse neurofibromas are best imaged by MRI.
fibrocollagenous center and surrounding hypoechoic myxoid area, most notably with benign neurofibromas.53 Plexiform neurofibromas appear as multiple lobular, predominantly hypoechoic masses with possible target appearances involving a large nerve trunk.53 Diffuse neurofibroma appears as hyperechoic dermal and subcutaneous tissue thickening with intervening hypoechoic tubular or nodular areas.54 As they are frequently extensive, plexiform and diffuse neurofibromas are best imaged by MRI.
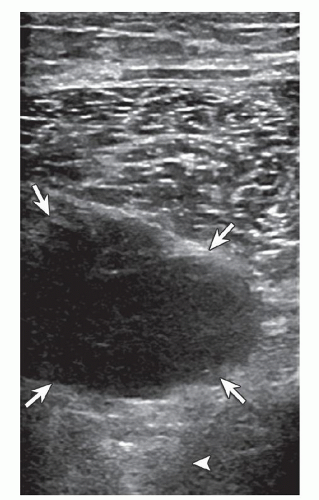
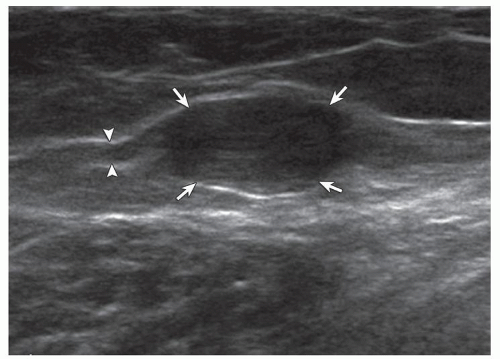 Figure 9.28. Neurofibroma. Ultrasound image shows a well-defined hypoechoic mass (arrows) that is in continuity with a peripheral nerve (arrowheads) (pathologically proven).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|