Foot and Ankle
Ryan Lee
James Griffith
INTRODUCTION
The superficial location of most soft tissue and surface bone lesions of the ankle and foot makes this area readily accessible to high frequency (>10 MHz) ultrasound. The high resolution and clinical efficacy of ultrasound ensure that it is a comparable, and in many respects better, imaging modality than magnetic resonance imaging (MRI) when assessing most soft tissues of the foot and ankle. Imaging anatomy and pathology are best approached by arbitrarily dividing the ankle into anterior, posterior, medial, and lateral regions, whereas the foot is best approached by separately considering the hindfoot, midfoot, and forefoot.
PATIENT POSITION
For the anterior, medial, and lateral ankle and dorsal foot, the patient should be supine with the knee semiflexed. The knee is rotated medially and the ankle slightly inverted for the lateral ankle, and the knee rotated laterally with the ankle slightly everted for the medial ankle. For the posterior ankle and sole of the foot, the patient is best examined prone with the foot hanging freely or in a dorsiflexed position over the edge of the examination couch.
ULTRASOUND APPEARANCES OF LIGAMENTS, TENDONS, AND NERVES
The ultrasound appearances of ankle and foot ligaments, tendons, and nerves are similar to those in other parts of the body. In general, ligaments are seen as thin, regular, hyperechoic fibers aligned in parallel with a well-defined border and attached to bone at both ends. Ankle ligaments are best examined with the transducer aligned with the long axis of the ligament and the ligament stretched. Tendons have a thicker, tightly packed linear fibrillar echotexture when scanned longitudinally and have a speckled echogenic dot appearance on transverse scanning. Most tendons and nerves around the ankle joint are best examined in a transverse plane. Extended longitudinal views of the curved ankle tendons are difficult to obtain. Ankle tendons are prevented from “bowstringing” by overlying thin fibrous retinacula, which also serve as fulcra for the pulley action of the tendons. All ankle and foot ligaments and tendons are anisotropic and appear hypoechoic if the transducer is not perpendicular to their fibers. Anisotropy can be used to identify a tendon or ligament by distinguishing it from adjacent tissues. For example, tilting the transducer to make the anterior talofibular ligament (ATFL) appear hypoechoic accentuates the conspicuity of the ligament against the adjacent echogenic fat. Conversely, tendon or ligament echogenicity should always be interpreted in the light of anisotropy. Nerves are also tubular echogenic fascicular structures. They have a slightly coarser fibrillar echotexture than tendons and are found in predictable locations, typically in neurovascular bundles. If doubt exists, nerves can be differentiated from tendons by tracing their course proximally or distally, while scanning in short axis.
Tip:
In general, most ankle and foot tendons or ligaments are best assessed with ultrasound except for those on the plantar aspect of the foot, which are best assessed with MR imaging
RELEVANT ULTRASOUND ANATOMY
Anterior Ankle
Anterior Ligaments
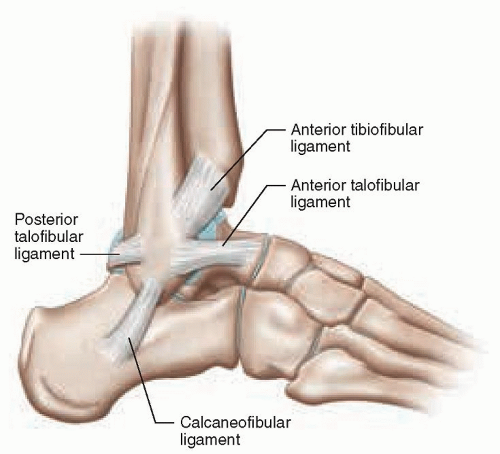
The anterior inferior tibiofibular ligament is a strong multifascicular fan-shaped ligament that lies between the anterior aspect of the distal tibia (Tillaux-Chaput tubercle) and the adjacent fibula (Fig. 8.1). It runs slightly obliquely upward and medially from the anteromedial aspect of the distal fibula at the upper margin of the ankle joint and is widest at the tibial insertion (Fig. 8.1). Moving the transducer proximally in a transverse plane from the ankle joint shows the anterior tibiofibular ligament (Fig. 8.2). Ligament conspicuity can be improved by slight angulation of the transducer or by rotating the tibial end of the transducer slightly more cranially.
The ligament is <2-mm wide at its mid-portion and provides major support to the distal tibiofibular syndesmosis.1 The distal interosseous membrane is seen as a thin, hyperechoic (almost isoechoic to bone) line between the tibia and the fibula2 proximal to the anterior tibiofibular ligament.
The ligament is <2-mm wide at its mid-portion and provides major support to the distal tibiofibular syndesmosis.1 The distal interosseous membrane is seen as a thin, hyperechoic (almost isoechoic to bone) line between the tibia and the fibula2 proximal to the anterior tibiofibular ligament.
Tip:
The anterior inferior tibiofibular ligament is best seen by scanning transversely between the tibia and the fibula just proximal to the ankle joint.
Anterior Tendons
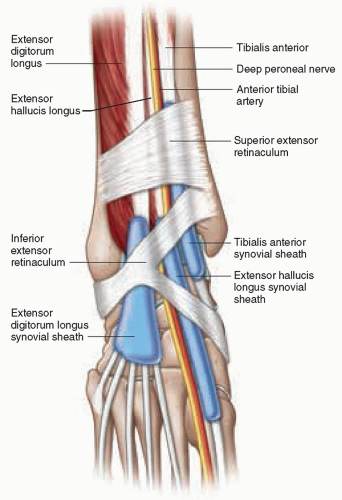
The anterior ankle tendons comprise the tibialis anterior, extensor hallucis longus (EHL), and extensor digitorum longus (EDL) from medial to lateral (Fig. 8.3). They can be memorized by “Tom Has a Date Perhaps” from medial to lateral (Tom = Tibialis anterior, Has = extensor Hallucis longus, A = Anterior tibial artery/vein and deep peroneal nerve, Date = extensor Digitorum longus, and Perhaps = Peroneus tertius). They are covered by retinaculum. The superior extensor retinaculum extends from the lateral malleolus to the medial malleolus and is continuous with the flexor retinaculum medially and superior peroneal retinaculum laterally. The inferior extensor retinaculum is Y-shaped. The stem of the Y lies on the lateral aspect of the retinaculum and divides into superomedial and inferomedial limbs, which attach to the medial malleolus and navicular-cuneiform area, respectively.
 Figure 8.2. Transverse ultrasound showing normal anterior inferior tibiofibular ligament (arrows) with a wider attachment to the tibia than the fibula. |
The tibialis anterior tendon is the strongest, largest, and most superficial of the anterior tendons. It begins at the junction of the lower and middle-thirds of the tibia. At the level of the ankle joint, it lies medial to the midline
and then runs toward the medial border of the foot, where it attaches to the superomedial aspect of the medial cuneiform and the first metatarsal3,4 (Fig. 8.3). The tendon is ovoid proximally and becomes flatter distally, measuring <5 mm in width at 3 cm from its insertion.5
and then runs toward the medial border of the foot, where it attaches to the superomedial aspect of the medial cuneiform and the first metatarsal3,4 (Fig. 8.3). The tendon is ovoid proximally and becomes flatter distally, measuring <5 mm in width at 3 cm from its insertion.5
The EHL tendon lies just lateral to the tibialis anterior tendon and inserts dorsally on the base of the distal phalanx of the hallux. The anterior tibial artery, anterior tibial vein, and deep peroneal nerve lie just lateral to EHL. In the distal leg, the deep peroneal nerve lies on the medial side of the anterior tibial artery. At the ankle, the nerve crosses over the artery to lie on its lateral side (Fig. 8.3). This arrangement is important to note during aspiration of an ankle joint effusion using an anterior approach.
The EDL tendon is the most lateral of the anterior tendons, and branches at the anterior ankle joint line into separate tendons to the second to fifth toes (Fig. 8.3). The peroneus tertius tendon crosses the ankle joint lateral to the EDL tendon to insert into the dorsal surface of the fifth metatarsal base. It is absent in about 10% of individuals.
Tip:
All extensor tendons of the ankle have their own individual tendon sheath at the level of the inferior retinaculum.
The deep and superficial peroneal nerves arise from the common peroneal nerve at the level of the fibular neck and run distally deep to the peroneus longus muscle. At the ankle, the deep peroneal nerve runs deep to the extensor retinaculum initially medial to and then lateral to the anterior tibial artery. Just distal to the retinaculum it divides into a medial sensory branch, which supplies the first digital interspace, and a lateral motor branch, which supplies the extensor digitorum brevis muscle. It can become trapped between the extensor digitorum brevis muscle and the head of the talus.6 The superficial peroneal nerve separates from the deep peroneal nerve 10 to 15 cm above the ankle. It pierces the investing fascia about 9 cm proximal to the lateral malleolus, where it is prone to injury,7 then runs anterolateral to the lateral malleolus, superficial to the superior and inferior extensor retinacula, before dividing into medial and intermediate dorsal cutaneous nerves. It provides sensory innervation to the skin on the dorsum of the foot and most of the toes.
Tip:
The deep peroneal nerve lies initially medial to and then lateral to the anterior tibial artery at the ankle joint.
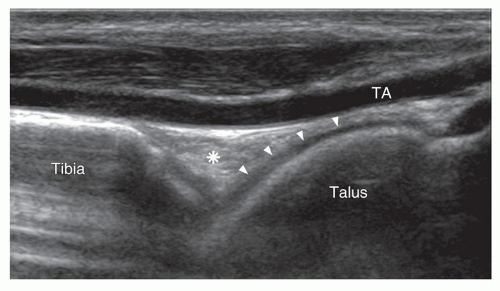
Anterior Ankle Joint
The anterior ankle joint is best assessed in the longitudinal plane with the ankle in slight plantar flexion. The anterior joint capsule is attached along the distal margin of the tibia and fibula approximately 10 mm from the ankle joint and extends to the neck of the talus.8 High-resolution imaging is needed to distinguish the capsule from the triangular-shaped fat pad that lies slightly deeper and divides the anterior recess of the ankle into smaller superior and larger inferior recesses (Fig. 8.4). A small amount of joint fluid is normal and best appreciated in the medial and lateral recesses. Larger quantities of fluid distend the anterior and posterior recesses. Increased fluid in the anterior recess displaces the fat pad anteriorly. A thin (approximately 2 mm), hypoechoic layer of articular cartilage covers the anterior aspect of the talar dome when the ankle is plantar flexed and should not be confused with joint fluid. Articular cartilage in the central and posterior ankle joint cannot be seen with ultrasound.
The anterolateral recess or gutter is bounded laterally by the fibula, medially by the talus and tibia, anteriorly by the tibiotalar joint capsule, the anterior talofibular and tibiofibular ligaments, anteroinferiorly by the calcaneofibular (CFL) ligament, and superiorly by the tibial plafond and distal tibiofibular syndesmosis.9 The anterolateral and anteromedial recesses should be routinely assessed on ultrasound of the ankle joint as fluid, crystal aggregates, synovial proliferation, and other pathologies may be visible, although not apparent in the anterior recess.
Lateral Ankle
Lateral Ligaments
The lateral ankle ligaments, or lateral collateral ligaments, comprise the anterior talofibular, CFL, and posterior talofibular ligaments (Fig. 8.1).
Anterior Talofibular Ligament (ATFL)
The ATFL is a condensation of the ankle capsule similar to the glenohumeral ligaments in the shoulder.10 It extends
from the anterosuperior aspect of the distal fibula at the level of the malleolar fossa to the lateral aspect of the neck of talus. It is best visualized with the ankle in a relaxed position (about 20 degrees plantar flexed, i.e., with the sole of the foot flat on the examination couch) and the ligament almost parallel to the ankle joint. The transducer is placed just anterior to the lateral malleolus and oriented horizontally. The distal end of the transducer is then turned slightly caudally.11 The normal thickness of the ATFL is 2 mm, and it is about 20 mm in length.12 The ligament is best seen when straight and taut (Fig. 8.5) by plantar flexing the ankle joint.
from the anterosuperior aspect of the distal fibula at the level of the malleolar fossa to the lateral aspect of the neck of talus. It is best visualized with the ankle in a relaxed position (about 20 degrees plantar flexed, i.e., with the sole of the foot flat on the examination couch) and the ligament almost parallel to the ankle joint. The transducer is placed just anterior to the lateral malleolus and oriented horizontally. The distal end of the transducer is then turned slightly caudally.11 The normal thickness of the ATFL is 2 mm, and it is about 20 mm in length.12 The ligament is best seen when straight and taut (Fig. 8.5) by plantar flexing the ankle joint.
Tip:
The ATFL is best seen by scanning almost transversely when the foot is slightly plantar flexed just distal to the ankle joint.
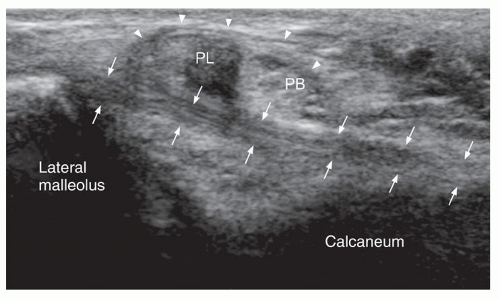
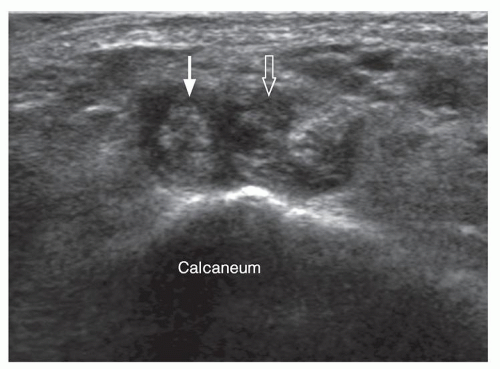
Calcaneofibular Ligament
The CFL ligament extends posteroinferiorly from the inferior tip of the fibula to insert on the lateral aspect of the calcaneal body. It lies deep, almost at right angles to the peroneal tendons (Fig. 8.1), and has a curved alignment akin to a hammock when relaxed. The normal ligament is about 2 mm wide and 2 mm thick and can be seen deep to the peroneal tendons when the tendons are scanned transversely12 (Fig. 8.6). The ligament is best seen with the ankle in dorsiflexion as this stretches the ligament and reduces its curvature. The transducer is positioned with its proximal end at the inferior tip of the lateral malleolus and its distal end aligned posteriorly and slightly toward the heel.12 The ligament is hyperechoic in the distal two-thirds only. The curved proximal portion of the ligament usually appears hypoechoic due to anisotropy.
Tip:
The CFL ligament is best seen deep to the inframalleolar peroneal tendons when these tendons are scanned in a transverse plane.
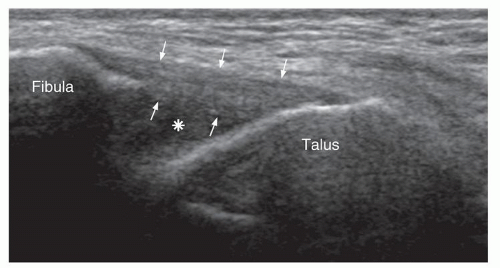 Figure 8.5. Transverse ultrasound showing normal ATFL (arrows). There is a small amount of fluid in the anterolateral ankle recess (asterisk). ATFL, anterior talofibular ligament. |
Posterior Talofibular Ligament
This ligament is partially obscured by the fibula and is difficult to see in its entirety on ultrasound. It is orientated in a similar plane to the ATFL and extends from the distal aspect of the malleolar fossa and to the lateral tubercle of the posterior process of the talus. It is best seen with the patient prone.
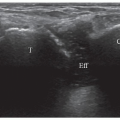
Lateral Tendons
The tendons posterior to the lateral malleolus are the peroneus brevis and peroneus longus tendons (Fig. 8.7). The peroneus longus tendon starts about 4 cm above the level of the ankle joint and peroneus brevis more distally. Both tendons run posterior and then inferior to the lateral malleolus where they share a common supramalleolar and retromalleolar synovial sheath. They lie within the fibro-osseous retromalleolar groove of the fibula covered by the superior peroneal retinaculum. The groove is lined by fibrocartilage and varies in width and depth. The superior peroneal retinaculum is about 1mm thick, 1- to 2 cm wide; extends from the posterolateral edge of the distal fibula to the lateral wall of the calcaneum, although variations of this insertion exist13; and is the primary restraint to peroneal tendon subluxation. The peroneus longus tendon lies posterolateral to the brevis tendon in the retromalleolar groove and takes the longer route around the inferior aspect of the malleolus (remembered by the peroneus longus takes the longer route round the malleolus or peroneus brevis lies closer to the bone). The peroneus longus is marginally (10% to 15%) larger in cross-sectional area than the peroneus brevis tendon.10
Tip:
The peroneus longus tendon is slightly larger than the peroneus brevis tendon in cross-sectional area.
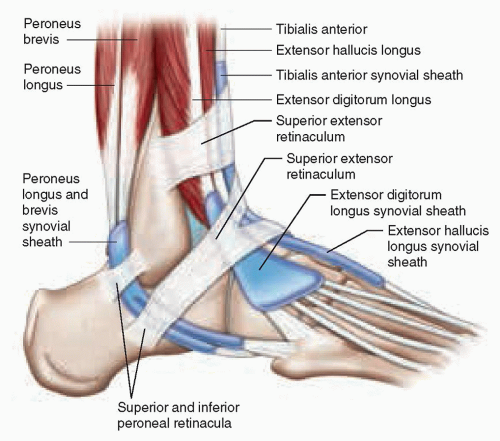 Figure 8.7. Schematic diagram of the tendons and retinacula on the anterior and lateral aspects of the ankle joint. |
The common peroneal tendon sheath divides just proximal to the peroneal tubercle of the calcaneus, and the tendons run anteriorly in their respective tendon sheaths. Peroneus brevis runs dorsal and peroneus longus plantar to the peroneal tubercle, deep to the inferior peroneal retinaculum. The tubercle varies in size from a clearly palpable and distinct tubercle to a barely discernible one. As peroneus longus moves around the peroneal tubercle, it may become irritated when the tubercle is hypertrophied. Small amounts of fluid in the peroneal tendon sheaths are normal, particularly in the dependent inframalleolar region. The peroneus brevis tendon extends horizontally from the peroneal tubercle to insert on the base of the fifth metatarsal.
Peroneus longus passes into the sole of the foot running in a groove on the cuboid (the cuboid tunnel) before turning sharply and running obliquely across the midfoot to insert onto the undersurface of the medial cuneiform and the base of the first metatarsal. The os peroneum is a sesamoid bone located in the peroneus longus tendon just proximal to the cuboid tunnel in up to 30% of adults, bilateral in 60% of cases, bipartite in about 10%,14 and seen as a small (5 to 15 mm) hyperechoic body with posterior acoustic shadowing. The primary function of the peroneus longus tendon is plantar flexion of the medial forefoot. Along with the peroneus brevis, it also everts and stabilizes the ankle joint.
Tip:
The os peroneum is located within the peroneus longus tendon and is sometimes associated with focal tendinosis of the peroneus longus and fracture.
An accessory peroneus quartus muscle, present in about 10% of subjects, lies medial and posterior to the peroneus brevis and longus. Its tendon runs in the common peroneal tendon sheath and usually inserts into the retrotrochlear eminence of the calcaneus, which is often hypertrophied, just posterior to the peroneal tubercle.15 Other insertions include the peroneus longus and brevis tendons, the base of the fifth metatarsal, and the cuboid.16 Occasionally, the muscle belly inserts directly into the retrotrochlear eminence.
The sural nerve runs initially between the Achilles tendon and the peroneal tendons accompanied by the small saphenous vein, then inferior to the peroneal tendons. It bifurcates into terminal lateral and medial branches at the base of the fifth metatarsal and provides sensory supply to the lateral ankle, foot, and the small toe. It anastomoses with branches of the superficial peroneal nerve.
Medial Ankle
Medial Ligament
Deltoid Ligament
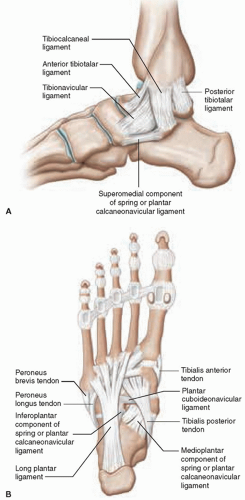
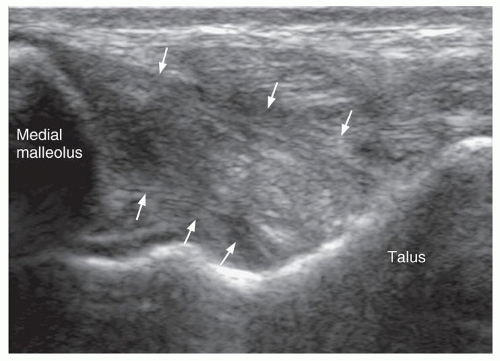
The deltoid ligament is a strong, fan-shaped ligament extending from the medial malleolus to insert on the posterior talus, sustentaculum tali of the calcaneum, anterior talus, and navicular (Fig. 8.8A). It has superficial and deep components that are separable on ultrasound. The superficial fibers extend to the navicular bone, spring ligament, and calcaneum, and are known as the tibionavicular, tibiospring, and tibiocalcaneal fibers, respectively. The stronger and shorter deep fibers extend
to the talus and are known as the anterior and posterior tibiotalar fibers. While the superficial and deep fibers are identifiable as separate structures, the individual components of the superficial and deep layers are seen as a continuum. In general, the superficial fibers tend to be located more anteriorly, though considerable overlap does occur. The deltoid ligament is best visualized in a longitudinal plane with the ankle slightly dorsiflexed and the hindfoot everted. The proximal end of the probe is placed on the medial malleolus, while the distal end of the probe is moved in a fan-shaped manner to show all components (Fig. 8.9). The anterior and mid-fibers are not as consistently well visualized as the posterior fibers which run posteriorly and inferiorly to the talus.17 The deltoid ligament is normally 4- to 5 mm thick in its mid-portion.18 On transverse scanning, the tibialis posterior tendon crosses the superficial component of the deltoid ligament.
to the talus and are known as the anterior and posterior tibiotalar fibers. While the superficial and deep fibers are identifiable as separate structures, the individual components of the superficial and deep layers are seen as a continuum. In general, the superficial fibers tend to be located more anteriorly, though considerable overlap does occur. The deltoid ligament is best visualized in a longitudinal plane with the ankle slightly dorsiflexed and the hindfoot everted. The proximal end of the probe is placed on the medial malleolus, while the distal end of the probe is moved in a fan-shaped manner to show all components (Fig. 8.9). The anterior and mid-fibers are not as consistently well visualized as the posterior fibers which run posteriorly and inferiorly to the talus.17 The deltoid ligament is normally 4- to 5 mm thick in its mid-portion.18 On transverse scanning, the tibialis posterior tendon crosses the superficial component of the deltoid ligament.
Tip:
The deltoid ligament is composed of superficial and deep fibers. The separate components of the fibers are inseparable on ultrasound.
Spring Ligament Complex
The spring (plantar calcaneonavicular) ligament complex is located between the calcaneus and navicular on the medial and inferoplantar aspects of the foot. It helps to support the head of the talus and, with the tibialis posterior tendon, forms a crucial support for the medial longitudinal arch19 (Figs. 8.8A, B). It has superomedial, oblique medioplantar, and inferoplantar components (also known respectively as the medial, intermediate, and lateral components). The superomedial fibers are functionally the most important, and extend from the sustentaculum tali, over the surface of talar head, to
insert onto the superomedial aspect of the navicular. There is a “gliding layer” of fibrocartilage between these fibers and the overlying posterior tibial tendon, though this gliding layer is not seen as a discrete separate structure on ultrasound imaging. There are also some connecting collagenous fibers between the posterior tibial tendon and the superomedial fibers of the spring ligament. The superomedial fibers are seen as an echogenic band just deep to the posterior tibial tendon,20 best demonstrated by placing the probe with one end over the sustentaculum tali and the other over the talar head and medial aspect of the navicular bone.20 The superomedial component of the spring ligament can also be seen deep to the posterior tibial tendon just proximal to the tendon insertion when the tendon is scanned transversely. Proximally, the normal thickness of the superomedial component of the spring ligament is 4 mm overlying the talar head.21 The medioplantar and inferoplantar components of the spring ligament are functionally less important and not consistently seen on ultrasound (Fig. 8.8B).
insert onto the superomedial aspect of the navicular. There is a “gliding layer” of fibrocartilage between these fibers and the overlying posterior tibial tendon, though this gliding layer is not seen as a discrete separate structure on ultrasound imaging. There are also some connecting collagenous fibers between the posterior tibial tendon and the superomedial fibers of the spring ligament. The superomedial fibers are seen as an echogenic band just deep to the posterior tibial tendon,20 best demonstrated by placing the probe with one end over the sustentaculum tali and the other over the talar head and medial aspect of the navicular bone.20 The superomedial component of the spring ligament can also be seen deep to the posterior tibial tendon just proximal to the tendon insertion when the tendon is scanned transversely. Proximally, the normal thickness of the superomedial component of the spring ligament is 4 mm overlying the talar head.21 The medioplantar and inferoplantar components of the spring ligament are functionally less important and not consistently seen on ultrasound (Fig. 8.8B).
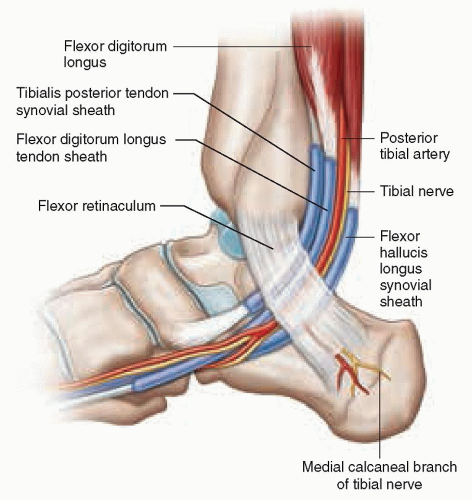
Medial Tendons
The tendons that run posterior to the medial malleolus are from anterior to posterior (or medial to lateral), the posterior tibial (tibialis posterior), flexor digitorum longus (FDL), and flexor hallucis longus (FHL) tendons. The neurovascular bundle, comprising the posterior tibial vessels and tibial nerve, lies between the FDL and FHL tendons (Fig. 8.10). The arrangement can be memorized by “Tom, Dick, And Harry” from anterior to posterior (Tom = Tibialis posterior, Dick = FDL, And = posterior tibial Artery, concomitant veins and tibial nerve, and Harry = FHL). In the retromalleolar region, they are covered by the flexor retinaculum to form a fibro-osseous tarsal tunnel.22 The retinaculum is a thin (<1 mm) echogenic band extending from the medial malleolus to the posterosuperior aspect of the calcaneus. The proximal tunnel is covered by a deep aponeurosis of the leg and has an osseous floor formed by the tibia and the talus. The more distal tunnel is covered by the flexor retinaculum and the fascial covering of the abductor hallucis muscle and has an osseous floor formed by the calcaneus, sustentaculum tali, and inferomedial navicular.
The tibial nerve trifurcates about 1.5 cm proximal to the tip of the medial malleolus.23 Its first branch is the sensory medial calcaneal nerve, which arises proximal to the flexor retinaculum in 40% of subjects. When it does so, sensory deficit due to compression of the tibial nerve in the tarsal tunnel tends to spare the heel.24 The tibial nerve then divides into the medial and lateral plantar nerves, deep to the flexor retinaculum and separated by the interfascicular septum. The medial plantar nerve runs with the posterior tibial tendon along the medial aspect of the foot to innervate the small muscles (abductor hallucis, flexor hallucis brevis, flexor digitorum brevis, and the first lumbrical muscles). The lateral plantar nerve descends under the midfoot to innervate the small muscles on the lateral side of the foot (abductor digiti minimi, abductor hallucis, quadratus plantae, interosseous muscles, second to fifth lumbricals).
The posterior tibial tendon is held against the posteromedial aspect of the medial malleolus by the flexor retinaculum. It courses around the inferior tip of the medial malleolus. The inframalleolar segment of the tendon runs over the deltoid ligament and the body of the calcaneum before inserting on the plantar aspects of the medial pole of the navicular, the cuneiforms, and the second to fourth metatarsal bases. Its tendon sheath extends from just distal to the musculotendinous junction to 1 to 2 cm proximal to the navicular insertion. The tendon sheath is usually dry, but a trace of fluid (<2 mm in thickness and not circumferential) is normal. The posterior tibial tendon is best examined in short axis in the supra-, retro-, and inframalleolar regions. Distally, it is best examined in long axis as this allows easier evaluation of the insertion. The posterior tibial tendon normally fans out near its insertion, leading to thickening and hypoechogenicity that may mimic a tendon tear or tendinosis. It may insert into an elongated (cornuate) medial pole
of the navicular or an accessory navicular. The normal cross-sectional area/mean width of the posterior tibial tendon are: retromalleolar <0.16 cm2/<2 mm; inframalleolar <0.18 cm2/<2.5 mm; and pre-insertional <0.27 cm2/<3.5 mm. The retromalleolar and inframalleolar segments of the posterior tibial tendon are about twice the size of the adjacent FDL tendons. The largest variability in size of the posterior tibial tendon is the most distal portion where it flares out to insert onto the undersurface of the navicular medially, the three cuneiforms, and the medial metatarsal bases.25
of the navicular or an accessory navicular. The normal cross-sectional area/mean width of the posterior tibial tendon are: retromalleolar <0.16 cm2/<2 mm; inframalleolar <0.18 cm2/<2.5 mm; and pre-insertional <0.27 cm2/<3.5 mm. The retromalleolar and inframalleolar segments of the posterior tibial tendon are about twice the size of the adjacent FDL tendons. The largest variability in size of the posterior tibial tendon is the most distal portion where it flares out to insert onto the undersurface of the navicular medially, the three cuneiforms, and the medial metatarsal bases.25
Tip:
The retromalleolar and inframalleolar portions of the posterior tibial tendon are about twice the size of the EDL tendon.
The FDL tendon lies immediately posterolateral to the posterior tibial tendon behind the medial malleolus. It is important on transverse scanning to appreciate whether both tendons are present, as FDL can slip forward if tibialis posterior is ruptured and simulate a normal tibialis posterior tendon. In the inframalleolar region, FDL separates from the posterior tibial tendon and runs superficial to the sustentaculum tali. The normal caliber of the FDL is approximately half that of the tibialis posterior. Usually, there is no detectable fluid within the FDL tendon sheath on ultrasound.26
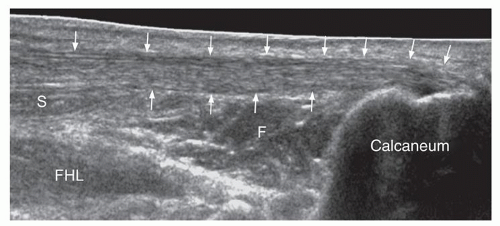
The FHL tendon is the most posterior and deepest ankle tendon in the medial ankle. The fleshy muscle belly extends to the level of the ankle joint. The tendon originates behind the ankle joint and lies in a fibro-osseous inframalleolar groove between the medial and lateral talar tubercle. The tendon is covered by the retinaculum and may become entrapped by reactive changes affecting the posterior talar process. Distally, the tendon courses inferior to the sustentaculum tali before inserting on the base of the distal phalanx of the hallux. Due to its deep location, it is less easily appreciated than the other medial ankle tendons on ultrasound. The retromalleolar portion is best seen on sagittal scanning medial to the Achilles tendon. Passive flexion and extension of the big toe during scanning help to confirm continuity of the FHL. In the hindfoot, FHL crosses the tendon of FDL to which it is connected by a thin fibrous slip. In 20% of normal individuals, the FHL tendon sheath communicates with the ankle joint, and an ankle effusion may result in considerable fluid distension of the FHL tendon sheath.
Tip:
Scanning in a sagittal plane medial to the Achilles tendon while flexing the big toe will help confirm continuity of FHL tendon.
Posterior Ankle
Posterior Ligaments
The posterior inferior tibiofibular and posterior intermalleolar ligaments are deep, not entirely accessible by ultrasound and better assessed by MRI. The posterior tibiofibular ligament is a short ligament between the posterior tibia and fibula. The posterior intermalleolar ligament is present in half of normal subjects and extends obliquely from the superior margin of the medial malleolus to the superior margin of the fibular malleolar fossa where it attaches just proximal to the posterior talofibular ligament.27
Posterior Tendon Groups
The Achilles tendon, the largest tendon in the human body, is a merger of the tendons of the triceps surae (i.e., gastrocnemius and soleus muscles) (Fig. 8.11). The gastrocnemius muscle ends in the mid-calf, soleus more distally. The Achilles tendon inserts via a broad attachment on the posterosuperior aspect of the calcaneus28 (Fig. 8.12). There is a narrow band of fibrocartilage binding the tendon to the bone. The tendon is moderately echogenic with fine parallel echogenic lines on longitudinal scanning. It is generally oval-shaped with a flat or concave anterior border on transverse scanning and is covered by an incomplete tendon sheath or paratenon that envelops the dorsum and sides of the tendon. The paratenon is a thin echogenic band that outlines the moderately echogenic tendon. Anterior to the distal tendon is an echogenic fat pad known as
Kager’s fat. There are two bursae at the insertion. The retrocalcaneal bursa is a comma-shaped hypoechoic structure (2 to 3 mm in depth) between the tendon and the calcaneus. A subcutaneous bursa lies between the tendon and the skin. It is usually not distended or visible. Focal tendon calcification, fluid in the retrocalcaneal bursa, and bony contour abnormalities at the calcaneal insertion are seen in 2%, 35%, and 63% of asymptomatic subjects.28 The normal Achilles tendon is 4 to 6 mm (mean 5.3 mm) wide and 5 to 6 cm long, although size is greater in taller and heavier subjects, and in men.24,25 Achilles tendon measurements are best made on transverse scanning as measurements made on longitudinal scanning tend to be overestimations due to tendon obliquity. Vascularity on Doppler ultrasound is normally minimal or absent.28 The middle third of the tendon is almost avascular,28 while the proximal and distal portions are better vascularized from the soleus muscle belly and calcaneal periosteum, respectively. The Achilles tendon receives its sensory nerve supply from the nerves innervating the adjacent muscles and from cutaneous nerves, such as the sural nerve.29
Kager’s fat. There are two bursae at the insertion. The retrocalcaneal bursa is a comma-shaped hypoechoic structure (2 to 3 mm in depth) between the tendon and the calcaneus. A subcutaneous bursa lies between the tendon and the skin. It is usually not distended or visible. Focal tendon calcification, fluid in the retrocalcaneal bursa, and bony contour abnormalities at the calcaneal insertion are seen in 2%, 35%, and 63% of asymptomatic subjects.28 The normal Achilles tendon is 4 to 6 mm (mean 5.3 mm) wide and 5 to 6 cm long, although size is greater in taller and heavier subjects, and in men.24,25 Achilles tendon measurements are best made on transverse scanning as measurements made on longitudinal scanning tend to be overestimations due to tendon obliquity. Vascularity on Doppler ultrasound is normally minimal or absent.28 The middle third of the tendon is almost avascular,28 while the proximal and distal portions are better vascularized from the soleus muscle belly and calcaneal periosteum, respectively. The Achilles tendon receives its sensory nerve supply from the nerves innervating the adjacent muscles and from cutaneous nerves, such as the sural nerve.29
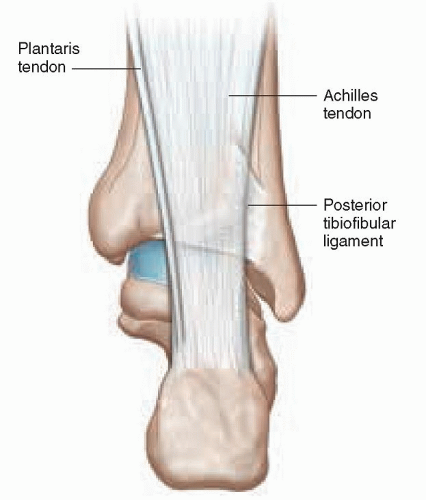 Figure 8.11. Schematic diagram of the posterior tendons showing the Achilles tendon and the plantaris tendon medially. The posterior tibiofibular ligament is also shown. |
Tip:
Measurements of the Achilles tendon are best made on transverse sections.
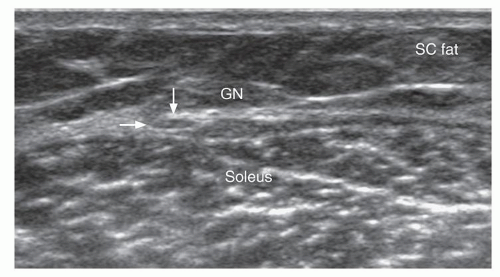
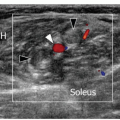
The plantaris muscle, which is present in about 90% of the population, has a short (7 to 10 cm) muscle belly arising from the lateral supracondylar region of the femur superficial to the origin of the lateral head of gastrocnemius.30 The long slender plantaris tendon runs inferomedially, deep to the medial belly of gastrocnemius, to the medial side of the Achilles tendon, and either fuses with the Achilles tendon or inserts into the flexor retinaculum or the calcaneus. The myotendinous junction of plantaris is in the upper calf region.31 The tendon is a thin ribbon-like structure between the medial head of gastrocnemius and the soleus muscle proximally, medial to the Achilles tendon distally (Fig. 8.13). It is best identified just proximal to the Achilles myotendinous junction, deep to the medial belly of gastrocnemius, as a small oval hyperechoic structure with an internal fibrillar appearance (Fig. 8.13). The whole course of the tendon may be traced, although it is more difficult to trace proximally than distally. Plantaris should be distinguished from an accessory soleus muscle and tendon. The accessory soleus muscle is a larger more fleshy structure, usually located at the anteromedial aspect of the Achilles tendon, and its tendon inserts into the medial side of the calcaneum.
Posterior Ankle Joint
Fluid distension of the posterior recess of the ankle joint is best appreciated with the patient prone and can lead to unusual configurations such as an inverted “figure of 3” shape due to fluid bulging between the posterior tibiofibular and tibiotalar ligaments.
The posterior talocalcaneal articulation is continuous with the ankle joint in about 20% of normal subjects. The posterior talar process originates from a secondary ossification center that mineralizes between 7 and 14 years and fuses with the talar body within a year to form the lateral talar tubercle. If elongated, it is called a trigonal (Stieda) process. Failure of fusion occurs in approximately 25% of subjects, and the resulting ossicle, or os-trigonum, articulates via a synchondrosis with the talus. Ultrasound cannot usually distinguish between an os-trigonum and a Stieda process as acoustic shadowing precludes assessment of any synchondrosis.
Tip:
All the tendons crossing the ankle joint are enclosed in a tendon sheath except for the Achilles tendon (which has a paratenon) and the plantaris tendon. Only the Achilles paratenon can be seen in normal subjects on ultrasound. The synovial sheaths of the other ankle tendons cannot be seen in normal subjects.
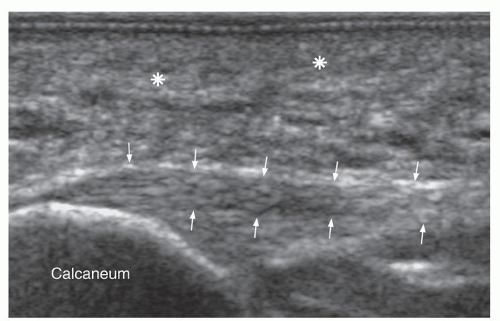
Foot
Plantar Foot
The plantar fascia is examined with the patient prone or supine. The plantar fascia is not strictly fascial but can be regarded as a common tendon aponeurosis for the superficial layer of the intrinsic plantar foot muscles. It is a thin structure that arises from the medial and lateral inferior calcaneal tubercles and attaches to the plantar plates of the metatarsophalangeal joints and the proximal phalangeal bases. It is a homogeneous echogenic band with internal linear interfaces on longitudinal scans, normally 2- to 3.6-mm thick near its calcaneal origin (Fig. 8.14), becoming thinner (1 to 2 mm) and more superficial distally. It comprises a thicker central cord and smaller medial and lateral cords that are not distinct entities but merge indistinguishably with each other. The plantar fascia is the main supporting structure for the longitudinal arches of the foot, connecting the posteroinferior calcaneus and the proximal phalanges.
The intertarsal joints, tarsometatarsal joints, metatarsophalangeal and interphalangeal joints, and their ligaments are assessed individually. The Lisfranc ligament extends obliquely between the lateral aspect of the medial cuneiform and the medial aspect of the second metatarsal base and is an important stabilizer of the tarsometatarsal joints, although it is not assessable by ultrasound. The normal joint space between the medial cuneiform and second metatarsal base is <1.0 mm.32
The sinus tarsi is an area bounded by the talus, calcaneum, talonavicular joint, and the posterior compartment of the subtalar joint. It contains the cervical and talocalcaneal interosseous ligaments, inferior extensor retinaculum, fat, and nerve endings of the deep peroneal nerve. The interosseous ligaments cannot be seen on ultrasound as they are deep, partially obscured by bone, and surrounded by adjacent echogenic sinus fat. The sinus tarsi region can be assessed by placing the probe anteroinferior to the tip of the lateral malleolus and angling toward the anterior subtalar joint.
Small plantar digital nerves and their accompanying vessels run between the metatarsal bones. The diameter of the normal plantar digital nerve is 1 to 2 mm at the level of the intermetatarsal heads, and the nerve can be seen on high-resolution (>10 MHz) ultrasound. The intermetatarsal bursa is normally present in each interspace, dorsal to the deep transverse intermetatarsal ligament and neurovascular bundle, and just proximal to the metatarsal head.33 The bursa may reach ≤3 mm in asymptomatic subjects.34
The capsulo-ligamentous-sesamoid complex on the plantar aspect of the first metatarsophalangeal joint includes the joint capsule, collateral ligaments, fibrous plantar plate, and the flexor hallucis brevis, abductor hallucis, and adductor hallucis tendons. Flexor hallucis brevis originates on the cuboid and lateral cuneiform and splits beneath the first metatarsal into medial and lateral tendons that blend with the medial and lateral sesamoid bones just proximal to inserting into the proximal phalanx. The sesamoids are paired oval hyperechoic structures with posterior acoustic shadowing. The sesamoids are embedded in the medial and lateral tendon slips of the flexor hallucis brevis muscle and in the tendon of abductor hallucis muscle. Between the sesamoid bones runs the FHL tendon and deep to this, the thick interconnecting intersesamoid ligament. The sesamoids are bipartite in about 10% of subjects. In this situation, the summated width of the two bipartite ossicles is more than the width of the normal adjacent sesamoid allowing the distinction of bipartite sesamoid to be made.
The plantar plate is a triangular thick biconcave hyperechoic fibrocartilaginous structure on the plantar aspect of the metatarsophalangeal joints. It is firmly attached to the proximal phalanx and extends posteriorly to cover the articular cartilage on the plantar aspects of the metatarsal heads. The plantar plates are connected at the sides to the collateral ligaments of the metatarsophalangeal joints. The long and short toe flexors, invested in a synovial sheath, run just superficial to the plantar plates within a common fibrous sheath. In full-thickness tears of the plantar plate, the tendon sheath may communicate with the metatarsophalangeal joint.
Dorsal Foot
The tibialis anterior, EHL, and the four slips of the EDL tendons can be identified on the dorsal aspect of the midfoot (Fig. 8.3). The most medial tendon is the tibialis anterior tendon, which tapers distally to insert on the anteromedial aspect of the first cuneiform and the base of the first metatarsal bone. The distal portion of this tendon is more medial than dorsal and may normally show a mild longitudinal separation just prior to insertion. This
should not be confused with a longitudinal split tear. The EHL tendon is thin and more easily appreciated by passive flexion and extension of the big toe. The four diverging slips of EDL insert onto the middle and distal phalanges of the toes. Peroneus tertius may be seen as an accessory fifth lateral slip of the EDL extending toward the base of the fifth metatarsal bone. The dorsal pedis artery and medial branch of the deep peroneal nerve both run between EHL and EDL distal to the ankle joint. The medial branch of the deep peroneal nerve lies just lateral to the dorsalis pedis artery.
should not be confused with a longitudinal split tear. The EHL tendon is thin and more easily appreciated by passive flexion and extension of the big toe. The four diverging slips of EDL insert onto the middle and distal phalanges of the toes. Peroneus tertius may be seen as an accessory fifth lateral slip of the EDL extending toward the base of the fifth metatarsal bone. The dorsal pedis artery and medial branch of the deep peroneal nerve both run between EHL and EDL distal to the ankle joint. The medial branch of the deep peroneal nerve lies just lateral to the dorsalis pedis artery.
The intertarsal, tarsometatarsal, metatarsophalangeal, and interphalangeal joints and corresponding ligaments are assessed individually. A small amount of fluid in the dorsal recess of the metatarsophalangeal or interphalangeal joints is normal. Extensor digitorum brevis and extensor hallucis brevis are the only muscles on the dorsal foot. They extend from the superolateral aspect of the calcaneus (just lateral to sinus tarsi) to the toes, the flat muscle belly lying deep to the EDL tendons.34 The extensor hallucis brevis muscle is on the medial aspect of the extensor digitorum brevis muscle belly and may be indistinguishable from it. The extensor digitorum tendons insert into the lateral aspects of the EDL tendons.
Tip:
A small effusion in the dorsal recesses of the small joints of the toes is normal and should not be misinterpreted as synovitis.
ANKLE PATHOLOGY
Tendon Pathology
Anterior Tendons
The anterior tendons are the least prone of all the ankle tendons to tendinosis or tenosynovitis, and of these the tibialis anterior is the most commonly affected (Fig. 8.15). It is the strongest dorsiflexor of the ankle and also assists foot inversion. As it runs a relatively straight course within a fibrous tunnel, the mechanical demands on the tendon are low. Complete tears are rare but can result from acute injury or spontaneous rupture of a chronically degenerate tendon.3 Acute rupture usually presents in younger patients and acute-on-chronic spontaneous rupture in elderly patients, predominantly males.35,36 Predisposing factors include diabetes mellitus, inflammatory arthropathy, gout, and local steroid injections. The distal tendon is relatively avascular, and this, together with friction against the retinaculum, may explain why most tears occur distally. Ruptures occur at the medial cuneiform, beneath the superomedial limb of the inferior extensor retinaculum, or just distal to the superior extensor retinaculum. Ultrasound shows complete fiber discontinuity. The proximal end of the tendon usually retracts, appears moderately enlarged and hypoechoic, and is typically located deep to the superomedial limb of the inferior retinaculum. It may manifest clinically as a soft tissue mass anterior to the ankle joint. The distal end of the tendon tends not to swell or retract to the same degree and is not as well seen.
The next most common disorder of the tibialis anterior tendon is tendinosis of the distal tendon, which results in a swollen, hypoechoic tendon.5 Partial tears can occur on a background of tendinosis, usually located near the superomedial limb of the inferior retinaculum.3,37 The tendon is focally swollen to a moderate degree and hypoechoic. Surface fraying or a discrete partial tear may be visible. Small partial tendon tears may be too small to detect, although swelling and hypoechogenicity are apparent.
Tenosynovitis, tears precipitated by large dorsal osteophytes, and cortical avulsion at the distal insertion are occasionally encountered in EHL and EDL.
Tip:
Tears of the tibialis anterior tendon may present as a mass anterior to the ankle joint.
Lateral Tendons
The peroneus longus and brevis tendons primarily evert the foot and stabilize the ankle. After the Achilles and posterior tibial tendons, disorders of the peroneal tendons are the next most common.
Tenosynovitis and Tendinosis
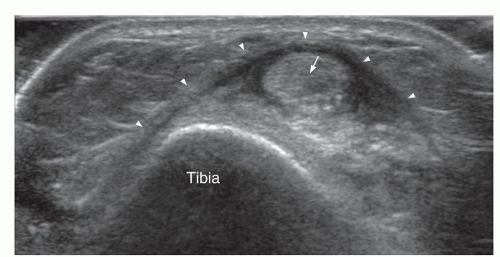
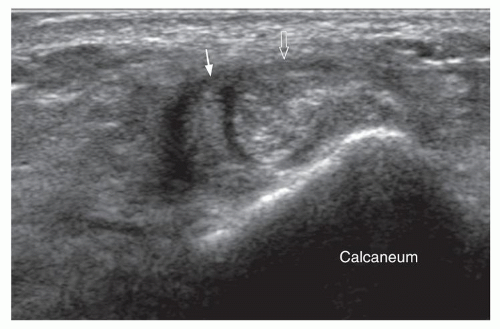
Tenosynovitis and tendinosis are the most frequent abnormalities. Tenosynovitis is primarily a disease of the tendon sheath with secondary involvement of the tendon, while tendinosis is primarily a disease of the tendon with secondary involvement of the tendon sheath. In most ankle tendons, one or other predominates, but in the peroneal tendons, a mixed picture with features of both
tends to occur. Tenosynovitis produces distension of the tendon sheath with synovial proliferation ± fluid, peritendinous hyperemia, and a relatively unaffected tendon. Tendinosis manifests as tendon thickening, hypoechogenicity, intratendinous tears, and a variable degree of peritendinitis (Fig. 8.16). The more severe the tendinosis, the greater the likelihood of a tendon tear (Fig. 8.17). Tendons are prone to tendinosis at areas of greatest physical stress, and for the peroneal tendons this occurs at the tip of the lateral malleolus, around the peroneal tubercle and in the cuboid groove (for peroneus longus). Several anatomical variants predispose to tendinosis. A low-lying peroneus brevis muscle belly or an accessory peroneus quartus muscle can lead to stenosis within the fibro-osseous retromalleolar tunnel and stretching of the superior peroneal retinaculum. Hypertrophy of the peroneal tubercle, particularly if >5 mm in height, or a varus hindfoot alignment increase stress on the tendons.
tends to occur. Tenosynovitis produces distension of the tendon sheath with synovial proliferation ± fluid, peritendinous hyperemia, and a relatively unaffected tendon. Tendinosis manifests as tendon thickening, hypoechogenicity, intratendinous tears, and a variable degree of peritendinitis (Fig. 8.16). The more severe the tendinosis, the greater the likelihood of a tendon tear (Fig. 8.17). Tendons are prone to tendinosis at areas of greatest physical stress, and for the peroneal tendons this occurs at the tip of the lateral malleolus, around the peroneal tubercle and in the cuboid groove (for peroneus longus). Several anatomical variants predispose to tendinosis. A low-lying peroneus brevis muscle belly or an accessory peroneus quartus muscle can lead to stenosis within the fibro-osseous retromalleolar tunnel and stretching of the superior peroneal retinaculum. Hypertrophy of the peroneal tubercle, particularly if >5 mm in height, or a varus hindfoot alignment increase stress on the tendons.
Peroneal Tendon Tear
Most peroneal tendon tears are longitudinal, intrasubstance partial-thickness tears, or split tears38 (Fig. 8.17). Complete tears are uncommon and are transverse39. Tears of a healthy tendon may occur during acute ankle inversion. More commonly longitudinal tears, usually 2- to 5-cm long, occur in middle-aged patients on a background of tendinosis. Predisposing factors include tendon subluxation, a bony spur at the lateral malleolus, distal fibular or calcaneal fracture, or an os peroneum. Peroneus brevis tends to tear in the retromalleolar sulcus where it may be compressed by the overlying peroneus longus tendon. With more severe tears, peroneus brevis assumes a horseshoe shape on transverse scanning into which insinuates the peroneus longus tendon. Peroneus brevis may eventually split into two tendons, resulting in three apparent tendons being visible instead of the normal two in the retromalleolar region,40,41 not to be confused with a concurrent peroneus quartus tendon, which usually inserts onto the retrotroclear eminence of the calcaneus. An effusion of the common peroneal tendon sheath is often present, and helps in visualization of the tendon tear. Dynamic examination with plantar or dorsiflexion may also accentuate any longitudinal tendon splits. Occasionally, multiple splits may occur, and the tendon looks like a horsetail at surgery.
Tip:
The peroneus brevis tendon is more prone to tear. Tears normally occur near the fibular tip and extend proximally and distally. Three rather than two tendons may be seen than peroneus longus.
Peroneus longus tends to tear near the peroneal tubercle and the cuboid groove. An os peroneum predisposes peroneus longus to tendinosis, partial splits, and complete tears, and the combination is known as os peroneum syndrome. An os peroneum is prone to fracture or stress reaction. A fracture is seen as a large gap in the ossicle with irregular margins usually associated with a full-thickness peroneus longus tendon tear.13 The tendons and bone fragments retract ≥6 mm and have irregular margins, surrounding soft tissue swelling and tenderness on transducer pressure.10,13 In an undisplaced os peroneum fracture or bipartite os peroneum, the gap is usually <2 mm. Stress reaction of the os peroneum and cuboid marrow edema in peroneal tendinosis are best seen on MRI.1,10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree