Hard signs
Soft signs
Shock
Non-pulsatile bleeding
Pulsatile bleeding
Stable hematoma
Bruit or thrill over the wound(s)
Nerve injury
Expanding or pulsatile hematoma
Unequal blood pressures
Absent palpable pulses distally
Proximity of injury tract
Limb ischemia
Distal ischemic manifestations (pain, pallor; paralysis, paresthesias, poikilothermy)
There is growing evidence that most of these injuries heal spontaneously or stabilize without further compromising the distal circulation and perfusion [6].
Vascular injuries may be initially undiagnosed in hemodynamically stable patients, so a detailed clinical history including the mechanism of the trauma is important. Factors that can jeopardize diagnosis of acute vascular injuries usually are the presence of distraction injuries, lack of correlation with clinical presentation, radiologist experience, or inadequate CT scan protocol [7].
Subclinical vascular injuries with intact distal perfusion may be observed with serial monitoring, antiplatelet therapy or systemic anticoagulation, and repeat noninvasive imaging [8].
Subclinical vascular defects have been defined as those exhibiting the following characteristics:
- 1.
Low-velocity injury
- 2.
Minimal (<5 mm) arterial wall disruption for intimal defects and pseudoaneurysm (PSA)
- 3.
Adherent or downstream protrusion of intimal flaps
- 4.
Intact distal circulation
- 5.
No active hemorrhage
The liberal use of imaging in the presence of any hard sign to confirm or exclude vascular injury is recommended [4].
Most hard signs in this setting (as much as 87%) are not due to vascular injury, but rather to soft tissue and bone bleeding, traction of intact arteries with pulse loss, or compartment syndrome [9].
If significant vascular injuries (such as occlusion, extravasation, or transection) are excluded, the treatment of soft tissue and skeletal injuries may proceed. How reperfusion is achieved depends on the patient’s hemodynamic status, physiologic parameters, skeletal stability, wound characteristics, and resource availability [10].
Vascular imaging is mandatory when expectant management is chosen, but resolution can be seen in 85–90% of these lesions with no operative intervention [11].
Doppler Ultrasound (DUS) has shown an overall accuracy of 98% for diagnosing vascular injury, but it requires time and high experience [1].
DUS provides additional information on clinical examination but there is not consensus in the literature about its importance in the diagnostic management in the injuries of the limbs in trauma patient. DUS can be obtained rapidly and used to detect occlusion, intimal flaps, and luminal defects [12].
For the lower limbs evaluation a DUS assessment should be done also to confirm the absence of pedal pulses and to perform an ankle-brachial index (ABI) when possible. In emergency traumatic setting, an ABI is useful for the evaluation of a patient who is at increased risk for lower extremity arterial injury: an ABI < 0.90 suggests a need for further vascular imaging, whereas an ABI > 0.90 decreases the likelihood of an arterial injury, and the patient may be observed with serial ABI assessments or may undergo a vascular study on a delayed basis [13].
DUS has some diagnostic limitations in locating the exact point of artery cutoff point and the traumatized area. Moreover, the DUS evaluation of the vascular limbs injuries, especially in trauma patients, requires high level of expertise; it is highly operator dependent and can be time-consuming [14].
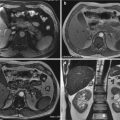
Large retrospective reviews have shown that Computed Tomography Angiography (CTA) significantly increases the probability of survival in polytrauma patients [15].
It has the added advantage of simultaneously being able to assess extensive body areas as well as demonstrating associated soft tissue and bony injuries.
CTA has dramatically improved over the last few years and has overtaken catheter angiography as the initial first choice diagnostic tool in the trauma patients [4].
While traditional angiography has been the gold standard and affords opportunity for intervention, the ability to rapidly acquire high-specificity diagnostic imaging with spiral CTA has been a game changer as a rapid screening test and plays a major role in the management of multi-trauma patients.
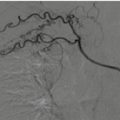
Digital Subtraction Angiography (DSA) is the diagnostic standard for vascular injury and allows for therapeutic intervention [16].
CTA has a sensitivity of 90–95% and specificity of between 98% and 100% for the detection of upper and lower limbs arterial injuries [16]. CTA may be limited by poor arterial opacification, motion artifact, streak artifact from adjacent metallic fragments, or slowing of flow beyond injured sites [16]. CTA has nowadays replaced catheter angiography as the primary imaging technique to evaluate patients with suspected acute vascular injuries [7, 10, 17]. Nevertheless, some investigators still recommend DSA as the primary imaging test, particularly in patients with finding of metallic fragments or shrapnel on conventional imaging to avoid technical artifacts which may render affected vascular segments non-diagnostic on cross-sectional images [18]. However, in this set, DSA requires an highly trained team readily available at the time of patient admission, it is costly and it is not free from the possibility of serious complications due to catheter insertion, especially in an artery with local hematoma formation, vessel thrombosis and, in more severe cases, post-angiography dissection, embolization and pseudoaneurysm formation [19–21].
CTA pledge the acquisition of three-dimensional images with submillimetric spatial resolution of the entire body, from head to foot in only a few seconds with a single contrast bolus, and state-of-the-art workstations allow Multiplanar Reformations (MPR), Maximum Intensity Projection (MIP), and Volume Rendering (VR) reconstructions [10, 21–24].
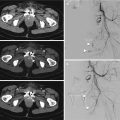
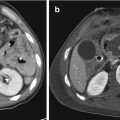
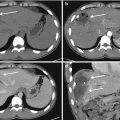
It is of fundamental importance the appropriate selection of scan parameters and CT protocols. It is consolidated knowledge that acquiring images in arterial phase improves the detection of arterial injures, AVF, and PSA while the venous phase is essential to detect venous injuries and to differentiate contained vascular injures from actively bleeding lesions. Therefore, both phases should be routinely included in the whole-body CT evaluation of patients with deceleration injury [17].
All studies should be performed with multiphasic, high-resolution protocol, slice thickness and reconstruction interval value of about 1 mm, before and after administration of intravenous, highly concentrated contrast media (350–400 mgI/mL, with a 3.5–5 ml/s infusion rate, followed by a 25–50 ml bolus of isotonic saline at the same flow rate). The field of view (FOV) should be the smallest including both limbs, to minimize the isotropic voxels and to allow evaluation of symmetry of contrast material arrival time and symmetry of flow. The scan coverage should include both the proximal and distal joints to the region of suspected injury. All study should be performed under the supervision of a radiologist, to evaluate any need of additional late phases. An automated bolus tracking, with region of interest placed at the diaphragmatic aorta (for whole-body scanning) at an attenuation threshold of 100HU, is suggested to time the beginning of the arterial phase, in order to avoid poor timing of the contrast material bolus or bolus outrun [10, 17, 21]. Three-dimensional multiplanar reconstructions and maximum intensity projection should be routinely performed to facilitate recognizing the vessel anatomy and look for possible injuries [10, 17, 21].
Many different vascular injuries can be detected. Active arterial hemorrhage or extravasation can be defined as extravascular contrast media leakage, recognized as hyperattenuating regions with density similar to that of the arteries. Dissection is the evidence of an intraluminal flap with intramural extension of intravenous contrast material. Arteriovenous fistula formation is a communication between an artery and an adjacent vein, with premature venous enhancement. Pseudoaneurysm is a well-contained accumulation of contrast material-enhanced blood beyond the confines of the arterial wall. Narrowing of an artery is an abrupt change in caliber of the vessel within the area of traumatic injury with maintained patency while occlusion of an artery is an abrupt complete termination of an artery. Vessel transection is seen as an abnormality in the vessel contour due to full thickness laceration with free contrast extravasation detectable in the arterial phase [10, 17].
Hemodynamic instability in limbs injuries is more often associated with Penetrating Extremity Trauma (PET) or exposed fractures. In a 14 patient series who died from isolated limb PET, 70% occurred to the lower extremity and 86% were proximal to the elbow and knee [25].
A patient in shock with PET belong in the operating room and no diagnostic studies, except X-rays of the chest, pelvis and the involved extremity are indicated. If there is no inspective evidence that an arterial injury is present but clinical evidence is still strongly suggesting so, DUS, MDCT or DSA can be obtained [8, 14, 26, 27].
25.3 Upper Limb Injuries
Upper extremity trauma patients generally have a lower injury severity score, lower amputation rate, and lower overall mortality when compared to lower extremity injured patients [28].
Upper extremity injuries are more frequently caused by a penetrating mechanism than blunt etiologies. They are usually associated with lower-velocity missiles and a smaller region of injury than lower extremity injuries [28].
Although much of the current state-of-the-art information is the result of wartime observations, the incidence of civilian extremity vascular trauma is significant. It is estimated that subclavian and axillary artery injuries constitute 5–10% of artery trauma in the European and US civilians [29]. Structures concomitantly involved include the brachial plexus, aerodigestive tract, sympathetic chain, and spinal cord [30].
Axillary artery injuries are very similar to subclavian injuries. High axillary injuries may be difficult to expose and gain proximal control for open operative repair. Both supraclavicular and infraclavicular incision may be necessary to achieve adequate control of the vessel for open repair. Moreover, the proximity to the brachial plexus must also be considered [31–33].
Modern IR techniques offer some promises for both adjuvant care with balloon tamponade and definitive treatment by covered stent placement [4].
New advances in vascular techniques and endovascular care have resulted in outstanding success with limb salvage; the coexisting orthopedic, neurologic, and soft tissue injuries most likely determine the outcome [34].
Associated nonvascular injuries usually are associated with consequent disability and functional outcomes [28]. It is essential to have an early multidisciplinary approach to these patients and to define with appropriate scores functional, orthopedic, and vascular lesions [34]. The Multidisciplinary Team (MT) should include surgeon, interventional radiologist, orthopedic, plastic surgeon, hand surgeon, and neurosurgeon.
Excluding ischemia, acute limb loss is frequently from overwhelming and uncontrolled secondary infection so adequate debridement of nonviable tissue and appropriate coverage of vascular and orthopedic repair is essential [11]. Unstable fractures may require stabilization before repair such that ultimate reduction does not strain the vascular repair. Also in this case, communication and intraoperative collaboration between orthopedic surgeon, interventional radiologist, and vascular surgeon should be essential [1].
25.4 Forearm Vessels
Traumatic injuries to the forearm and hand can be penetrating or blunt, which represent 4–36% of upper limb arterial trauma [34]. Because of the close proximity of the vessels and the nerves as they travel in the upper extremities, injuries are rarely just vascular in nature, often complicating not only the presentation but also the long-term outcome. If not treated in a timely fashion and properly, such injuries can lead to loss of function, loss of limb, or even death [35].
Single vessel injury of the forearm can be simply ligated, after making sure that the opposing vessel is intact to the hand and a palmer arch is present [34]. Bedside handheld DUS evaluation of the palmer arch and digital vessels can be performed to confirm viability prior to ligation of the injured vessel. If in-line flow is not present or an incomplete palmer arch is present, primary repair of the injured vessel should be completed [4].
Endovascular approaches and stent graft have no appreciable role in the management of forearm vessel injuries [35].
25.5 Lower Limb Injuries
Patients with lower limb vascular traumas present daily in emergency departments and trauma centers worldwide. According to the National Hospital Ambulatory Medical Care Survey, among approximately 117 million visits to emergency departments in the USA in 2007, 14.6% were for lower extremity injuries [36].
Nowadays, most polytrauma patients will survive, but will not regain their pre-injury level of function; if multiple trauma is survived, lower extremity injuries mainly affect the functional outcome and quality of life in the long term [37].
25.6 Femoral and Popliteal Injuries
Open surgical repair of the femoral vessels at the level of the groin should be undertaken as routine. Primary repair or short saphenous interposition grafts can be used to reconstruct these vessels [1].
The use of covered stent grafts has been described, but long-term patency data is not available [38]. The popliteal artery provides some clinical controversy. It can be a challenging injury to manage. Historically, amputation rates were as high as 20% with injuries in this location [39]. Classic traction injury from posterior knee dislocation can result in injuries ranging anywhere from a small hemodynamically insignificant intimal flaps to critical ischemia and complete transection [1]. In most clinically apparent injuries, open repair is indicated, either by primary repair (stab wounds) or short segmental saphenous vein bypass (blunt injury, gunshot wounds), but there are also the possibility to use covered stent graft repair for trauma and iatrogenic [38, 40].
25.7 Below-Knee Popliteal, Tibial, and Foot Injuries
As with the upper extremity, injury to one terminal vessel in the lower limb can be dealt with by simple ligation. Injury at the level of the tibioperoneal trunk should prompt open surgical reconstruction. Injury to all three tibial arteries should prompt open operative repair of at least two arteries to avoid a potential risk for future amputation [41]. Currently endovascular techniques have not played a major role in the management of tibial arteries injuries.
25.8 The Role of Interventional Radiology in Polytrauma Extremity
In the last two decades, IR shifted the management of vascular disease from traditional open surgery to complex endovascular interventions (EVIs) [4].
On the basis of CTA findings and with the cooperation and support of the other members of the MT team, the interventional radiologist must be increasingly prepared to provide prompt, efficient, and high-quality service [7].
The primary principle in treating acute traumatic arterial injuries is to avoid prolonged ischemia. This reduces the risk of irreversible ischemia and morbidity associated with ischemia reperfusion [42].
Endovascular techniques have the advantages of avoiding general anesthesia, rapid recovery time, lower costs, less tissue trauma in cases of previous soft tissue or bone injuries, and lower chances of infection when there are associated bone fractures; also, there is less risk of collateral flow damage during surgical exposure [43].
Becker et al. [44] were the first to use a stent graft in the management of a penetrating subclavian injury resulting from catheterization.
A systematic review of axillo-subclavian injuries from DuBose et al. found that results of endovascular repair were promising, with an initial success of endovascular stent placement in 96.9% of patients. No mortalities related to endovascular intervention were reported. New neurologic deficits after the use of endovascular modalities were reported in only one patient over 160 treated with endovascular approach [45]. Endovascular management of axillo-subclavian injuries is less technically challenging than open access and has the potential to reduce injury to the surrounding brachial plexus [46].
In all types of EVIs, the basic concepts of catheter-directed treatment of a vascular lesion include access to the vascular tree at a remote site, crossing the offending lesion with a wire, and delivering a device that will allow correction of the lesion [1].
Transcatheter treatments include balloon occlusion, embolization, and endovascular repair with insertion of stent grafts which will be discussed in the following parts. An appreciation of the collateral circulation to the distal extremity is necessary to evaluate the best strategy of treatment and consequently the success and the safety [47].
An integrated endovascular and open approach for the management of polytraumatic patients is sometimes required [1].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree