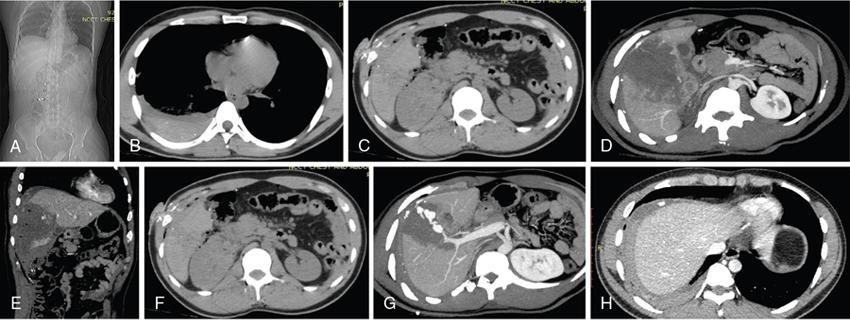
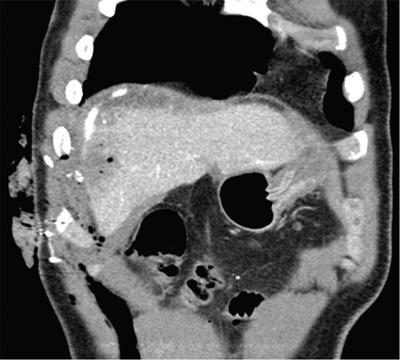
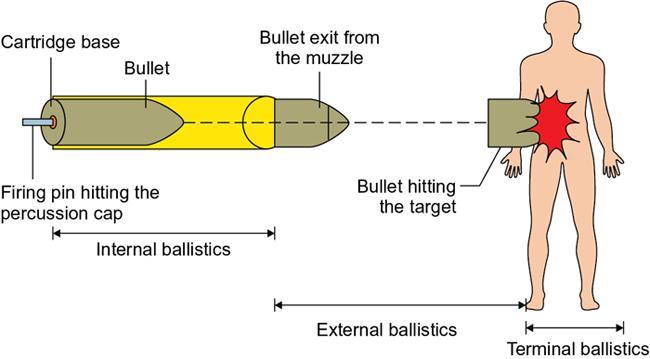
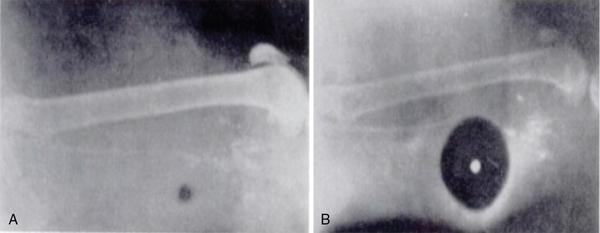
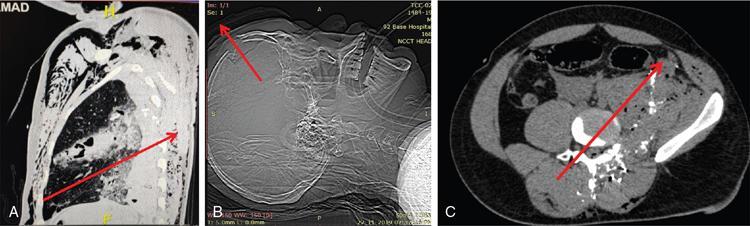
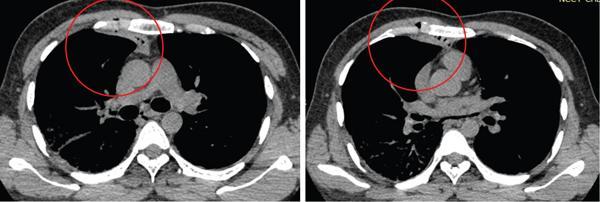
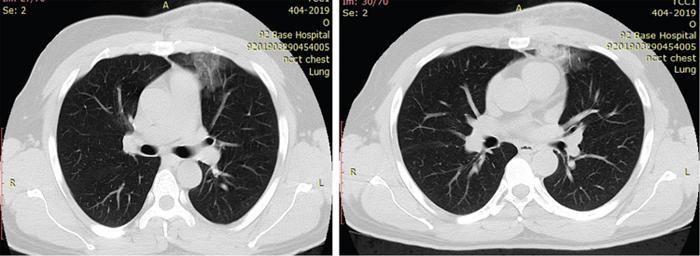
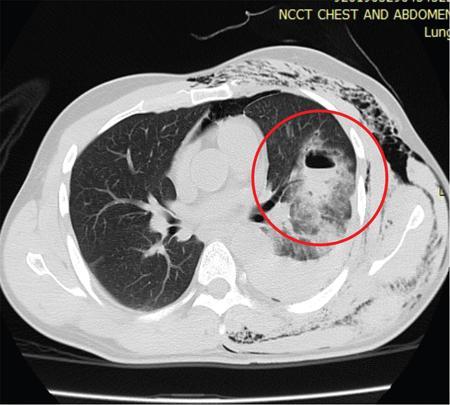
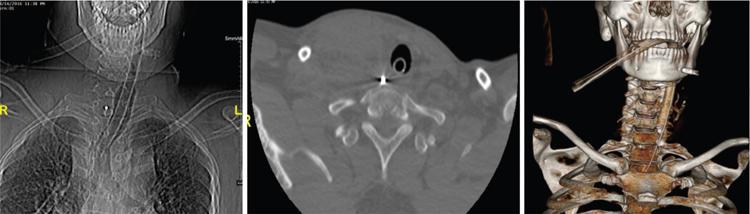
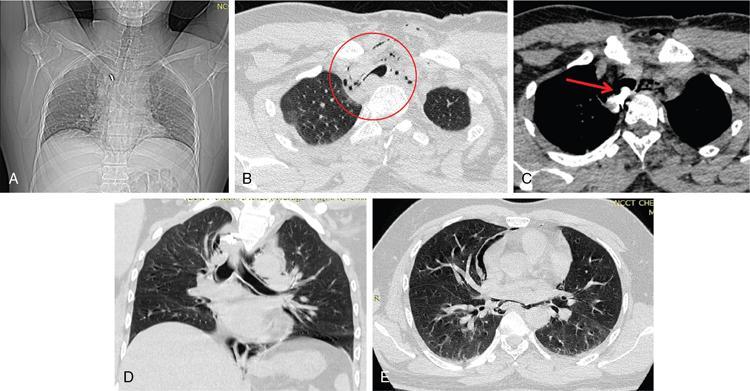
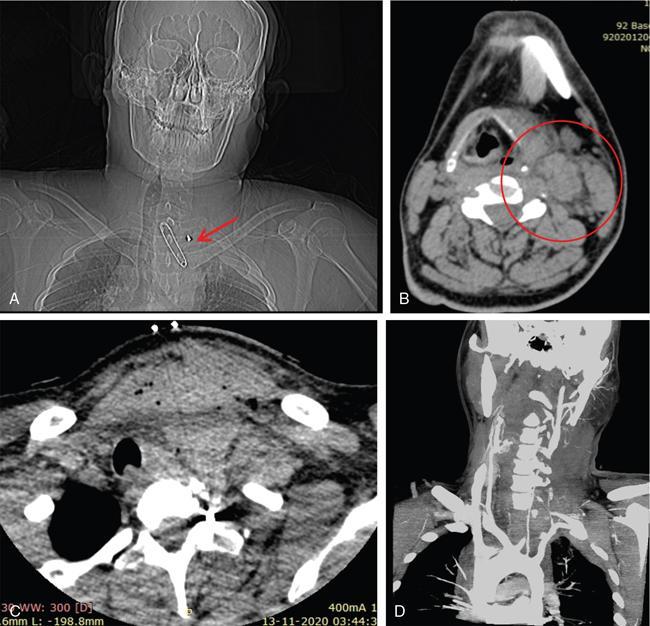
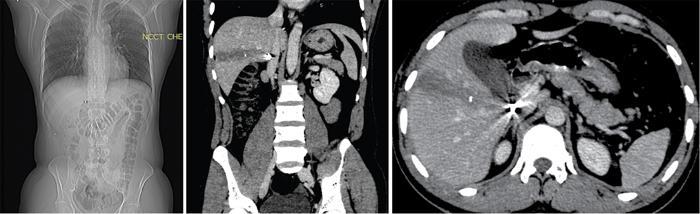
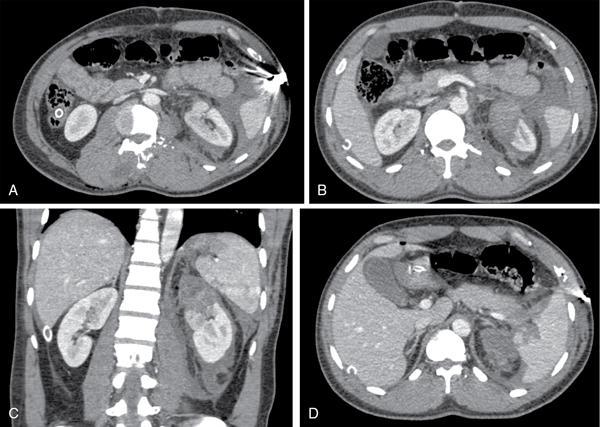
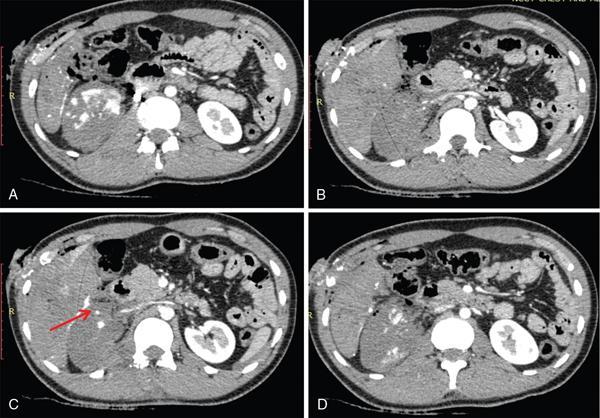
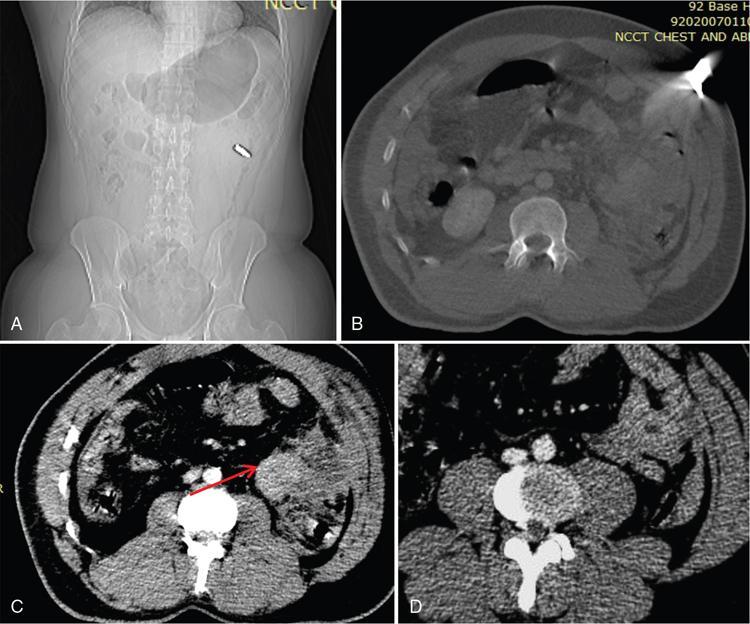
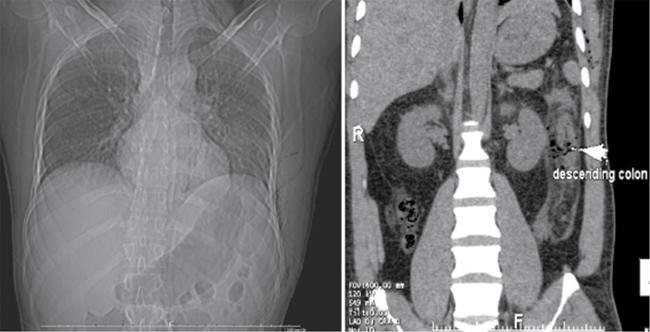
INJURIES DURING WAR R Ravikumar, Manoj Gopinath, Hashim P I, Samarjeet Singh, Somali Pattanayak, Preeti Gupta, Rachit Sharma War is open and declared often intense armed conflict between countries, governments or paramilitary groups with the use of multiple firearms and explosives resulting in extreme violence and severe destruction, leading to multiple injuries and high mortality. Troops are constantly deployed in areas with active insurgencies and hostile borders. Such areas many a times have difficult terrains and hostile weather, and thus, troops can suffer trauma due to various causes. Injuries suffered due to enemy/terrorist actions are generally categorized as combat-related trauma (CRT), which is a significant contributor to mortality and morbidity of troops deployed in active areas. Gunshot wounds, blast injuries and splinter injuries from improvised explosive devices or other explosives, along with blast effects, can inflict dangerous and severe injuries. These injuries may be confounded by altered mental status secondary to head trauma or shock, often along with lack of proper history, which can present challenges in management. Imaging plays a key role in evaluation and management of these cases. Ballistics deals with the study of various aspects related to different projectile/objects in motion. Ballistics comprises three different phases which are considered as various subsets or categories. These are as follows: A subcategory of terminal ballistics is wound ballistics; this part of ballistics deals with the physiological changes induced by the fired projectiles and various aspects of injuries caused to humans. Wound ballistics is thus the most important aspect of ballistics for physicians to understand (Fig. 2.13.1.1). During war, troops can suffer injuries from gunshot wounds (GSWs) from various rifles, blast injury and splinter injuries from artillery, mortar shells and air dropped ordinance including cruise and ballistic missiles. Rifles (e.g. AK 47) are the most common firearms encountered by troops deployed in active insurgencies. The same weapon can, however, be used to fire different types of bullets. There are multiple factors which affect the type and severity of injuries that are caused in the victims. These include (1) weapon type, (2) projectile/firearm used, (3) the distance and angle between the firearm/blast and target, (4) tissue factors such as the type of organ injured. Therefore, not only is it important to know the type and nature of weapon and projectiles, but also it is paramount importance to know how various tissues are affected by and respond to projectile hits. Weapon characteristics: Grooves within the barrel of the rifle give a “spin” to the bullet when fired which. This spin imparted to the bullet has a gyroscopic effect, which gives it directional stability. Rifle bullets have higher velocities and thus have greater wounding potential. Hand guns have lesser velocity but can cause significant damage as all energy can be spent inside the victim, while rifles bullets can exit the victim and may not be able to impart all energy. Shot guns which fire pellets can have devastating effect in short range as multiple low-energy pellets can inflict great injuries to the multiple organs, but when same are fired from long range, these pellets usually cause superficial injuries due to low residual energy in these pellets. Bullet characteristics: Bullets are tapered at front end (which exits the barrel first) and are thus lighter at front end and heavier at the back end. When the bullet strikes its target, it ceases spinning, which causes loss of gyroscopic stability. Having lost its directional stability, it is now able to tumble (rotate around its short axis). The bullet tends to tumble through 180 degrees as heavier back end tries to become the leading edge due to more mass and then continue through the target with its proximal end leading. Bullet’s orientation (only orientation of bullet not direction of travel) does not reverse all the time and depends on the length of path it travels inside the victim. The longer the path inside the victim, the greater the chance that the bullet will reverse completely. This tendency to reverse orientation means that if intact bullets are seen on radiographs, frequently they do not point toward their direction of travel, but often point toward their entry wounds. If the bullet is deformed at impact, this tendency to tumble will be modified and may even be eliminated completely. Most bullets are made of lead. Lead being a soft metal can get deformed while inside the barrel of the firing weapon. To prevent this deformity, many high-velocity bullets have a metal casing, usually of copper (other metals also used) surrounding the lead core. If these metal casings completely cover the lead, the bullet is called a fully jacketed bullet. If metal casing only partially covers the lead core, then the bullet is called a semijacketed bullet. The defect in metal casing is usually at the tip of bullet, which partially exposes the soft lead in front. This soft lead tip fragments on impact to increase tissue injury. Hollow-point bullets have an open cavity in their front end, which deforms on impact, generally into a mushroom shape which increases their calibre and increases tissue injury (Fig. 2.13.1.2). Fragmentation: Rifle bullets have very high energy. Sometimes, they can exit the victim so fast that they are unable to transmit maximum wounding energy into the target. Unjacketed bullets and semijacketed bullets break apart into multiple fragments once they strike a target; this phenomenon is called fragmentation. Fragmentation of high-velocity bullets leaves a trail of lead and metal fragments along their path and creates a “lead snowstorm” appearance on radiographs (Fig. 2.13.1.3). These fragments significantly increase the amount of energy deposited inside the victim. Use of unjacketed and semijacketed bullets is prohibited in modern armies, but insurgents routinely use such bullets. Fragments are deposited in a conical area and the apex of cone points towards entry. Deformity induced on impact of hollow point bullets is usually of mushroom shape, which increases their diameter, and as a result, these bullets decelerate faster. Faster deceleration causes most of the kinetic energy of the projectile to be deposited within a smaller volume of the target. These bullets are thus able to deposit all their kinetic energy inside the target increasing the severity of injury. Fully jacketed or nondeforming high-velocity bullets usually leave the target through an exit wound and will still have some kinetic energy left which these bullets were not able to deposit inside the target. Tissue characteristics: After impact bullets cause injury due to two major mechanisms (Fig. 2.13.1.4): Of all the CRT patients suffering from gunshot, blast, missile and splinter injuries undergoing CT scans – fractures account for the maximum number of cases, accounting for approximately half the cases. Of the rest, approximately 10%–15% each are detected to have haemoperitoneum, haemothorax, solid organ injuries and bowel injuries. Radiologist has a substantial role in the evaluation and treatment of the patient with a gunshot wound. During evaluation and imaging of patient with plain films, USG, CT and MRI radiologist should evaluate the following: Imaging Modalities Various imaging protocols exist and are deployed in CRT settings depending on the clinical status of the patient and availability of equipment. CRT patients undergoing medevac are received by military hospitals in dedicated casualty reception areas (CRAs), which are different from the routine casualty. Teams of healthcare personnel are at hand, including surgeons, anaesthetists, nurses and paramedics including radiographers to evaluate and manage casualties, which are often multiple. The radiologist is a key member of this team for eFAST scans. Plain radiographs still retain a primary and important role in combat trauma setting and at most times are the first imaging modality and sometimes the only imaging performed. After initial clinical examination, multiple X-rays of the patient can be taken depending upon the site of the injury/injuries and the condition of the patient. In this setting, radiographs obtained by “portable digital X-ray machines” with their ability to quickly produce high-quality radiographs have drastically improved initial evaluation. These radiographs can easily locate metallic density bullets and splinters and are helpful in identifying ballistic tracks and potential sites of injury. Initial radiological examination can begin with X-ray chest and X-ray abdomen both supine – to quickly point towards a cardiopulmonary injury, fractures including pelvic, spinal or rib fractures – which may then point towards other serious intrathoracic or intraabdominal injuries. Pneumothorax, haemothorax and pneumoperitoneum – all can be quickly diagnosed in this initial setting, and many a times lifesaving procedures such as intercostal drainage tube insertion can be performed during this early evaluation, without shifting patients to OT. Radiographs are of immense help in imaging of extremity injuries (Fig. 2.13.1.5). Their ability to demonstrate fractures, displaced bony fragments and location of metallic fragments, coupled with good clinical examination, can obviate the need for further imaging. In most cases of extremity injury, AP and lateral views of the injured part suffice. Focused assessment by sonography for trauma (FAST) is now routinely used at multiple centres for initial assessment of patients with multiple injuries. Its role is similar in CRT settings. There is vast body of literature on FAST, and it has been recommended in the advanced trauma life support (ATLS) training. In noncombat setting, FAST is generally performed by a trained clinician or surgeon. However, in CRT setting, FAST can be performed by the radiologist to allow the clinician/surgeon in his evaluation and/or resuscitation efforts. While in the casualty reception area, radiologist can also provide valuable preliminary interpretation of initial radiographs. Fast scanning is performed using a portable USG machine and standard convex 3 to 7 MHZ transducer. FAST examination is dedicated to finding free intraperitoneal fluid, which is taken as evidence of haemoperitoneum in trauma setting. Fluid is assessed in four locations namely: The FAST protocol has demonstrated sensitivities between 85% and 96% and specificities exceeding 98% for detecting haemoperitoneum and haemopericardium. In hypotensive trauma patients, it can be done under 5 minutes and sensitivity approaches 100%. Advent of multislice helical CT scanners with subsecond gantry rotation times and their ability to generate high-quality 3D images has revolutionized assessment of patients in CRT setting. Hospitals catering to CRT should ideally have CT scanners in close proximity to the casualty reception area (CRA). CRT patients thus can quickly undergo CT scanning before being shifted to operating theatre. In our hospitals, many a times CT scanning is performed even for seriously wounded after undergoing urgent resuscitation under surgical/anaesthetic care. CT scanning often adds significant additional information or detects unsuspected injuries even when indications for surgery are present. Various protocols are available for imaging patients in CRT setting. Before embarking on whole-body CT scanning, a discussion with treating team can limit the area being imaged and reduce scan and interpretation times. Interpretation of X-rays taken in CRA and scout images obtained in CT can further localize splinters; bone fragments and scan coverage can be altered accordingly (Table 2.13.1.1). Because the hospital is generally aware of arrival of trauma patients, preloaded contrast in the pressure injector saves time. In many situations where time is a factor, noncontrast images can suffice and provide road map for surgical management. For IV access, 18G IV cannula is preferred, and before using IV contrast, it is mandatory to check for the patency of IV access. Administration of oral and rectal contrast increases time and is rarely used. It is best to evolve a dedicated CT protocol tailored for own hospital needs. Injection of IV contrast and scanning of the part should be timed such that there should be simultaneous arterial, pulmonary and solid organ parenchymal enhancement. Delayed images can be obtained in some cases to demonstrate extravasation or active bleeding, pseudoaneurysms and ureteric injuries. CT cystograms using dilute iodinated contrast may be used to detect intra/extraperitoneal bladder injuries. Entry wounds are generally smaller and the exit wounds are larger; however, clinicians in CRA are frequently unable to reliably differentiate entry from exit wounds. Assessment of fractures and distribution, orientation and location of the bone fragments and metallic splinters can be helpful in estimating the direction of projectile travel and thus help in detecting the entry and exit wounds. Some reliable points to establish direction of projectile travel are as follows (Fig. 2.13.1.6): Injuries to thorax contribute a significant number of cases received in combat. Injuries to thoracic structures can occur by blast wave, displaced objects from blast, bullets and splinters from explosives. Chest radiography and CT remain the main modalities to evaluate thoracic trauma. Initial radiographs in CRA diagnose tension pneumothorax, large haemothorax, flail chest and malpositioned medical support tubes. As compared with radiographs, CT identifies 38%–81% additional diagnoses and 20% more extensive pathology. Various injuries suffered in thoracic trauma include ribs, scapular and sternal fractures, costal cartilage injuries (Fig. 2.13.1.7), contusions and laceration to lung parenchyma, mediastinal injuries including injuries to great vessels, pericardial and cardiac injuries. Rib fractures are common injuries and account for majority of injuries in setting of trauma. MDCT with MPR reconstructions remains the most sensitive modality for detecting rib fractures. Displaced rib fractures themselves can cause lung parenchymal injuries or pneumothorax. Fractures of first three ribs signify great force and are associated with injuries to brachial plexus and subclavian vessels. Fractures of the 8th to 12th ribs may be associated with abdominal injuries. Flail chest defined as paradoxical chest wall motion during respiration due to three or more contiguous rib fractures at two or more locations is more common in combat trauma, frequently associated with other thoracic injuries such as pneumohaemothorax, pulmonary contusions and lacerations and generally requires surgical intervention. Isolated sternal fractures and costal cartilage fractures are also noted in patients suffering severe trauma. Pulmonary contusions are most common lung parenchymal injuries. In civilian population, they most commonly occur during deceleration in road traffic accidents. Compression forces of blast injuries or use of body armour which essentially converts penetrating to blunt trauma cause alveolar injury and haemorrhage without disruption, resulting in lung contusion (Fig. 2.13.1.8). Pulmonary contusions on chest radiography appear as ill-defined patchy nonsegmental consolidations in the acute setting. On MDCT, they appear as ill-defined nonsegmental areas of ground-glass opacities or consolidations and do not respect anatomic boundaries such as fissures. Patients may lose consciousness in trauma setting and aspirate which may appear similar on CT, fluid or debris in central airways suggests aspiration. Although delayed appearance of contusion appearing up to 24 hrs later has been described, pulmonary opacities which first appear after 24 hours or several days after trauma should be considered as pneumonitis, aspiration or embolism. Resolution of pulmonary contusions begins at 24–48 h s and is usually complete in 3–10 days. Disruption of lung parenchyma due to compressive, shear or penetrating injuries results in lung lacerations. They manifest on CT as round or oval cavity, which often gets filled with blood or fluid (Fig. 2.13.1.9 and 2.13.1.10). Lacerations may be single or multiple and may be unilocular or multilocular in appearance. They may get filled up with fluid, blood or puss and show air fluid levels. Lacerations heal slowly over several months. Pneumothorax is defined as air within the pleural space. In combat setting, pneumothorax is caused by disruption of pleura by the projectile or due to alveolar rupture caused by increased thoracic pressure or by blunt crushing force or deceleration forces sustained during blast injuries. Diagnosis of pneumothorax is usually made at chest radiography. However, in combat settings where patient is usually supine, 10%–50% of pneumothoraces can be missed on radiographs and are detected only on CT and are referred to as “occult pneumothoraces”. Even small pneumothoraces can be clinically significant because they can enlarge later during mechanical ventilation. In supine patients, air accumulates anteriorly and medially (Fig. 2.13.1.11). Various signs are described to diagnose pneumothorax on a supine radiograph including (1) deep sulcus sign – air outlines the costophrenic angle and lucency of the costophrenic angle projects much inferior to the contralateral costophrenic angle; (2) increased lucency at the base of lung, (3) double diaphragm sign – visualization of both the anterior part and dome of affected diaphragm and (4) increased sharpness or better definition of cardiac outline or mediastinal contour. Blood in pleural space is defined as haemothorax. Blood can accumulate in pleural space arising from injuries to chest wall, pleura, lung tissues or even abdominal organs. Haemothorax is diagnosed on noncontrast CT images by increased density (Av HU 35 to 70) of pleural fluid (Fig. 2.13.1.11). Volume more than 1000 mL of high-density pleural fluid constitutes massive haemothorax. Penetrating transmediastinal injury (TMI) is defined as traumatic injury that traverses the mediastinum and is generally caused by gunshot injuries, splinter injuries from blasts or from stab wounds by knives or other sharp instruments. All patients who have (1) entry and exit wounds on separate sides of thorax and (2) only entry wound to thorax especially close to mediastinum should be suspected to have transmediastinal injury (Fig. 2.13.1.12). Penetrating TMI can injure vital structures such as heart, great vessels and their branches, and these patients are in grave danger due to bleeding or associated complications. In fact, many transmediastinal injuries are fatal (Fig. 2.13.1.13). Trauma to main airways such as trachea and major bronchi is rare in clinical practice because these injuries usually occur with other penetrating mediastinal injuries and are usually fatal. The upper half of trachea is located in lower neck, and its lower half lies in superior mediastinum anteriorly. Carina and proximal main stem bronchi are also located in mediastinum, while lobar and further branches are intrapulmonary. Patients suffering trachea–bronchial injuries present with extensive subcutaneous emphysema, hoarseness and haemoptysis along with tachypnoea. These injuries require skillful airway management by experts. On CT, injuries to trachea are seen with subcutaneous emphysema, pneumomediastinum, focal defect in tracheal wall (which may get occluded by adjacent soft tissues or clot) and communication of tracheal air with mediastinal air (Fig. 2.13.1.14 and 2.13.1.15) Few other signs of tracheal injury relating to intubation are also described such as malpositioned endotracheal tube through the tracheal defect, herniation of endotracheal balloon through the tracheal defect and overdistension of endotracheal balloon (diameter >28 mm). Bronchial injuries manifest as angulated bronchus, bronchial wall defects or bronchial “cutoff”. If bronchial injury occurs distal to mediastinal pleura – tension pneumothorax refractory to chest tube drainage may occur. Signs like “fallen lung” resulting from complete transection of bronchus are rarely seen. Delay in diagnosis of tracheal or bronchial injuries can lead to various complications such as empyema, sepsis, mediastinitis, ventilatory failure and death. Delay in surgery leads to infections, bronchiectasis, tracheal or bronchial stenosis, trachea-esophageal fistula and permanent lung damage from chronic airway obstruction Vascular injuries from penetrating mediastinal trauma generally involve ascending aorta, arch of aorta or its proximal branches. In contrast, blunt trauma from blasts more commonly involves the descending aorta. Many patients with large vessel injury are unstable and do not undergo CT scanning; their imaging may be limited to radiographs and/or urgent USG performed in CRA. Patients who are haemodynamically stable can be taken up for CT angiography, which can reveal a pseudoaneurysm, vascular occlusion, active contrast extravasation, early venous contrast material filling due to arteriovenous fistula or an intimal flap. Injuries to arch vessels are more common on CT angiography because only stable patients undergo imaging (Fig. 2.13.1.16). Bullets and splinters are known to embolize from mediastinum to other parts along blood vessels and bowel loops and also along potential spaces of pleural and peritoneal cavities. Before the introduction of concept of selective nonoperative management (NOM) in the 1960s, there was high negative laparotomy rate for penetrating abdominal injuries. Shaftan in his review of 180 cases of abdominal trauma suggested that in patients with abdominal injury, decision for laparotomy should be based on clinical examination as 34.1% of patients in his review underwent negative laprotomies. Although he gave little importance to then available lab and imaging modalities stating “laboratory studies including roentgenograms were of little value in deciding the need for surgery”, the concept of “observant and expectant” management stayed. This “selective conservative approach” concept got greater emphasis as more and more reviews emphasized better management in select cases by conservative approach, and this approach was firmly established in surgical practice by the 1980s. Since then, due to constant evolution of treatment protocols and practices, there is better decision-making leading to reduction in unnecessary surgeries, while at the same time reducing complications of a missed injury. Although initially conservative approach would not be extended to gunshot wounds due to bleeding and risk of contamination accumulating data suggested feasibility of this approach even for GSW for a “highly select subset of haemodynamically stable adult patients without peritonitis”. CT scanning, diagnostic peritoneal lavage and laparoscopy allowed assessment of intraabdominal injury while avoiding complications of laparotomy. Practice guidelines now recommend routine use of abdominopelvic CT as a diagnostic tool to facilitate initial management decisions in patients selected for NOM. CT is an indispensable tool in predicting the need for laparotomy in patients with penetrating abdominal trauma but still has room for improvement. CT has 98% accuracy in detecting peritoneal penetration. ON CT, peritoneal penetration or violation is said to be present if a wound trajectory passes through the peritoneum and air, haemorrhage, or bullet fragments outline the wound tract, or if there is intraperitoneal free air or fluid or intraperitoneal bullet(s) or displaced bony fragments. Peritoneal penetration is also said to be present if an intraperitoneal organ or mesentery is injured or if there is injury to mesenteric vessels. Although in blunt trauma, pneumoperitoneum denotes hollow viscus injury, in the setting of penetrating or perforating abdominal or torso trauma, pneumoperitoneum only denotes peritoneal violation and does not necessarily means a hollow viscus injury. Free intraperitoneal fluid is sensitive marker for peritoneal penetration and is seen in approximately 85% of cases with intraperitoneal injury. In contrast, pneumoperitoneum is seen only in 35% of cases and even then has got little importance in detecting hollow viscus injury as air can be introduced by projectile entry or from penetration wound. Many patients with solid organ injury are unstable and have clear indications for surgery. However, due to improved resuscitation techniques and relaxed interpretation of haemodynamic stability, many more patients are undergoing imaging even with solid organ injuries. CT grading of organ injury is helpful in prognostication and deciding patients for NOM. The three most common types of parenchymal solid-organ injuries seen at CT are lacerations, haematomas and active extravasation. Lacerations appear as linear hypodensity traversing through the organ. Acute haematomas are seen as nonenhancing hypodense regions (as compared with enhancing normal parenchyma) with attenuation values ranging from 35 to 45 HU. Subcapsular haematomas appear as peripheral crescentic hypodense subcapsular collections, outlining the organ or altering contours of a solid organ. Active haemorrhage is seen as foci isodense or hyperdense to enhanced vessels at CECT, with attenuation values ranging from 85 to 350 HU. Liver is the most frequent organ injured in right upper quadrant penetrating trauma. As described before, lacerations, hematomas, active extravasation and subcapsular collections are the most common injuries encountered along with vascular injuries (Fig. 2.13.1.17 and 2.13.1.18). Violation of hepatic capsule leads to haemoperitoneum, but segment VIII injury can lead to isolated retroperitoneal haematoma surrounding IVC or adjacent adrenal gland. Injuries to retrohepatic IVC and hepatic veins have high mortality. However, most of other hepatic injuries – almost all grade III and half of grade IV hepatic injuries – can be managed by NOM Patients with hepatic injury can develop complications such as internal (communicating with bowel, bronchus, pleural) and external (communicating with skin) biliary fistula. Biliary vascular fistulas may form when there is communication with hepatic artery, portal or hepatic veins and blood may appear as hyperdense (Av HU > 50) material within the biliary system. Biliary pleural fistula may get infected. Liver injuries can be associated with diaphragmatic injuries, which if small may not be repaired due to shielding provided by liver hepatic injury resulting from GSW to back. Splenic injuries in penetrating trauma appear similar to hepatic injuries. There is tendency for delayed haemorrhage. NOM management is of greater value in splenic injuries because of sepsis-related complications in asplenic patients. About 63% pateints with penetrating splenic injuries undergo NOM, but only 25% with grade IV injuries are selected for NOM. There can be associated injuries to diaphragm, splenic vascular pedicle or pancreatic tail. While evaluating for renal injuries, delayed scanning for integrity of ureters and bladder may be added to scanning protocol. A focal ill-defined hypodensity on CECT which shows some enhancement in delayed scans is suggestive of contusion. Irregular linear hypodense region of parenchymal defect extending up to the surface and causing disruption of parenchymal continuity are lacerations. Laceration can be complex with varying width, complex shape and associated with blood clots. Infarcts are wedge-shaped hypodensities on nephrographic phase with no enhancement even on delayed scans. Perinephric haematomas are collections around kidney in perinephric space generally limited by Gerota’s fascia. Subcapsular haematomas appear as crescentic or biconvex area of blood collection along the renal contour, causing renal contour abnormality such as flattening or depression of the underlying renal surface. Complex multiple lacerations leading to disruption and fragmentation of renal tissues which may get devascularized; often associated with functional impairment is termed as a shattered kidney. It is often accompanied with severe haemorrhage, ongoing active bleeding and injuries to pelvicalyceal system, leading to urinary extravasations and collections (Fig. 2.13.1.19 and 2.13.1.20). Up to 40% patients with renal injuries can be managed conservatively with organ preservation rates reaching 75%–100%. Successful NOM has been achieved with grade IV injuries (extending to collecting system or closed vascular injuries of the main renal artery or vein), with nephrectomy reserved only for grade V renal injuries. High-grade renal injuries result in the formation of urinary collection in subcapsular or perinephric space appearing as hypodense collections. Urinary collection can extend to peritoneum and simulate ascites. Ureteric injuries: Ureters are less commonly injured – due to protective effect of the psoas muscles, pelvic bones and adjacent vertebra. When ureteric injuries occur, they are associated with other major injuries and can be missed. Ureteric injuries appear as urine leakage and ureteric fistulas. Small and large bowel are one of the most common organs injured in penetrating abdominal trauma. Patients suspected of having bowel injury from penetrating or blunt abdominal trauma and who are haemodynamically unstable or present with clear clinical evidence of peritonitis go directly to OT. Triple contrast CT with oral, rectal and i.v contrast is recommended for patients who are suspected of having bowel injury but are haemodynamically stable. However, administration of oral and rectal contrast causes delay which can be up to 2–3 hrs, and this delay can be crucial in the setting of penetrating abdominal injuries. Studies have shown no added benefit of giving positive oral or rectal contrast. In this emergency situation where the surgeon is likely to operate if there are positive findings on CT, it would be wiser to keep the patients nil orally. In our centre, we only use a single i.v contrast in such settings and reserve oral or rectal contrast only for equivocal cases or where repeat imaging is required (Fig. 2.13.1.21). Direct and indirect signs have been described as CT findings of bowel injury. Contrast leak, bowel wall defects and wound trajectory extending up to or through a bowel segment are most sensitive and specific signs. Other direct signs include mesenteric stranding and contrast extravasation from injured vessels in close proximity to injured bowel. Indirect signs include bowel wall thickening, interloop fluid and mesenteric hematoma. In the absence of a visible trajectory through bowel loops, these indirect signs lack specificity. Conversely, direct signs are highly specific but rarely encountered. In colonic injuries, “dirty masses” and “dirty stranding” corresponding with faecal collections and debris are seen within ascitic fluid and are suggestive of faecal peritonitis which may be localized or diffuse. Other than contrast leak, almost all other signs can be seen on single contrast study. Contrast leak itself although a highly specific sign is seen in only 15%–29% of cases and cannot be relied for diagnosing bowel injury (Fig. 2.13.1.22 and 2.13.1.23). Pelvic penetrating injury is defined as penetrating wound extending within the confines of pelvis and injuries bladder, pelvic bowel loops, pelvic vessels or other adjacent organs. As so many organs are closely located, a GSW or splinter injury to pelvis can cause injury to multiple organs. Bladder and rectal injuries are most common in this region. As with other regions, haemodynamically unstable patients or patients with peritonitis do not undergo imaging. Suspected bladder injuries are usually investigated using retrograde CT cystography where dilute iodinated contrast is injected into the bladder and leaks detected on CT. Similarly, dilute contrast can be injected into the rectum and sigmoid for imaging of rectosigmoid injuries. GSW through pelvis can be entirely extraperitoneal and post challenges for surgical exploration. If there is no injury to rectum, bladder or prostate surgical exploration is usually avoided. Rectal injury: From the sacral promontory to the anorectal junction, rectum can be divided into three parts. Upper third is covered by peritoneum, middle third is only covered anteriorly and lower third is extraperitoneal. Extraperitoneal rectal injuries are left to heal on their own after diversion colostomy, while intraperitoneal injuries are surgically repaired. Wound trajectory analysis thus becomes important in determining what part of rectum is injured to facilitate treatment decision. Approximately one-third of patients suffering from transpelvic penetrating trauma suffer bladder injury. Rectal and bladder injuries can coexist in about 30%–40% patients. Extraperitoneal bladder ruptures leak into space of Retzius and are generally self-limiting, whereas in intraperitoneal bladder rupture, urine leaks extend intraperitoneally and are treated by surgical repairs. CT cystography reliably distinguishes between the two types or mixed patterns of injures. Wound trajectory should be carefully scrutinized for associated lower ureteric injuries (Fig. 2.13.1.24). In a large epidemiological study for civilian cardiovascular injuries for a period of 30 years, it was revealed that most cardiovascular injuries are due to penetrating trauma. Of the 5760 cardiovascular injuries analyzed, upper and lower limb injuries accounted for about one-third (1102 + 859 – lower limb and upper limb) of all injuries. Peripheral vessels are defined as axillobrachial and branches in the upper extremity and femoropopliteal and branches in the lower extremity. Five different types of vascular injuries have been described namely – intimal injury, wall defect and pseudoaneurysm, transection with haemorrhage and/or thrombosis, A-V fistulas and lastly vascular spasm. Intimal injuries are commonly associated with blunt trauma, while wall defect, transections and A-V fistulas are more common after penetrating trauma. Spasm can occur in both settings. Arterial injury is suspected when clinical or Doppler evaluation shows low volume or absent pulses. Specific signs of such an injury in extremities are (1) external bleeding; (2) a rapidly expanding haematoma; (3) any of the classical signs of arterial occlusion – five “P’s” – pulselessness, pallor, paresthesias, pain, paralysis) and (4) a palpable thrill/audible bruit. Immediate operation on the injured extremity is appropriate in the patient without other life-threatening injuries. Indications for imaging include a comparatively low volume or absent pulses in wrist or ankle and/or API <0.9 in an injured extremity. Imaging can include catheter angiography, CT angiography or CDFI, and the choice is dependent on availability of equipment and expertise of radiologist. CT angiography rapidly acquires the images, performs multiplanar and 3D reconstructions and assesses the adjacent soft tissues and bones. Both axial and reformatted images should be evaluated to assess for vascular injuries. CTA is generally performed due to wide availability of CT scanners and trained radiographers with ability to image entire limbs within seconds. Moreover, CT angiography entails a reduced radiation dose and less adverse effects and require no need of sedation. Poor timing of examination with respect to contrast bolus and motion blur and streak artefacts from adjacent bones or metallic splinters are the only major limitations with CT angiography. Our centre also routinely employs CT angiography as imaging procedure of choice to evaluate arterial injury to the extremities (Fig. 2.13.1.25).
2.13: Injury imaging
Introduction
Ballistics


Epidemiology
Imaging and protocols
Plain X-rays

Focussed assessment by sonography for trauma
CT scan
Evaluation and interpretation of imaging
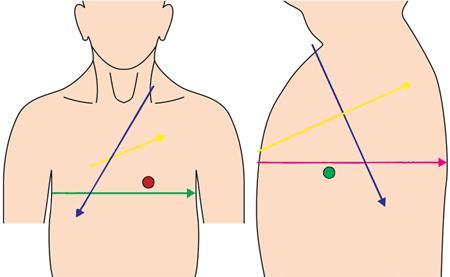
Entry and exit wounds
Systemic injuries
Thoracic trauma
Fractures
Pulmonary contusions
Pulmonary laceration
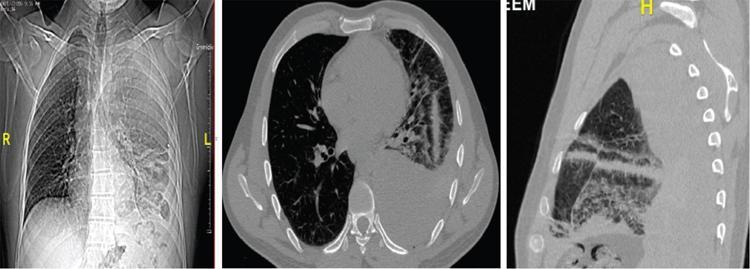
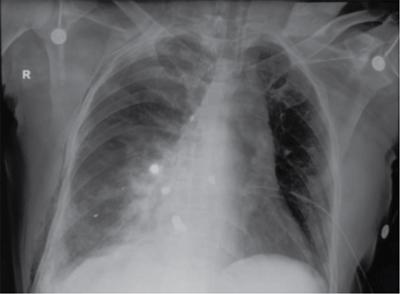
Injuries related to pleura
Pneumothorax.
Haemothorax.
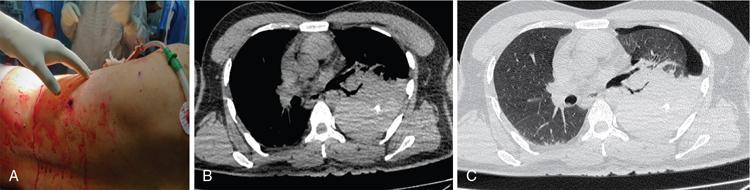
Mediastinal injuries.
Airway injuries.
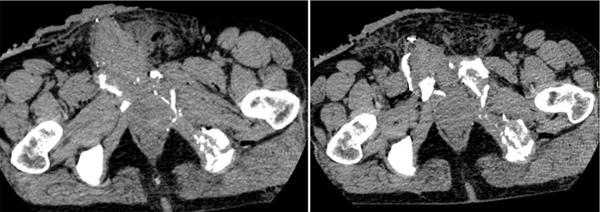
Vascular injuries.
Abdominal trauma
Peritoneal penetration
Solid organ injury
Liver.
Spleen.
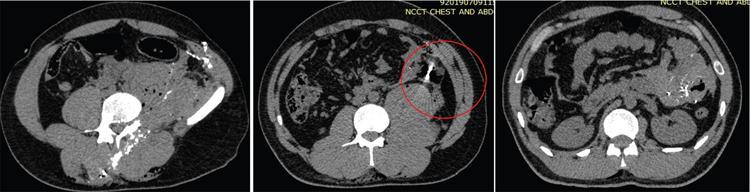
Kidney.
Bowel injuries
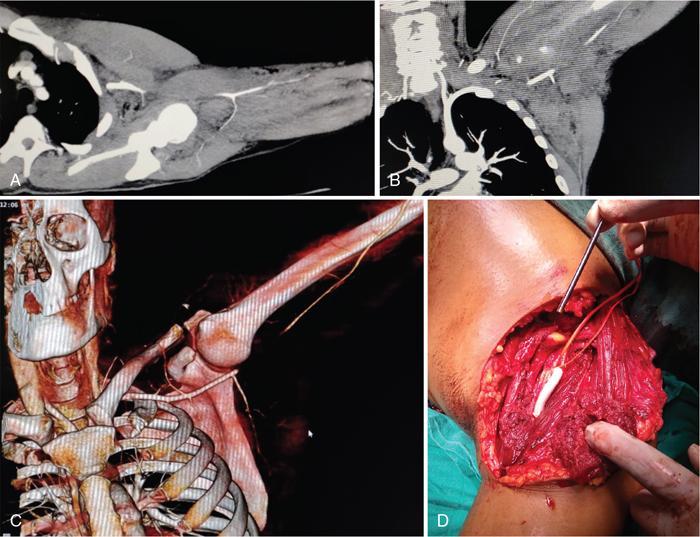
Pelvic injuries
Bladder injury
Peripheral vascular injuries
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree