Chapter 16 Instability
The term ‘instability’ has crept into the literature on low back pain as a diagnostic entity. The implication is that the patient has something wrong biomechanically in their back, and that this is somehow the cause of their pain. Furthermore, since the cause of pain is biomechanical in nature, its treatment should be mechanical. The notion of lumbar instability, however, has become very controversial, as is evident in several reviews1,2 and symposia.3–5 Physicians have abused the term and have applied it clinically without discipline and without due regard to available biomechanical definitions and diagnostic techniques.
Biomechanics
Instability has been defined as a condition of a system in which the application of a small load causes an inordinately large, perhaps catastrophic, displacement.6 This definition conveys the more colloquial sense of something that is about to fall apart or could easily fall apart. Bioengineers have insisted that instability is a mechanical entity and should be treated as such,7 but how biomechanists have portrayed the definition graphically in mathematical terms has evolved over recent years, as more and more embellishments and alternatives have been added.
Stiffness
An early definition simply maintained that instability was loss of stiffness.7 A later elaboration introduced a clinical dimension, to the effect that instability is a
loss of spinal motion segment stiffness such that force application to the structure produces a greater displacement(s) than would be seen in a normal structure, resulting in a painful condition, the potential for progressive deformity, and that places neurologic structures at risk.8
Other engineers have disagreed, insisting that any definition of instability should include the sense of sudden, unpredictable behaviour; that a small load causes a large, perhaps catastrophic, displacement.6 They argue that loss of stiffness may simply describe loose or hypermobile segments that are not at risk of catastrophic collapse.
Neutral zone
a significant decrease in the capacity of the stabilising system of the spine to maintain the intervertebral neutral zones within the physiological limits so that there is no neurological dysfunction, no major deformity, and no incapacitating pain.9
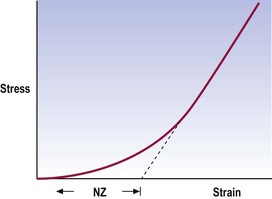
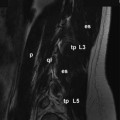
The neutral zone is that part of the range of physiological intervertebral motion, measured from the neutral position, within which the spinal motion is produced with a minimal internal resistance.9 In essence, although not exactly the same mathematically, it is similar to the length of the toe phase of the stress–strain curve that describes the behaviour of the segment (Fig. 16.1).
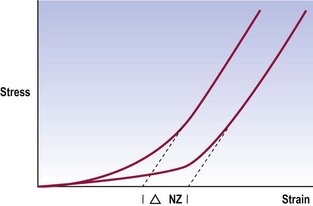
This definition describes joints that are loose but early in range. Their ultimate strength may be normal but early in range they exhibit excessive displacement (Fig. 16.2). This definition captures the sense of excessive displacement; it captures the sense of excessive displacement under minor load but it defies the engineering sense of impending catastrophic failure. However, it does so deliberately and not totally without regard to catastrophe.
Instability factor
Flexion–extension of the lumbar spine is not a singular movement; it involves a combination of rotation and translation (see Ch. 8). Notwithstanding the range of motion, the quality of motion may be defined in terms of the ratio between the amplitude of translation and the amplitude of rotation. For each phase of movement there should be a certain amount of translation accompanied by an appropriate degree of rotation. If this ratio is disturbed, the motion becomes abnormal and the sense of instability may arise. In this regard, the instability would be defined as an inordinate amount of translation for the degree of rotation undergone, or vice versa.
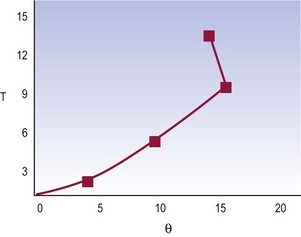
Normal lumbar segments exhibit an essentially uniform ratio of translation to rotation during flexion–extension.10 The overall pattern of movement looks smooth; translation progresses regularly, as does rotation (Fig. 16.3). The ratio between translation and rotation at any phase of movement is the same as the ratio between total translation and total rotation.
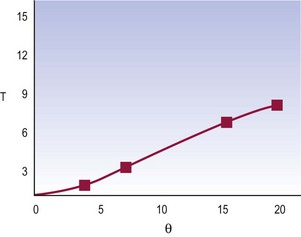
Figure 16.3 A normal movement pattern of a lumbar segment in terms of the ratio between translation and rotation.
(Based on Weiler et al. 1990.10)
It may be defined that instability occurs when, at any time in the movement, there is an aberration to this ratio. The segment suddenly exhibits an inordinate translation for the degree of rotation undergone, or may translate without any rotation (Fig. 16.4).
where (ΔT)i is the range of translation for each phase of motion (i) and (Δθ)i is the range of rotation for each phase.10 In normal spines, the instability factor has a mean value of 25 (mm radian−1) and a standard deviation of 8.7. Values beyond the upper two SD range nominally qualify for instability.
Anatomy
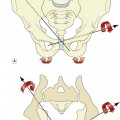
In principle, a spectrum of possibilities arises (Fig. 16.5). Instability may be related to the extent of injury to a segment and the factors that remain trying to stabilise it. At one extreme lies complete dislocation, where no factors maintain the integrity of the segment. At the opposite extreme lies an intact segment that is absolutely stable. Between lies a hierarchy of possibilities.
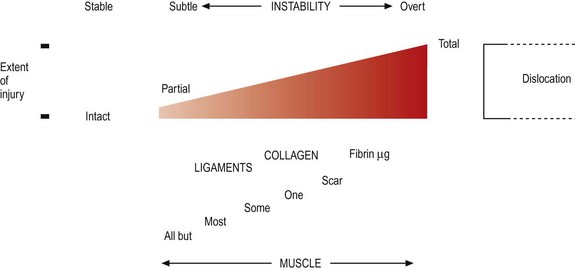
Figure 16.5 The relationship between instability, extent of injury and the factors maintaining stability.
For any degree of stability, the segment requires its stabilising elements: its facets and ligaments (see Chs 3 and 4). The fewer of these that are intact, the more liable the segment is to catastrophic failure; the more that are intact, the more stable the segment becomes.
Numerous studies have been conducted that demonstrate how progressively removing each of the restraining elements progressively disables a lumbar motion segment. Transecting the posterior longitudinal ligament and posterior anulus fibrosus produces hypermobility, even when other elements remain intact.11 Progressively transecting the supraspinous and interspinous ligaments, ligamentum flavum, joint capsules, facets, the posterior longitudinal ligament and the posterior anulus fibrosus leads to progressively greater displacements when a segment is loaded in flexion, with the greatest increase in displacement occurring after transection of the posterior disc.12 Short of transecting the disc, the zygapophysial joints appear to be the major stabilising elements in flexion.13,14
Superimposed on the facets and ligaments are muscles. These contribute to stability in two ways. The lesser mechanism is to pull directly against threatened displacements. In this regard, however, the back muscles are not well oriented to resist anterior or posterior shear or torsion; they run longitudinally and can only resist sagittal rotation (see Ch. 9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree