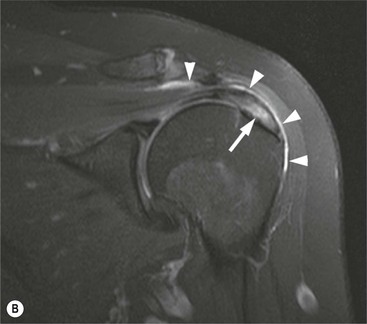
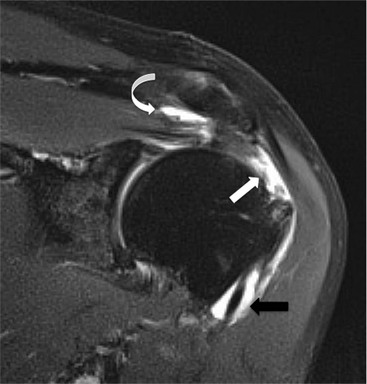
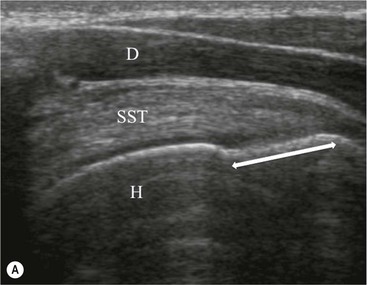
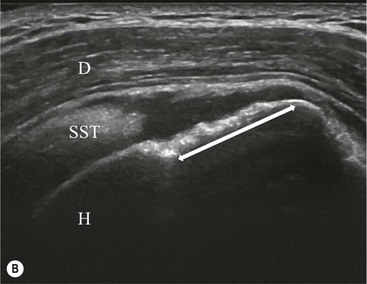
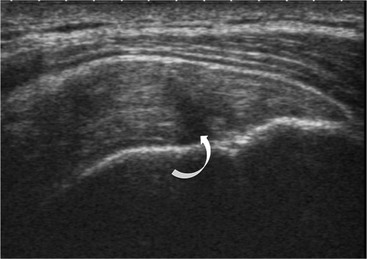
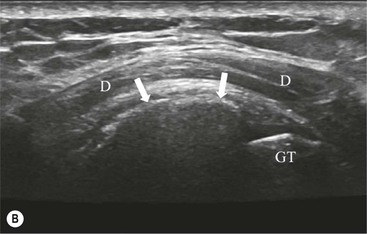
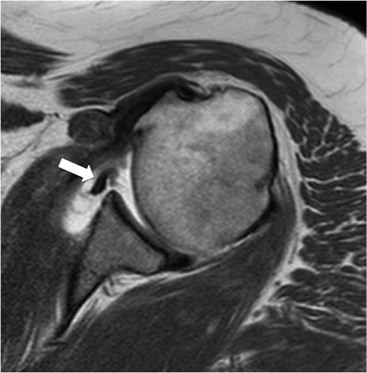
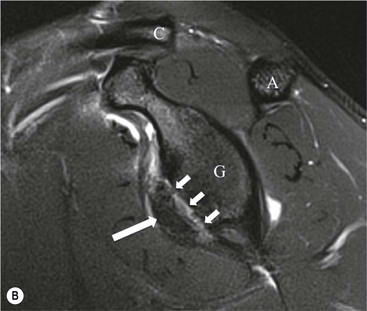
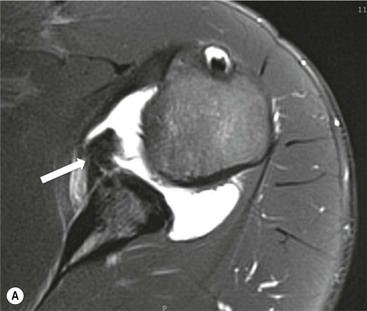
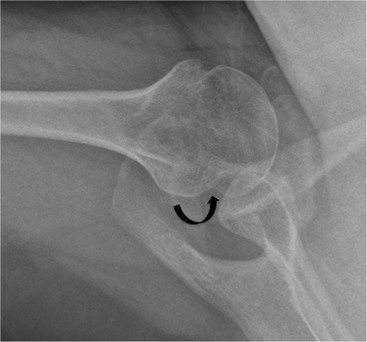
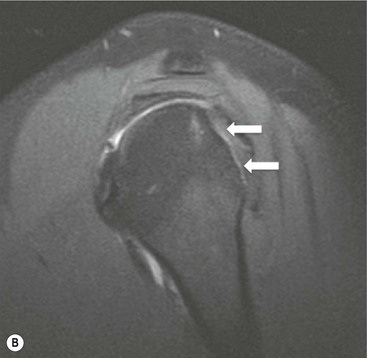
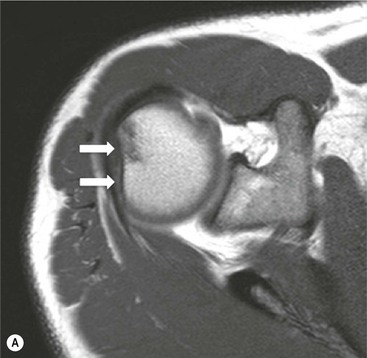
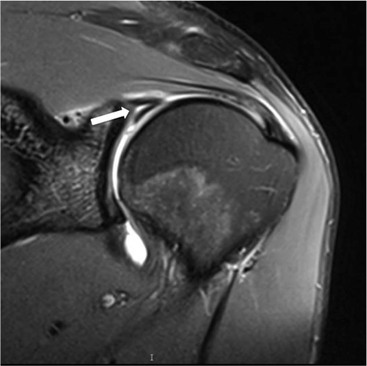
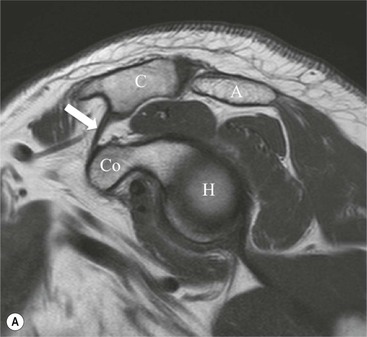
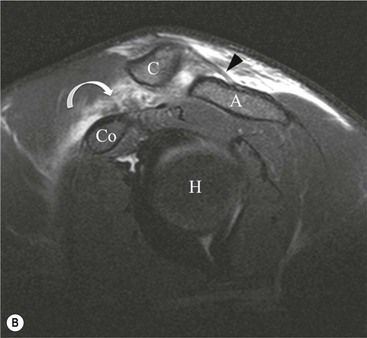
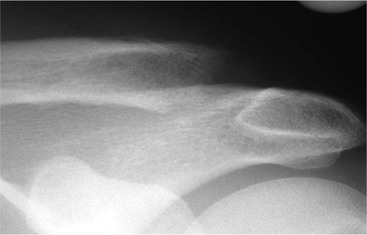
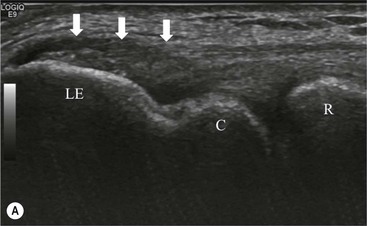
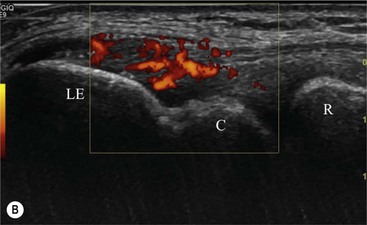
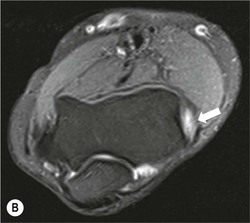
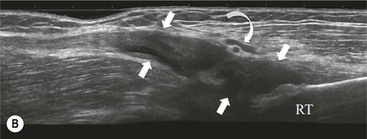
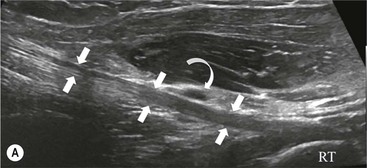
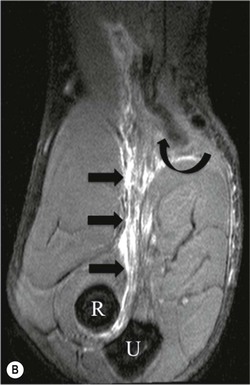
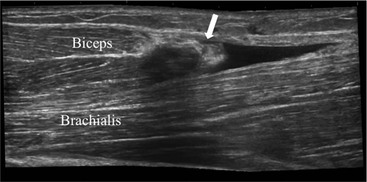
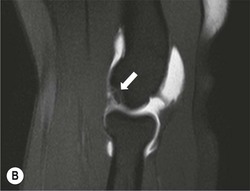
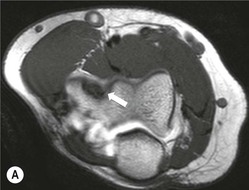
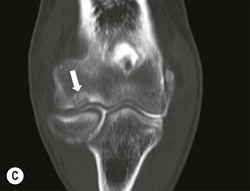
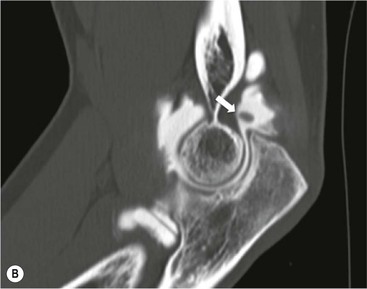
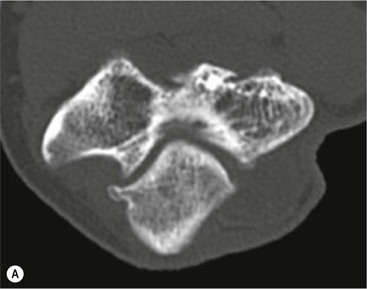
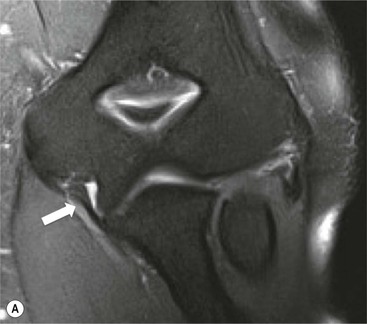
Robert S.D. Campbell, Andrew J. Dunn, Eugene McNally, Ahmed Daghir Magnetic resonance imaging (MRI) and ultrasound now allow the radiologist to undertake detailed examinations of the soft tissues of joints including tendons, ligaments, cartilage and fibrocartilagenous structures such as the menisci. Injuries that previously had to be inferred from patterns of bone injury shown on conventional radiographs can now be assessed in great detail allowing prognosis for conservative management and planning for surgical decision making. While common features exist in terms of the appearance of tendon and ligament abnormalities, the individual biomechanical properties of the different joints and the varying requirements of these joints strongly influence the patterns of injury seen. Broadly, soft-tissue joint injury falls into two patterns: acute injuries such as an acute ligament tear or osteochondral injury and chronic injury. Chronic injury generally occurs as a result of chronic and repetitive microtrauma to the structure concerned. Examples include tendinopathy and impingement syndromes. In this chapter we have used the term ‘tendinopathy’ (sometimes also known as tendinosis) to refer to chronic degenerative change in tendons. This was previously referred to as tendinitis, but this term has fallen out of use as it implies an inflammatory process which is not a feature of the chronic pattern of tendon injury being described. The shoulder is the most mobile joint in the human body. Movement occurs primarily through the gleno-humeral joint, but with a large contribution from the scapulothoracic articulation. The upper limb and scapula articulate with the trunk through the acromioclavicular and sternoclavicular joints. The wide range of movement that can occur at the shoulder is possible because of the shallow cup provided by the glenoid and relatively large humeral head. This configuration has been likened to a golf ball on a golf tee and is inherently unstable. Stability to the glenohumeral joint is provided through the soft tissues of the rotator cuff tendons and ligaments, which are susceptible to injury. The glenoid fossa of the scapula articulates with the head of the humerus to form the glenohumeral joint (GHJ). The glenoid is shallow, pear shaped and anteverted in both the sagittal and axial planes. The fibrocartilaginous labrum runs circumferentially around the glenoid, increasing the overall surface area and contributing to the stability of the joint. The GHJ is surrounded by a number of synovial-lined bursae that communicate with each other and provide lubrication for the motion of the rotator cuff tendons. The subscapularis bursa (SSB) lies anteriorly between the subscapularis tendon and the anterior deltoid muscle. The subacromial bursa (SAB) lies between the supraspinatus and infraspinatus tendons and the undersurface of the acromion, ACJ and lateral end of the clavicle. The subdeltoid bursa (SDB) is continuous with the lateral aspects of the SAB and SSB and continues posteriorly beneath the posterior belly of the deltoid muscle. The rotator cuff muscles and tendons along with the long head of biceps are the dynamic stabilisers of the GHJ. The rotator cuff muscles arise from the scapula, passing laterally, to insert on the proximal humerus. They contribute to abduction as well as internal and external rotation of the humerus. The coracoacromial arch is formed by the coracoid, the acromion and the intervening coracoacromial ligament, under which the supraspinatus tendon (SST) passes. The rotator cuff comprises: • Subscapularis: inserts on lesser tuberosity • Supraspinatus: inserts anterior facet of greater tuberosity • Infraspinatus: inserts middle facet of greater tuberosity • Teres minor: inserts posterior facet of greater tuberosity. The long head of biceps (LHB) tendon arises from the supraglenoid tubercle and superior labrum. The intra-articular component passes between the subscapularis and supraspinatus tendons in a region known as the rotator interval, and enters the bicipital groove on the anterior aspect of the humeral head. The LHB is stabilised within the rotator interval by the biceps pulley comprised of coracohumeral and superior glenohumeral ligaments. The static stabilisers of the GHJ are the glenohumeral (G-H) ligaments which are condensations of the joint capsule. They comprise the superior, middle and inferior glenohumeral ligaments. The IGHL is the most important of the G-H ligaments. It is divided into anterior and posterior components, which act like a hammock to support the humeral head in abduction. The commonest types of internal derangement of the shoulder relate to: The commonest cause of rotator cuff tendon tears is external impingement occurring mostly in patients over the age of 40 years. Acute injuries are uncommon in the younger population, except in athletes. Impingement of the rotator cuff tendons occurs between the humeral head and coracoacromial arch during abduction of the upper arm. Initially there is reversible oedema and haemorrhage in the tendons, which may lead to tendinopathy and eventually failure of the tendon.1 The subacromial space may be reduced by bony abnormalities such as AC joint osteophytes and abnormalities of the shape of the acromion. Secondary impingement may occur through abnormal coordination of the rotator cuff muscles and abnormal scapulothoracic movement. The impingement phenomenon is associated with the development of subacromial bursitis, and acromial bone spur formation. This further limits the subacromial space and aggravates the impingement process.1 Tendinopathy is defined as tendon injury on a cellular level that is most commonly age related and degenerative in nature but may also occur following trauma in younger individuals. The connective tissue that binds and organises the collagen bundles of the tendon undergoes microscopic tearing that leads to activation of inflammatory mediators and disorganised tendon healing. The tendon often thickens and may show features of delamination, mucoid degeneration and eventually partial tearing on imaging.2 Calcific tendinopathy is characterised by intrasubstance deposition of calcium hydroxyapatite crystals of unknown aetiology. The calcific deposits may be asymptomatic but can become painful when they produce focal tendon swelling that may contribute to external impingement. Release of calcium from the tendon into the overlying SAB can produce an acute inflammatory bursal reaction. Rotator cuff tendon tears are defined as partial or full thickness. A partial thickness tear (PTT) involves either the articular surface (commonest) or the bursal surface (less common), but does not extend all the way through the tendon.2 A full thickness tear (FTT) extends from the articular surface to the bursal surface and creates an abnormal communication between the GHJ and SAB. The term full thickness only indicates that the tear extends through the full thickness of the tendon; it does not imply the tear extends from the anterior edge of the tendon to the posterior edge. However, as the tear size increases, the whole tendon may become torn (anterior to posterior) creating a massive tear with medial tendon retraction. The supraspinatus is most commonly affected, but tears may progress to involve both infraspinatus and subscapularis. Tears of the LHB pulley and subscapularis tendon may lead to medial subluxation of the LHB tendon from the bicipital groove. The LHB may also show features on tendinopathy or may eventually rupture. Radiography is useful for demonstrating bony abnormalities of the AC joint and acromion and excluding associated GHJ arthrosis (Fig. 46-1). Marked narrowing of the subacromial space is a specific but insensitive sign of a full thickness rotator cuff tear3 (Fig. 46-2). MRI and ultrasound (US) directly visualise the rotator cuff tendons. Both techniques are capable of diagnosing tendinopathy (Fig. 46-3), and have nearly 100% accuracy rates for FTTs of the rotator cuff.4 MR arthrography is not usually indicated for primary rotator cuff disease. The most important features to describe that help determine management include the following: • presence of associated rotator cuff muscle atrophy • dislocation or rupture of the LHB tendon • bony abnormalities of the coracoacromial arch The primary sign of a rotator cuff FTT is a focal deficiency of the tendon (Figs. 46-4 and 46-5). This nearly always occurs at the tendon insertion on the tuberosity. The margins of the tear are best delineated when there is fluid within the tendon defect. Secondary signs of an FTT include the presence of fluid in both the GHJ and SAB, and flattening or concavity of the subacromial fat plane. PTTs are less reliably demonstrated by both MRI and US, and it may be difficult to differentiate tendinopathy from partial tears. Focal clefts, tears, or tendon thinning affecting the articular margin of the footprint of the tuberosity are most common (Figs. 46-6 and 46-7). Tendon thickening is not always present. It is important not to mistake magic angle phenomenon on short TE MR sequences or anisotropy on US as evidence of tendinopathy.2 Calcific tendinopathy can be visualised on radiographs as discrete amorphous deposits of calcium density. On US they are echogenic and may or may not cast acoustic shadowing (Fig. 46-8). Small deposits of calcium may be difficult to detect on MRI as both the calcification and surrounding tendon are of low SI. The GHJ is an inherently unstable joint. Injury or abnormality of the static stabilisers renders the joint susceptible to recurrent dislocation, and further injury. Chronic GHJ instability may lead to secondary arthrosis if untreated. Imaging is used to document the extent of internal derangement in order to determine the therapeutic options.5 Instability of the GHJ may be dependent on three factors, referred to as the Bayley triangle: A combination of these factors may be present in any one patient, but trauma is the commonest cause of instability. Anteroinferior dislocation is the commonest presentation. Posterior dislocation is frequently encountered following epileptic seizures. Inferior dislocation is rare. Radiographs are the primary imaging technique to confirm GHJ dislocation and establish joint congruity following reduction. Anteroposterior and axial views or a modified caudal angled axial are most appropriate. MRI, MR arthrography or CT arthrography are used in the non-acute setting to assess the static stabilisers.6 Anterior GHJ dislocation causes tearing and detachment of the anteroinferior glenoid labrum, known as a Bankart lesion. The location of the labral tear is described according to clockface terminology: 12 o’clock represents the biceps anchor, and 3 o’clock is anterior at the equator of the glenoid. Fluid signal intensity or contrast medium extending between the glenoid and labrum is the primary sign of a labral tear (Fig. 46-9). The labrum may become displaced, and it is important to assess the position of the labrum with respect to the face of the glenoid. More severe injury may be associated with a bony injury of the glenoid rim, usually called a bony Bankart lesion (Fig. 46-10). Non-enhanced CT may occasionally be preferred to assess the size of the bony defect of the glenoid. There is usually associated impaction injury on the posterosuperior aspect of the humeral head called a Hill–Sachs defect (Figs. 46-11 and 46-12). In posterior dislocation the location of labral and humeral injury is opposite to anterior dislocation, and are termed reverse Bankart lesions and reverse Hill–Sachs defects. Injury to the joint capsule and glenohumeral ligaments is common. The anterior band of IGHL is the most important joint stabiliser. It may be torn at the humeral insertion or less commonly from its origin on the glenoid. Imaging with the arm in abduction and external rotation (ABER imaging) is sometimes used to assess the integrity of the ligament, to identify the degree of labral displacement and loss of joint congruity.5 The most important features to describe that help determine management include: Tears of the superior labrum and biceps anchor are commonly encountered injuries in overhead throwing athletes. Abnormal traction on the biceps anchor and superior labrum results in tears that usually extend posteriorly. They are often referred to as superior labral tears anterior to posterior (SLAP tears).7 MRI, MR arthrography or CT arthrography may assess the glenoid labrum. Contrast medium or fluid signal intensity extending into the substance of the labrum or through the chondro-labral junction is the primary sign of a SLAP tear (Fig. 46-13). Tears may be localised to the posterosuperior labrum, or may be more extensive. There may be tear extension into the LHB tendon. There are many grades of SLAP tears described but the extent of the tear and the structures involved are the most important features.8 The most important features to describe that help determine management include: The AC joint is a synovial plane joint. All the forces of glenohumeral and scapulothoracic movements are transmitted to the trunk through the ACJ and sternoclavicular joint. Osteoathritis (OA) of the ACJ is common and the associated capsular thickening and osteophyte formation is a contributor to external impingement of the shoulder. The ACJ has strong capsular ligaments, and is also stabilised by the coracoclavicular (C-C) ligaments. Traumatic disruption and dislocation of the joint is described by the Rockwood classification: Grade I: undisplaced injury with sprain of acromio-clavicular ligaments. Grade II: ACJ widening with <50% superior displacement of lateral clavicle. Grade III: >100% superior displacement of lateral clavicle. Grade III and IV injuries are associated with disruption of the C-C ligaments and above are treated surgically. Grade I and II injuries usually resolve spontaneously. However, some patients may present with persistent pain and instability. Ligament reconstruction may be required in the athletic population.9 Weight-bearing radiographs may demonstrate abnormal joint widening, and the C-C ligaments can be visualised directly by MRI (Fig. 46-14). Post-traumatic osteolysis of the lateral clavicle occurs in approximately 6% of ACJ disruptions and may also be seen with repetitive ACJ microtrauma such as weight-lifting (Fig. 46-15). The sternoclavicular joint (SCJ) is a synovial saddle joint, with a cartilaginous articular disc. It has limited movement, but like the AC joint transmits the forces of shoulder movement to the trunk. It is very prone to osteoarthritis, which may be associated with chronic anterior subluxation. Radiographic evaluation of the SC joints may be difficult but CT or MRI readily demonstrate the features of arthrosis.10 Traumatic subluxation and dislocation usually occurs anteriorly. Posterior dislocation is a rare but important injury, as the displaced medial clavicle may be associated with vascular injury in the superior mediastinum.11 The elbow is a complex synovial hinge joint. It comprises the ulnotrochlear and radiocapitellar articulations which allow flexion and extension of the elbow. The proximal radioulnar joint (in conjuction with the distal radioulnar joint) enables pronation and supination of the forearm by rotation of the radius around the ulna.12 The primary flexors are biceps brachii, brachialis and brachoradialis. Triceps is the main extensor. Supination of the forearm occurs through the action of biceps and supinator. Pronation is by pronator teres, and pronator quadratus (at the wrist). The common tendon for wrist and hand extension arises from the lateral humeral epicondyle, and the common flexor tendon from the medial epicondyle. The joint is stabilised by the ulnar collateral and radial collateral ligaments. The radial collateral complex includes the annular ligament which supports the radial head. Insertional tendinopathy around the elbow joint most commonly affects: The triceps and other tendons are rarely involved. Tendinopathy of the common extensor and flexor tendons presents with localised pain over the distal humeral epicondyles. It is often a clinical diagnosis, although imaging may be performed in refractory cases to confirm the diagnosis and exclude a tear. Ultrasound is frequently used to guide injection therapy. The affected tendon is thickened and hyporeflective on US, with neovascularisation on Doppler imaging (Fig. 46-16). High SI is demonstrated on fluid-sensitive MRI sequences (Fig. 46-17). Tendon tears are demonstrated as focal areas of deficiency.13 In chronic cases, new bone formation may be seen on radiographs at the tendon enthesis. Calcific tendinopathy is much less common than in the rotator cuff of the shoulder. The distal biceps tendon inserts on the tuberosity of the proximal radius. It does not have a tendon sheath, but surrounding connective tissue is known as a paratenon. It is surrounded near the insertion by the bicipitoradial bursa. Distal biceps tears are often clinically unrecognised, but may be amenable to surgery if diagnosed early. In the early stages the tendon is thickened and there may be an effusion in the bicipitoradial bursa (Fig. 46-18). In complete rupture the tendon retracts proximally. MRI and US may be used to confirm the diagnosis and locate the tendon end (Figs. 46-19 and 46-20). The capitellum is the third most commonly affected site in osteochondritis dissecans (after the knee and ankle). It commonly affects teenagers and young adults. A focal osteochondral fragment or defect may be visualised on radiographs. Cross-sectional imaging with MRI, MR arthrography or CT arthrography is used to detect radiographically occult lesions and for grading osteochondral lesions (Fig. 46-21). The osteochondral fragment may remain in situ or lie remotely within the elbow joint. Fluid SI at the base of the osteochondral lesion on MRI, or contrast medium tracking around the fragment on arthrographic images, is a sign of an unstable lesion. Integrity of the overlying articular cartilage is a good sign of stability. Reports should include: • size and location of osteochondral defect; • stability of the lesion and integrity of overlying cartilage; and Intra-articular bodies are also frequently encountered in OA of the elbow. They may be calcified, but non-calcified chondral bodies may also occur. CT is often utilised to assess the size and location of osteophytes before surgery, as well as identify small loose bodies. Chondral bodies are not visualised on radiographs or conventional CT. In some cases pre- and post-angiography CT may be performed (Fig. 46-22). Conventional MRI is less sensitive for detection of small intra-articular bodies. The collateral ligaments of the elbow may be torn as the result of an elbow dislocation, and may require surgical repair. A coronoid process fracture is a sign of an unrecognised elbow dislocation. Chronic tears of the ulnar collateral ligament are infrequently encountered in some throwing sports and in weightlifters. In acute injuries MRI shows the presence of soft-tissue oedema and haemorrhage around the affected ligament. MR arthrography may be preferred for diagnosis of chronic tears. Acute ulnar collateral ligament (UCL) tears often occur at the proximal origin on the medial humeral epicondyle (Fig. 46-23). In chronic tears the defect is usually at the insertion on the sublime tubercle of the ulna.14 The wrist is a synovial joint, formed from the articulations between the radius and ulna, the eight carpal bones and the metacarpal bones. The distal radioulnar joint allows supination and pronation of the forearm. The mechanics of the wrist are complex, but movement occurs primarily through the proximal carpal row, comprising the scaphoid, lunate and triquetrum. This acts as a bridge between the forearm bones and the distal carpal row, which is relatively rigid. The proximal carpal row is referred to as the intercalated segment, and the lunate acts as the keystone. Stability between the segments of the proximal row is maintained by the intrinsic scapholunate and lunotriquetral ligaments. Stability between the radius and ulna, the proximal and distal carpal rows is maintained by multiple dorsal and volar extrinsic ligaments. Carpal alignment is assessed on PA radiographs, by identifying continuity of the articular surfaces of the carpal bones (known as the arcs of Gilula). The first carpometacarpal joint between the trapezium and first metacarpal is more mobile than the other CMC joints to allow for the greater range of movements of the thumb. It has a separate synovial compartment. The distal radioulnar joint and ulnocarpal joint are stabilised by the triangular fibrocartilage (TFC) complex. The TFC is a cartilaginous disc that arises from the ulnar border of the distal radius and attaches to the fovea of the ulnar styloid. Its margins blend with the dorsal and volar radioulnar ligaments, and the extensor carpi ulnaris (ECU) tendon sheath.
Internal Derangements of Joints
Upper and Lower Limbs
Introduction
The Shoulder
Rotator Cuff Disease
GHJ Instability
Superior Labral Tears
The Acromioclavicular Joint
The Sternoclavicular Joint
The Elbow
Tendons
Bone and Cartilage
Ligaments
Hand and Wrist
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Internal Derangements of Joints
Chapter 46