CHAPTER 35 Interpretation and Reporting in Obstructive Coronary Disease
TECHNIQUES
Indications
Potential indications for coronary CTA are many and continue to evolve. Recently, the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, the American College of Radiology, and others have published a joint review on the appropriateness of cardiac CTA.1 This report scored the appropriateness of cardiac CTA in several clinical applications on a scale from 1 to 9 based on the available literature. The information and experience available with cardiac CTA at this time are not robust enough to support categorical recommendations and guidelines. This is so because the technology continues to change rapidly, there are not enough prospective studies on different groups of patients, and there are no outcome studies on the prognostic value of cardiac CTA. Therefore, the appropriateness criteria are not guidelines but rather temporary recommendations until official guidelines are published.
Pitfalls and Solutions
In CT, the term artifact applies to any systematic discrepancy between the CT numbers in the reconstructed image and the true attenuation coefficients of the object. CT images are inherently prone to artifacts because the image is reconstructed from multiple independent detector measurements. The reconstruction algorithm assumes that all these measurements are consistent, so any error of measurement will usually be reflected as an error in the reconstructed image.2,3
Artifacts can seriously degrade the quality of CT images, sometimes to the point of making them diagnostically unusable. Furthermore, accuracy of cardiac CTA for detection of stenoses depends highly on image artifacts,3 which are a major cause of false-positive and false-negative interpretations.
To optimize image quality, it is necessary to understand why artifacts occur and how they can be prevented (Table 35-1). CT artifacts originate from a range of sources. Physics-based artifacts result from the physical processes involved in the acquisition of CT data. Patient-based artifacts are caused by such factors as movement of the patient or the presence of metallic materials inside or on the patient.
Beam Hardening
An x-ray beam is composed of individual photons with a range of energies. As the beam passes through the patient, it becomes “harder”; its mean energy increases because the lower energy photons are absorbed. As a result of this effect, dark bands or streaks can appear on the image adjacent to dense objects such as calcifications, dense contrast material, or metallic clips (Fig. 35-1). Beam hardening can be minimized by filtration.
Partial Volume (Blooming)
CT numbers are based on attenuation coefficients for a voxel of tissue. If the voxel contains more than one tissue type, the CT number will be based on an average of the different tissues involved. For example, a dense calcified plaque or stent, lying off-center, may appear larger than it actually is in the reconstructed image because of partial volume effects and create an exaggerated luminal narrowing (Fig. 35-2). This problem is magnified if there are also motion artifacts (Fig. 35-3).
Metallic Materials (Streaks)
The presence of metal objects (such as pacemakers, electrodes, stents, and surgical clips) in the scan field can generate severe streak artifacts (Figs. 35-4 and 35-5). They occur because the metal object absorbs the radiation, resulting in incomplete projection profiles.
Patient Motion (Blurring)
Motion of the patient can cause misregistration artifacts, which usually appear as shading or streaking in the reconstructed image (Fig. 35-6). Steps can be taken to prevent voluntary motion (due to movement or breathing during the scan), but some involuntary motion may be unavoidable. Prescan instructions about the expected breath-hold are critical to minimize motion artifacts as well as to decrease scan time. Involuntary motion artifacts may be caused by heart rate irregularities during the scan and will appear as blurring or stair-step artifacts. Looking for a motion-free phase can sometimes help improve visualization of the coronary arteries (Fig. 35-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


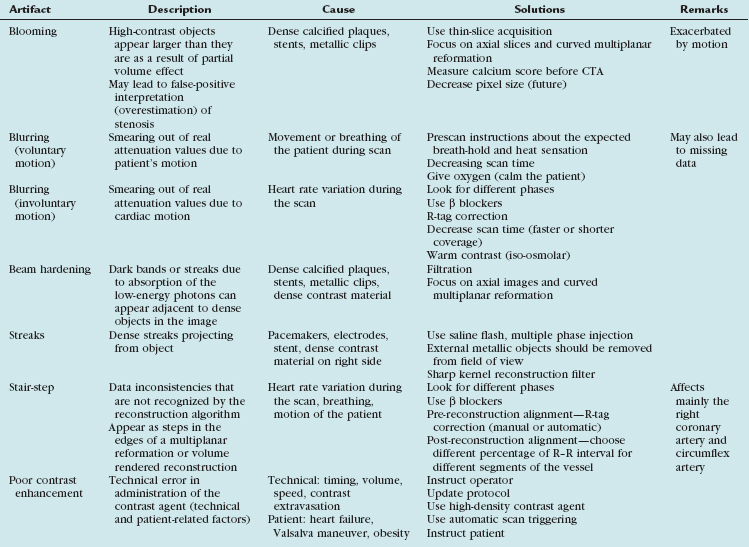
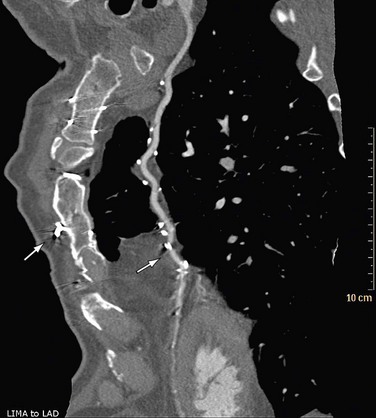
 FIGURE 35-1
FIGURE 35-1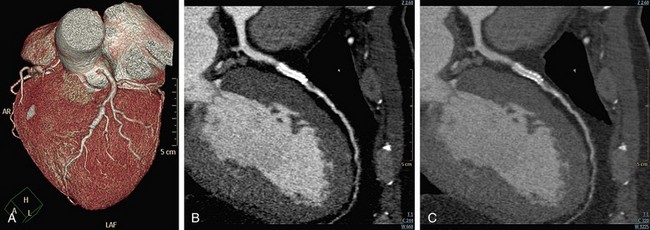
 FIGURE 35-2
FIGURE 35-2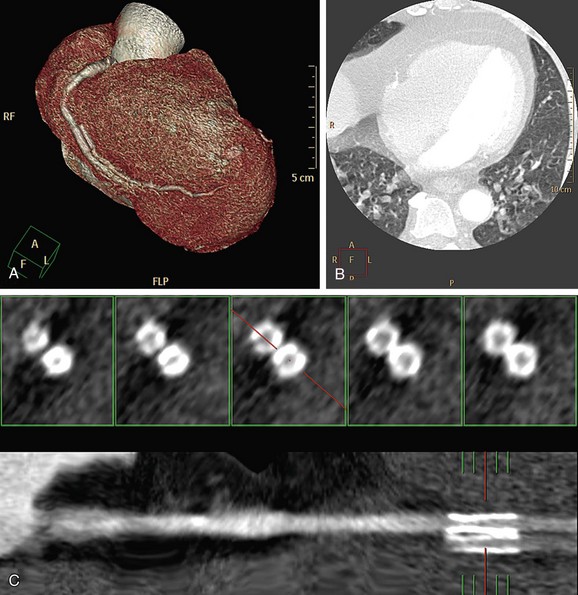
 FIGURE 35-3
FIGURE 35-3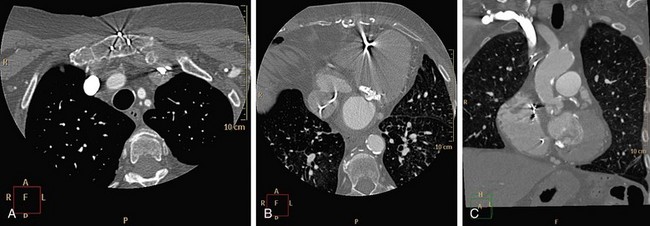
 FIGURE 35-4
FIGURE 35-4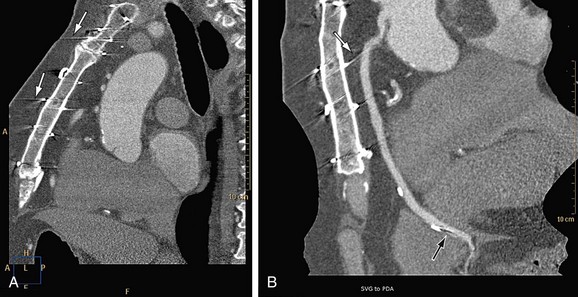
 FIGURE 35-5
FIGURE 35-5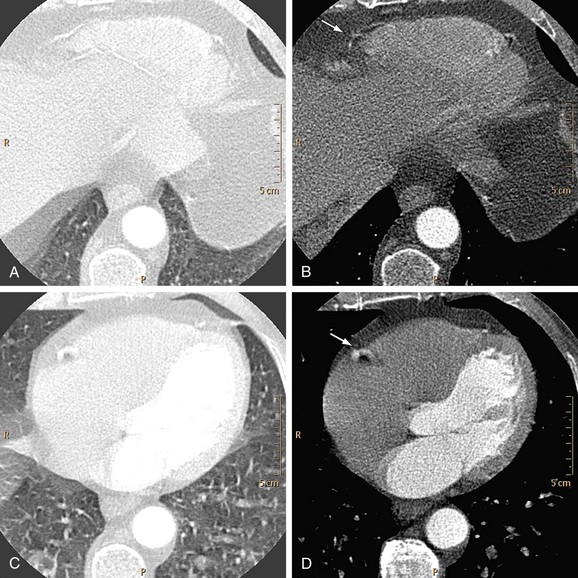
 FIGURE 35-6
FIGURE 35-6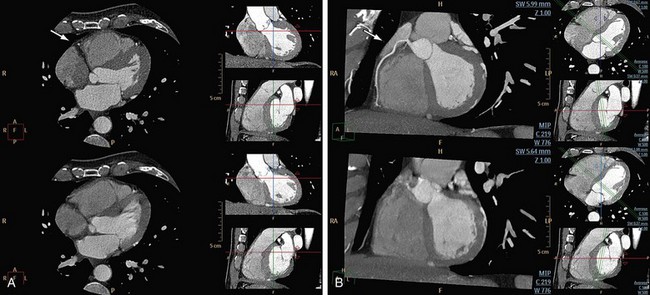
 FIGURE 35-7
FIGURE 35-7