Intracranial Infections
Bradley R. Foerster
Myria Petrou
Etiology and presentation.
Leptomeningeal inflammation most often occurs after hematogenous spread of bacteria. In the early phase, the pia and arachnoid matter become congested and hyperemic. Later, the leptomeninges becomes thickened and an exudate can cover the brain particularly in the dependent regions such as the basal cisterns. Inflammatory changes can interfere with cerebrospinal fluid (CSF) drainage, potentially causing hydrocephalus. Infants can have a varied clinical picture including mental status changes, fever, irritability, and vomiting. Adults have a more typical presentation with symptoms including fever, headache, meningismus, and photophobia. Bacterial meningitis is a clinical diagnosis based on history and physical examination and confirmed by CSF laboratory testing. Imaging is important to exclude a mass lesion, other potential diagnoses, and to look for potential complications of meningitis.
Differential diagnosis
includes migraine, subarachnoid hemorrhage, brain abscess, subdural empyema, and viral encephalitis.
Complications
Hydrocephalus is the most common complication and results from disruption of CSF resorption or obstruction.
Spread of infection may cause brain abscess and subdural empyema (see subsequent text).
Infarction from vasculitis, arterial ischemia, or venous thrombosis.
Ventriculitis is a possible complication of meningitis. Ventricles are enlarged with surrounding high T2 signal and subependymal enhancement.
Permanent neurologic deficits and death (in 10 to 30% of patients with bacterial meningitis).
Cerebrospinal Fluid Evaluation
Noncontrast head computed tomography (CT) is usually performed before lumbar puncture (LP) to exclude a mass lesion despite lack of evidence to support the routine use of this practice. Obtaining the head CT should not delay the LP and initiation of antibiotic therapy. CSF is sent for protein and glucose concentrations, cell count, Gram stain, and culture.
CSF findings in different types of infection are given in Table 8-1.
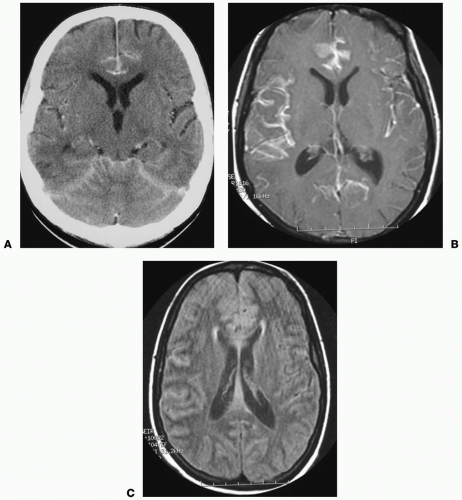
Possible Findings (Fig. 8-1)
Normal imaging is the most common finding in early meningitis.
Enhancement of the leptomeninges is better seen on magnetic resonance (MR) than on CT.
Enlargement of CSF spaces, particularly in the basal cisterns and interhemispheric fissure.
High intensity of subarachnoid fluid on fluid attenuation inversion recovery (FLAIR) imaging.
Communicating hydrocephalus with enlargement of temporal horns and effacement of basal cisterns.
Brain infarct.
Cerebral edema/inflammation (cerebritis).
| |||||||||||||||||||||||||
Pitfalls
Diffuse pachymeningeal enhancement can occur with intracranial hypotension following LP.
Etiology and presentation.
Cerebral abscesses are most commonly caused by hematogenous dissemination. Brain abscesses can be divided into four stages: (1) early cerebritis (1 to 3 days), (2) late cerebritis (4 to 9 days), (3) early capsule formation (10 to 13 days), and (4) late capsule formation (>13 days). Magnetic resonance imaging (MRI) is the study of choice for diagnosis of brain abscesses.
Possible Findings
Noncontrast CT
Low-density abnormalities with mass effect and surrounding edema.
Contrast-enhanced CT
Uniform ring enhancement is virtually always present in later phases.
MRI
Early phase can have patchy enhancement, low T1 signal, and high T2 signal.
Later phase is characterized by development of ring enhancement.
The abscess typically has low T1 and high T2 signal with surrounding edema, which has high T2 signal.
Restricted diffusion (bright signal on diffusion weighted imaging [DWI] and low signal on apparent diffusion coefficient [ADC] map) helps differentiate abscesses from necrotic neoplasms (usually not restricted), however not all abscesses follow this rule.
Pitfalls
Ring enhancement is nonspecific. Differential diagnosis includes neoplasm, tumefactive multiple sclerosis, lymphoma, hematoma, and infarct. Thickness, irregularity, and nodularity of the enhancing ring suggest tumor (majority of cases) or fungus.
Etiology and presentation.
Herpes simplex virus (HSV) is the most common cause of fatal endemic encephalitis. Both type 1 and type 2 viruses produce encephalitis. Type 1 affects children and adults, and presents with viral prodrome, seizures, fever, headache, and mental status changes. Type 2 infection occurs during the neonatal period. Mortality due to HSV encephalitis is reduced from approximately 75% to 25% with early diagnosis and prompt acyclovir therapy.