Pulmonary Embolism
Krishna Juluru
Epidemiology.
Although pulmonary embolism (PE) has been widely studied for many decades, its incidence, mortality, diagnosis, and treatment are still the subject of investigation. Incidence has been estimated to be 0.2 to 0.6 per 1,000 per year. Mortality rates as high as 30% have been reported in the older literature, although these studies are limited by use of clinical criteria for diagnosis of PE and by inclusion of patients with multiple comorbidities which may have independently contributed to death. The mortality in asymptomatic patients with PE and a low incidence of comorbid disease has been reported to be as low as 2.4%. Studies have shown that mild, untreated disease may have a low recurrence rate, arguing that clot burden should be a factor in determining management.
Risk Factors.
Most PE arise from clots within the venous circulation, and deep venous thrombosis (DVT) of the lower extremities is most common. Trauma and immobilization, cancer, and hypercoagulability comprise three broad categories of risk factors for DVT, with the latter two being most significant. The risk of recurrent thromboembolism is as high as 3.5 times greater in cancer populations than in those without cancer. Hypercoagulable states can exist due to genetic predisposition such as factor V Leiden mutation, prothrombin gene mutations, and deficiencies in protein S, protein C, and antithrombin III. Recently, blood types A and AB have been cited as additional risk factors. Certain medications, such as oral contraceptives, also increase risk.
Symptoms and Signs.
Clinical diagnosis of PE is unreliable. The most common symptom, dyspnea, is seen in only 73% of patients with angiographically proven PE. Other symptoms include pleuritic chest pain (66%), cough (37%), leg swelling (28%), leg pain (26%), and hemoptysis (15%). Angina, caused by right ventricular ischemia, and syncope have also been reported. Of note, patients with radiographic diagnosis of PE can be asymptomatic. The most common physical finding is tachypnea, seen in 70% of patients. Other findings include lung crackles on auscultation (55%), tachycardia (30%), and increased pulmonic component of the second heart sound (23%). The presence or absence of symptoms or signs should not exclusively influence a decision to proceed with further testing to diagnose PE.
Differential Diagnosis.
Owing to the lack of specific clinical findings, the differential diagnosis of PE is broad. Alternate considerations include pneumonia, congestive heart failure, acute myocardial infarction, exacerbation of chronic lung disease, aortic injury, and musculoskeletal inflammation/injury.
Indications.
Chest radiography is a low-cost and low-radiation technique that, in most cases, is an appropriate start in the assessment of patients with chest symptoms. It can help identify other etiologies of the patient’s symptoms and is used in conjunction with nuclear ventilation and perfusion imaging (ÿV/ÿQ) results, but it alone cannot help to include or exclude the diagnosis of PE.
Possible Findings.
Radiographic signs of PE include prominent central artery (Fleischner sign), enlarged hilum, enlarged mediastinum, pulmonary edema, oligemia (Westermark sign), pleural-based areas of increased opacity (Hamptons hump), pleural effusion, and elevated hemidiaphragm. The highest sensitivity of any finding is 36% for pleural effusion. The highest specificity of any finding is 92% for oligemia. Entities that can be identified other than PE include pneumonia, pneumothorax, pneumomediastinum, heart failure, pleural effusion, lung mass, and fractures.
Indications.
Computed tomographic pulmonary angiography (CTPA) performed on a multidetector computed tomographic (CT) scanner (four or more detectors) is the modality of choice for diagnosis of PE. Advantages include the ability to directly visualize pulmonary vessels and to diagnose diseases of the chest other than PE that may be contributing to the patient’s symptoms. Renal insufficiency and allergy to contrast dye are the only major contraindications. Some patient cooperation in breath-hold is required. Using clinical outcome reference standards, the negative predictive value of computed tomographic angiography (CTA) ranges from 94-100% on scanners with less than four detectors. In comparison, studies performed on multidetector computed tomographic (MDCT) scanners demonstrate similar negative predictive values, but with reduced rates of respiratory and motion artifacts.
Protocol.
CTA is performed following intravenous administration of 100-150 mL nonionic iodinated contrast agent at a rate of 3-4 mL/second. Power injection is considered unsafe through central lines, and therefore only peripheral venous access is used. The scan is performed from the lung apices to bases following live bolus tracking or a 23- to 28-second delay. Use thinnest possible (at most 1-2 mm) slice thickness. Multiplanar reconstruction of the pulmonary arteries from source data can be helpful in visualization of the pulmonary vessels.
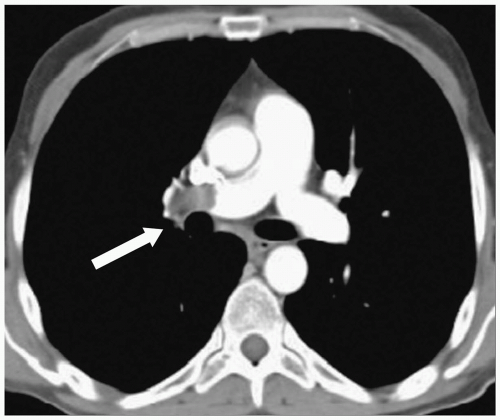
Possible Findings (Fig. 20-1)
Well-defined filling defects in a pulmonary artery seen on multiple sections are characteristic of PE (Fig. 20-1). Adjust the windows to make sure the pulmonary arteries
are not too bright to detect subtle PE. These should be distinguished from flow-related artifacts and from masses, most notably in the mediastinum, that may be causing vascular compression.
Careful inspection of the scan may reveal other symptom-related findings such as pleural/pericardial effusion, pulmonary infiltrates, pulmonary masses, and fractures.
Indications.
Nuclear ÿ V/ ÿ Q imaging scan can be used as a substitute for CTA, particularly in patients with renal insufficiency in whom iodinated intravenous contrast cannot be administered. Results are reported as normal, low, intermediate, or high probability. The sensitivity of a normal ÿ V/ ÿ Q scan is 98%, and the specificity of a high probability scan is 97%. A significant number of scans (39% in the Prospective Investigation of Pulmonary Embolism Diagnosis [PIOPED] study) fall into an intermediate probability category, limiting the strength of this imaging modality. Abnormalities on chest radiographs (e.g., infiltrates, masses) are associated with higher rates of intermediate probability scans, and when present, it is appropriate to let the ordering clinician know of this limitation.