Testicular Torsion
Karen M. Horton
George P. Kuo
Testicular torsion is a surgical emergency. Infarction can occur as soon as 4 hours after the onset of symptoms; however, if the degree of torsion is low, the testes can stay viable for as long as 24 hours. In general, surgical intervention within 6 hours of the onset of symptoms is preferred.
Etiology and Epidemiology.
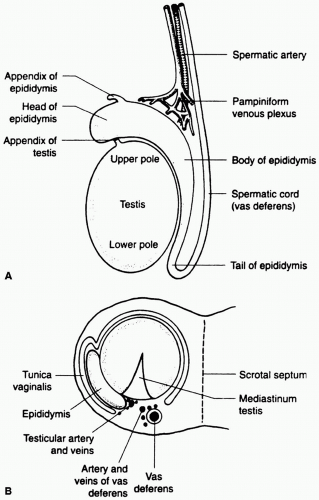
The normal testis (Fig. 46-1) is surrounded by the tunica vaginalis which is anchored posteriorly to the epididymis and scrotal wall. The testicular artery, the major blood supply to the testicle, runs in the spermatic cord. However, in some males, the tunica vaginalis surrounds the entire testis and inserts high on the spermatic cord. This anomaly is called a bell clapper deformity (Fig. 46-2) and predisposes to rotation of the testis within the tunica vaginalis, thereby twisting the spermatic cord and compromising blood flow to the testicle. Although testicular torsion can occur at any age, most cases occur in males around puberty (age 12-18). There is a second peak in early childhood.
Clinical History.
Acute onset of severe unilateral scrotal pain, often accompanied by nausea and vomiting. The pain can be referred to the lower abdomen or thigh. The vast majority of cases of testicular torsion occur spontaneously. History of possible precipitating events such as strenuous exercise or trauma is elicited in <5% of cases. There is sometimes a history of similar episodes in the past that are presumably related to previous torsion and spontaneous resolution.
Laboratory Studies.
Urinalysis almost always negative. There is usually no leucocytosis early on. Possible low-grade fever.
Physical Examination.
Early on, the testis is firm and often located high within the scrotal sac. The epididymis is usually not located in its usual posterior position, unless the testicle has torsed 360 or 720 degrees. Later, the hemiscrotum swells and becomes erythematous. If not diagnosed and surgically corrected, torsion leads to ischemic necrosis and atrophy of the testicle. The unaffected testis may be positioned transversely within the scrotum, indicating a bell clapper deformity.
Differential diagnosis of acute scrotal pain includes testicular torsion, torsion of the testes appendage (müllerian duct remnant), epididymitis, orchitis, and less commonly incarcerated inguinal hernia, vasculitis, and tumor. Testicular torsion and torsion of the appendage testes account for more than 90% of cases of acute onset of scrotal pain in the appropriate age group. Epididymitis and orchitis are the most common causes of painful scrotal swelling in an adult and are typically gradual in onset and accompanied by fever, urethral discharge, urinary tract symptoms, and a positive urinalysis. They typically result from an ascending infection of the urinary tract, sexually transmitted disease in younger men, and prostatitis in older men.
Indications.
Ultrasonography is a fast, accurate, noninvasive imaging modality which allows direct visualization of the testicle and its blood flow. Sensitivity is 80-90% and specificity is 90-100%.